Abstract
Background: Talc is a component of oral drugs that acts as a binding and bulking agent and a lubricant for the active ingredients. Talc has been shown to be fibrogenic and can cause the formation of foreign body granulomas in the pulmonary interstitium, leading to talcosis.
Objective: To interpret the High-Resolution Computed Tomography (HRCT) findings of pulmonary talcosis.
Methods: The study was conducted in the Department of Radiodiagnosis and Imaging, GMC Srinagar, with five patients after obtaining ethical clearance from the institutional ethical committee.
Results: Our study elucidated the HRCT pattern of pulmonary talcosis and highlighted the importance of recognizing talc as a potential cause of pulmonary fibrosis.
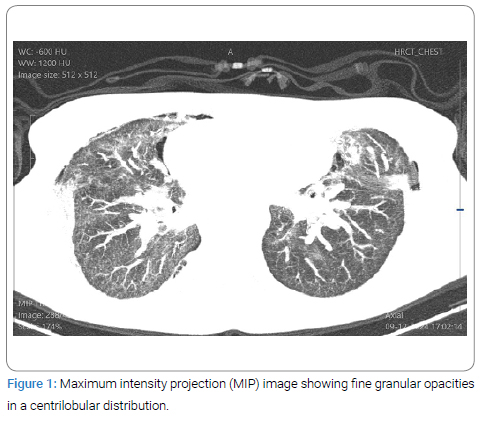
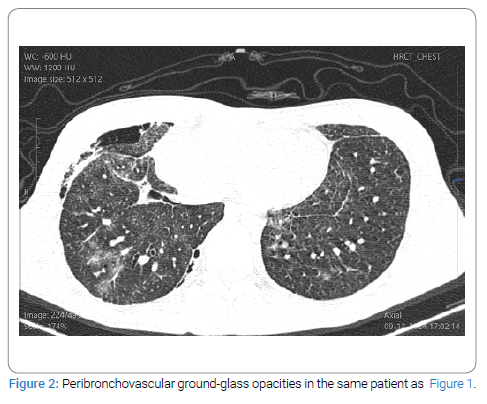
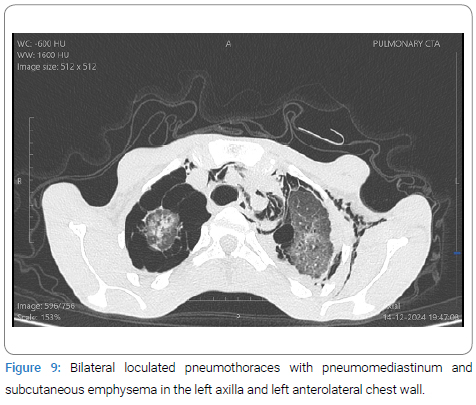
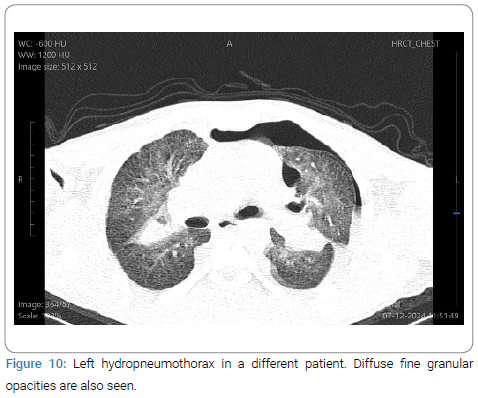
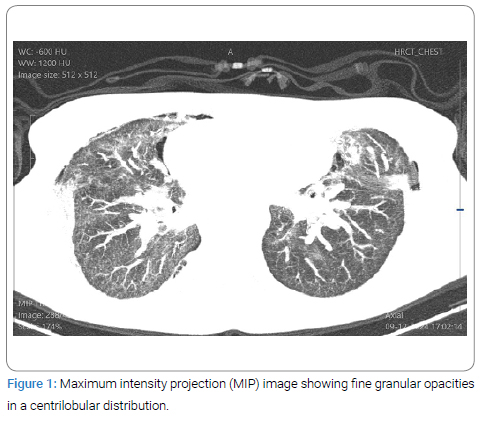
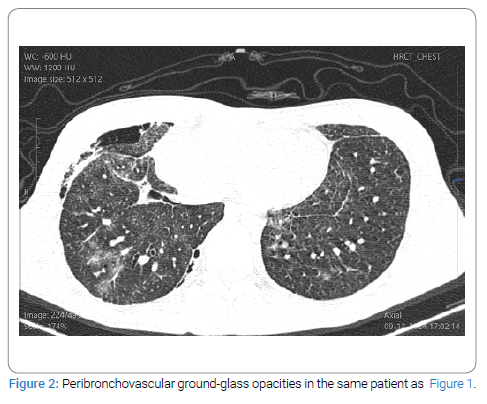
Conclusion: The most frequent findings included diffuse fine granular opacities (centrilobular distribution) and diffuse peribronchovascular ground-glass opacities, often accompanied by pneumothorax.
Introduction
Pulmonary Talcosis (A Rare Pneumoconiosis): We present five cases of intravenous drug abusers who injected medications intended for oral use. These patients were admitted to our hospital with complaints of shortness of breath and chest pain. They prepared an aqueous solution of the powdered drug before injection. The patients were adolescent to young adult males, ranging in age from 19 years to 30 years.
Chemically, talc is magnesium silicate [Mg3Si4O10(OH)2]. It is a component of oral medications, serving as a binding and bulking agent and a lubricant for the active ingredients. Talc has been shown to be fibrogenic, forming foreign body granulomas in the pulmonary interstitium.
Pulmonary talcosis is classified into four types: three inhalational forms (talco-silicosis, talco-asbestosis, and pure talcosis) and one intravenous form. The inhalational and intravenous forms share similar HRCT chest findings, except for the presence of emphysema (predominantly panacinar in the lower lobes), which is more commonly associated with intravenous methylphenidate (Ritalin) abuse. The inhalational forms differ based on the composition of the talc dust, which may also contain silica or asbestos.
Case Series
Case 1: A 24-year-old male IV drug abuser presented with chest pain, shortness of breath, and cyanosis.
HRCT of the chest revealed:
- Diffuse fine granular opacities (Figure 1).
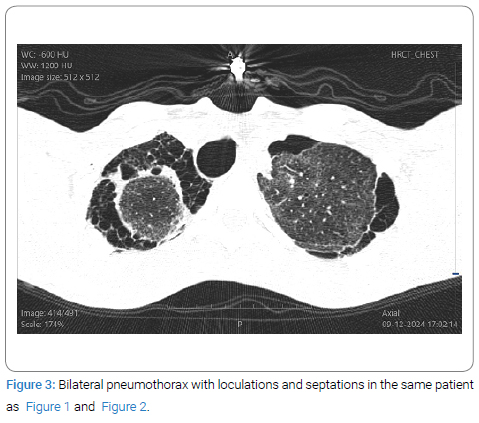
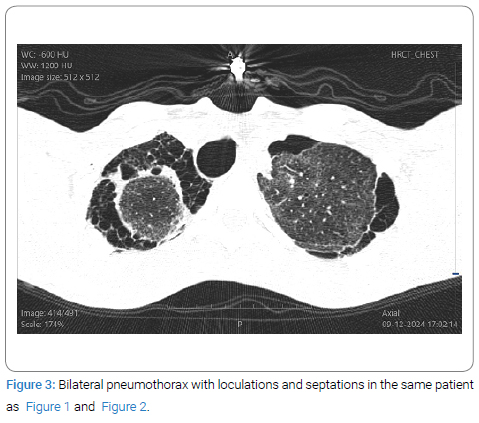
- Diffuse peri broncho vascular ground-glass opacities (Figure 2,Figure 3).
- Barotrauma-like features, including loculated pneumothorax (Figure 3).
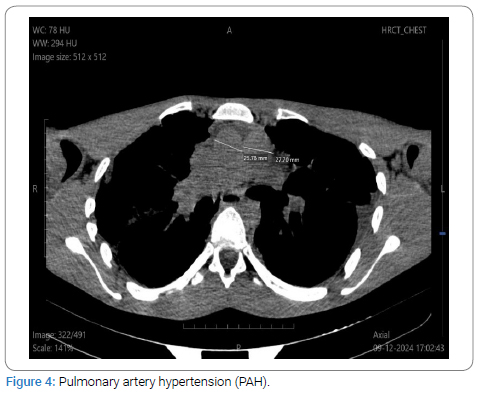
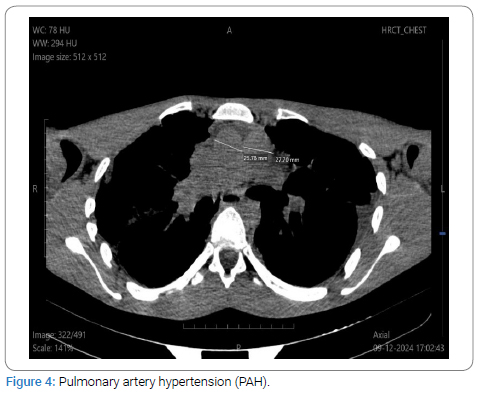
- Pulmonary artery hypertension (Figure 4).
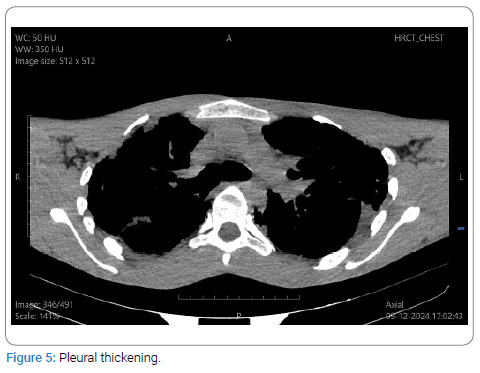
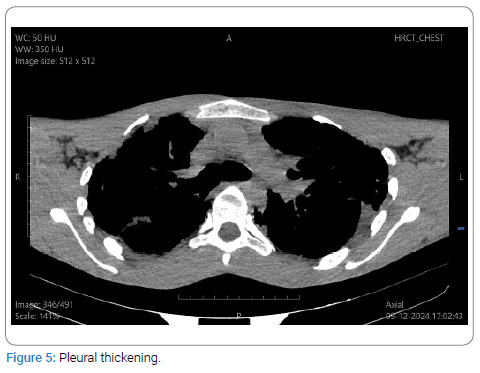
- Smooth pleural thickening (Figure 5).
Case 2: A 27-year-old male IV drug abuser presented with a fever for the past two months and shortness of breath.
HRCT of the chest revealed:
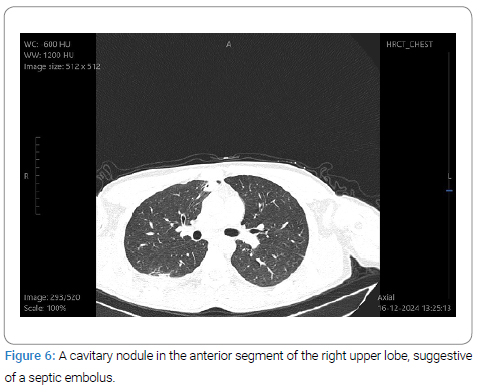
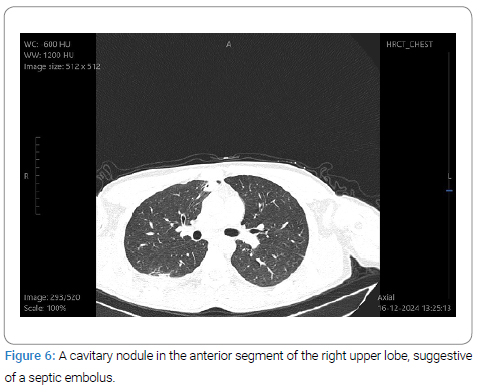
- A few randomly distributed cavitary nodules suggest septic emboli (Figure 6).
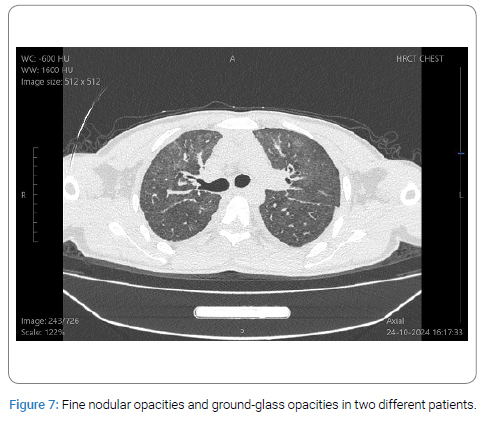
Case 3: A 19-year-old male IV drug abuser presented with chronic shortness of breath.
HRCT of the chest revealed:
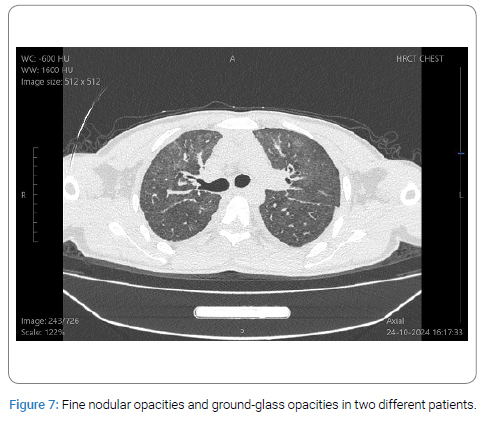
- Diffuse fine granular opacities and peri broncho vascular ground-glass opacities (Figure 7).
- Pulmonary artery hypertension.
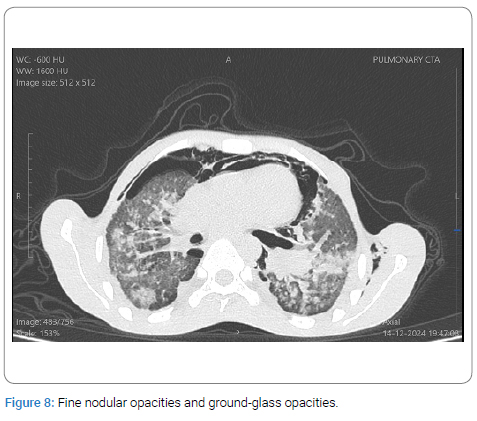
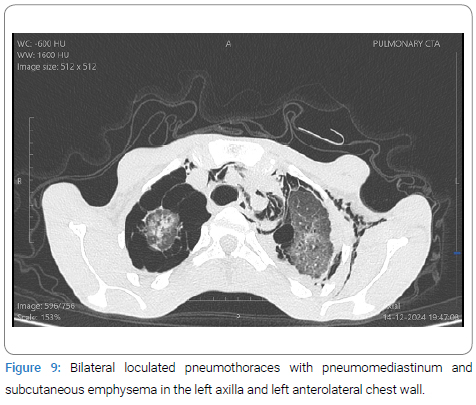
Case 4: A 19-year-old male IV drug abuser presented with acute chest pain and subcutaneous emphysema.
HRCT of the chest revealed:
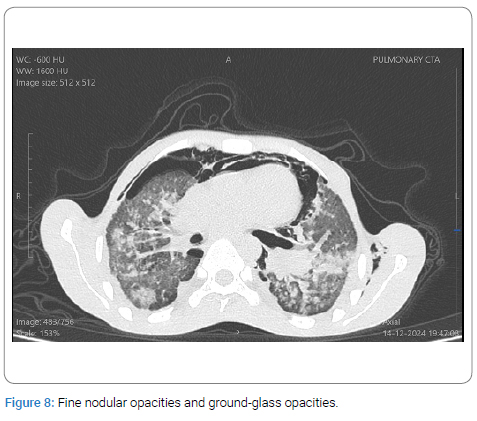
- Diffuse fine granular opacities and peri broncho vascular ground-glass opacities (Figure 8).
- Barotrauma-like features of pneumothorax, pneumomediastinum, and subcutaneous emphysema in the anterolateral chest wall, axilla, and neck (Figure 9).
- Pulmonary hypertension.
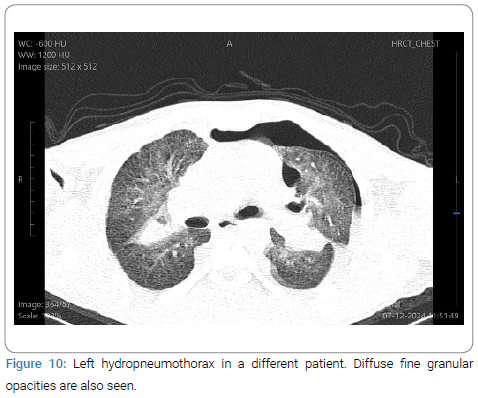
Case 5: A 30-year-old male IV drug abuser presented with acute chest pain and shortness of breath.
HRCT of the chest revealed:
- Diffuse fine granular opacities (Figure 10).
- Peribronchovascular ground-glass opacities.
- Barotrauma in the form of left hydropneumothorax.
- Features of pulmonary hypertension.
Discussion
Note that the most frequent High-Resolution Computed Tomography (HRCT) chest findings included a diffuse micronodular pattern, ground-glass opacities, heterogeneous conglomerate masses with areas of high attenuation, and pan-lobular emphysema in the lower lobes [1]. Interestingly, our patients did not exhibit emphysema (centriacinar or panacinar) or evidence of Progressive Massive Fibrosis (PMF).
Our study revealed that the most frequent findings were diffuse fine granular opacities (<1 mm, in centrilobular distribution) and diffuse peribronchovascular ground-glass opacities. The latter was more prominent, possibly due to the fine granular opacities being below the resolution of the CT scanner.
Demonstrated that a comprehensive medical history, including past exposures, can prevent delays in diagnosis and treatment that may be harmful to patients [2,3].
Reported imaging patterns consist of a fine micronodular pattern, conglomerate parahilar masses on a background of micronodularity, ground-glass attenuation, and emphysema [4].
Described an insidious imaging pattern mimicking primary lung cancer, with solitary lung lesions and mediastinal lymphadenopathy, showing intensive uptake on 18F-FDG PET/CT [5].
Our patients frequently exhibited barotrauma-like features, including pneumothorax, pneumomediastinum, and subcutaneous emphysema in the anterolateral chest wall, axilla, and neck. However, none had a significant history of trauma, suggesting that the pneumothoraxes were spontaneous. They also demonstrated loculated and septated pneumothorax, likely due to long-standing barotrauma.
The barotrauma may be explained by an alveolar rupture with air dissecting into the mediastinum or by injection of the drug into the supraclavicular fossa (the so-called ‘pocket shot’), which can lead to pneumothorax [6].
Pulmonary artery hypertension was a common finding, characterized by dilated main pulmonary arteries and a pulmonary artery-to-ascending aorta ratio >1.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Talcosis; Talc; Pneumothorax; Ground-glass opacities; Pulmonary hypertension
Cite this article
Mittal K, Hakeem AA. High-resolution computed tomography chest findings in IV opioid abusers. Clin Surg J. 2025;6(1):1–4.
Copyright
© 2025 Aijaz Ahmad Hakeem. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).