Diverting Ileostomy in Rectal Cancer: Associated Morbidity and Delay in Reconstruction Times
* Manuel González Bermúdez;
María Lourdes García Jiménez;
Javier Aguirrezabalaga González;
Jose Francisco Noguera Aguilar;
-
* Manuel González Bermúdez: General and Digestive Surgery Service, Complejo Hospitalario Universitario A Coruña, Spain.
-
María Lourdes García Jiménez: General and Digestive Surgery Service, Complejo Hospitalario Universitario A Coruña, Spain.
-
Javier Aguirrezabalaga González: General and Digestive Surgery Service, Complejo Hospitalario Universitario A Coruña, Spain.
-
Jose Francisco Noguera Aguilar: General and Digestive Surgery Service, Complejo Hospitalario Universitario A Coruña, Spain.
-
May 08, 2023 |
-
Volume: 4 |
-
Issue: 1 |
-
Views: 2508 |
-
Downloads: 1761 |
Abstract
Introduction: Rectal cancer treatment is being developed in many different ways, and the surgical one is probably breaking new ground. This is why we talk about sphincter-sparing surgery and the subsequent suggestive rise of diverting ileostomies. However, despite this fact, this approach has a considerable weakness which is usually underestimated.
Besides, reconstruction standards are not completely clear, and some published studies show evidence of increased complications and worse functional repercussions due to delayed times.
Objective: Not only discern the most real actuality of patients with ileostomies and define in a clear way the different complexities but also closing times and the certain analysis of all those circumstances it is influenced by.
Methods: Retrospective cohort study included patients operated on for rectal adenocarcinoma with diverting ileostomy between 2015 and 2019.
Results: There have been a total of 144 complications distributed in 106 of the 174 patients (61%), causing: 43 urgency admissions, 16 hospital admissions, 2 ICU admissions, and three surgical interventions prior to stomal reconstruction.
The median time up to stoma closure has been 10.2 months.
On the whole, neoadjuvant treatment, complications in the first surgery, adjuvant treatment, and ASA III–IV are the most important points associated with increased reconstruction time.
Moreover, 13.8% of registered patients have not been reconstructed by reason of death, progression, or anastomosis narrowing.
Conclusions: Diverting ileostomy presents considerable aggravations associated, and it is our commitment to take them into account every moment we indicate it.
As a result of clinical repercussions and health care costs associated with reconstruction of intestinal transit should be promoted as soon as possible.
Abbreviations
PO: Postoperative; AL: Anastomotic Leakage
Introduction
According to the latest SEOM review, colorectal cancer is the most incident one if we count both sexes together, being the rectal type 30% of them [1]. The last published studies reference a younger debut [2,3]. In addition to this, technological advances and neoadjuvant treatments [4,5] improvement are the main reasons for the increased use of the sphincter-preserving technique in down tumors and subsequent high risk of dehiscence [6,7].
Notwithstanding, diverting ileostomies is part of other different resources we use to avoid dehiscence effects [8].
Separated from its benefits, ileostomies bring a considerable aggravation development associated with the stoma, which carries deteriorated life quality by itself [9,10]. Even so, many of them will never be reconstructed [11], especially because of waiting lists and adjuvant oncological therapies. This is why the recommended times for reconstruction can not be on time [12].
Resources could be affected by this in postsurgical complications after stomal closure [13] and, without a doubt, functional results [14].
We have already worked on this in order to know about the de real situation of patients and define all the difficulties associated with ileostomies and their reconstruction times.
Material and Methods
It is a retrospective cohort study including patients operated on between 2015–2021 for rectal tumors associated with a programmed diverting ileostomy in the health area of A Coruña, Spain.
A surgical database was searched to identify data from patients who received a low anterior resection with total or partial mesorectal excision in patients with rectal cancer operated in the Department of Colorectal Surgery of the Hospital Universitario A Coruña, between January 1, 2015 and December 31, 2021.
We collected data on the patient, the tumor, the dates of the first intervention and the stomal closure, the morbidity associated with the stoma as well as different factors that, after reviewing the bibliography, we consider could be associated with an increase in the time’s reconstruction or even the absence of it.
Inclusion and Exclusion criteria: Patients with TNM Stage I to IV rectal cancer who underwent construction of a protective ileostomy at the time were included. Defunctioning ileostomies that were constructed in emergency surgery after an Anastomotic Leakage (AL) were excluded. Patients with diagnoses other than primary rectal adenocarcinoma, recurrent rectal cancer, previous local rectal surgery, or other kinds of stoma at their index surgery were also excluded.
Statistic analysis: It has been done with IBM SPSS version 25.0 for Macintosh.
Data are presented as proportions or as medians.
After verifying the absence of normal distribution of the variable time until reconstruction with the Kolmogorov-Smirnov test and Saphiro-Wilks (p < 0.05) for the analysis between qualitative and quantitative variables, a Mann Whitney U test was used for the analysis between 2 variables quantitative a Spearman correlation. For the analysis between categorical variables, we have used the Pearson Chi-square test with Yates correction. All statistical tests were 2-sided. Ap value of < 0.05 was considered statistically significant.
Results
Ileostomy indications: We have included 174 patients in our study. 67.8% were men with a median age of 68 years. The lower edge of the lesion has been found between 2 cm–15 cm from the anal margin, with 64.4% being locally advanced tumors that required neoadjuvant therapy. In addition, 57% have had to receive adjuvant chemotherapy due to definitive staging. Regarding the approach, 71.3% could be performed laparoscopically, requiring a combined TATME-type approach in 45.4% of cases.
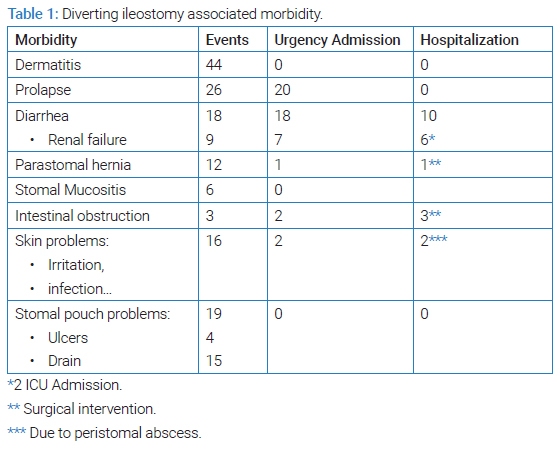
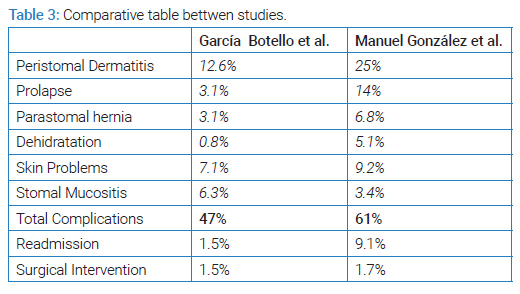
Morbidity: We have described a total of 144 complications distributed in 106 of the 174 patients (61%), these being those described in (Table 1).
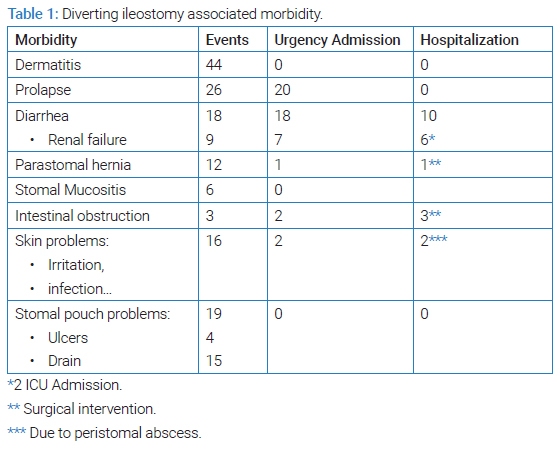
The most common complication has been peristomal dermatitis, followed by prolapses and pouch-related problems.
Causing 43 admissions to the Emergency Department, 16 hospital admissions, 2 ICU admissions, and three surgical interventions prior to stomal reconstruction.
Reconstruction times and factors associated with a late closure: We have found that the median time up to stoma closure has been 10.2 months (307 days), finding that 6.7% rebuild < 3 months, 10.1% 3 months–6 months, 46.9% 6–12, and 36.2% > 12 months.
The factors that have been associated in a statistically significant way with a delay in reconstruction times have been: neoadjuvant treatment (p = 0.02), complications first surgery (p = 0.02), adjuvant treatment (p < 0.01), ASA III-IV (p = 0.02).
Neither Sex (p = 0.53), ileostomy morbidity (p = 0.82), disease control (p = 0.82), or age (p = 0.82) have presented a statistically significant association with the closing time.
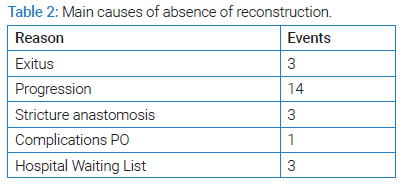
Absence of reconstruction causes and risk factors: Reconstruction has never been achieved in 13.8% of registered patients. The causes are those described in (Table 2).
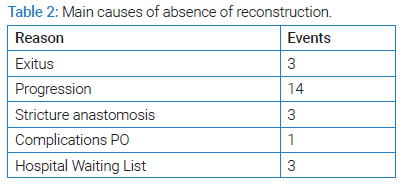
In addition, there have been factors such as being male (RR = 2.7, p < 0.05) or complications in the immediate Postoperative (PO) period (RR = 2.5, p < 0.05) that have been associated in a statistically significant way with a risk increased for no stomal reconstruction.
Discussion and Conclusions
According to studies results made with European and whole world population bases, rectal tumors appearance is evidenced in earlier aged [2,3]. This is conducted in an important change in patient profile, which can be integrated with technological advances. Tumor’s answer to neoadjuvant treatment [4,5,15] is the main reason for the increased use of sphincter-preserving techniques in down tumors.
The decrease in the height of the anastomosis is known as one of the risk factors for dehiscence in the PO rectal surgery [6,7]. Furthermore, the consequences of AL in colorectal cancer surgery, with the consequent appearance of PO sepsis and worse oncological results, are described in the literature [16,17].
Surgeons used different stunts in order to avoid AL or, at least, reduce its appearance [8]. One of the most established techniques is the diverting stomas [8], ileostomy being the most recommended one according to most recent publications [18,19].
Its indications by this moment are not totally defined. Despite this, there is enough support to perform it in patients with anastomosis ubicated six or fewer centimeters close to the anal margin or even in patients with anastomosis between six and eight centimeters with more than one risk dehiscence factor [20].
So far, there’s not enough evidence to confirm that this technique reduces the occurrence of fistula in the PO. However, it can mitigate its consequences, although the evidence supporting these findings is still weak [21–23].
As Nasir Zaheer et al. concluded in their meta-analysis, ileostomies will bring with them a percentage of morbidity associated with the stoma itself, regardless of its benefits [9]. This morbidity is often underdiagnosed [10], so its use should be reserved for those patients who really need it. 61% of the patients included in our study have presented some type of morbidity in relation to their stoma. Although it’s true that the most frequent complications have been trivial, such as dermatitis or prolapse, there have been others, such as renal failure or the incarceration of a parastomal hernia, that can cause to require hospital admission up to 16 times (2 of them in the ICU) or surgical intervention in 3 of our cases. In addition, there were 43 visits to the Emergency Department due to problems derived from the ostomy, which worsens the patient’s quality of life and also increases healthcare costs.
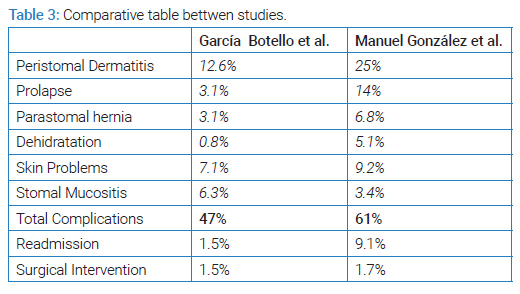
In the article published in 2004 by García Botello et al. [10], an associated morbidity of 40% has been evidenced, with the order of frequency of appearance of each complication being similar to that presented in our publication (Table 3).
Another topic under discussion is what is considered the optimal moment for stomal reconstruction. There are groups that advocate early closure, more or less ten days after the intervention, and others recommend late closure, which should be around 3-4 months [24,25]. However, a recent retrospective study on 788 patients has been published. Its authors concluded that the delay in stomal reconstruction was common, presenting a median time to closure of 259 days, far exceeding the 90–120 recommended by the current literature [12].
In our Health Area, we have shown how the times until stomal closure even exceeded those described in the CLOSE-IT study. A median of 307 days was demonstrated, and a statistically significant relationship was found between cancer treatments and ASA III–IV with this delay. These results represent a difference from what was published in the Dukes Club Research Collaborative study [12], where AL and the progression of the oncological disease were described as factors.
This delay in the closure of the stoma will cause a longer time for defunctionalization of the digestive tract, resulting in atrophy of the colonic mucosa and sphincters that may increase the appearance of Low Anterior Resection Syndrome (LARS), as has been published in the 2021 meta-analysis [14]. Furthermore, in this study, Vogel et al. showed that this delay could cause a worsening of long-term functional results [14].
T.H. Kwoo et al., in their retrospective study, conclude that a delay in reconstruction of more than six months can be associated with an increase in PO complications [13]. As we can see in our results, 84.5% of the patients will undergo reconstruction after this time, which could explain the almost 30% of complications in PO that we have been able to record. These complications could be minimized by reducing closure times or with prehabilitation programs for the efferent loop [26].
Finally, as Hong Da Pan et al. described in their prospective study, approximately 1 out of 6 patients will never undergo reconstruction [11]. These same findings have been evidenced in our study, also coinciding that the main reasons for this absence of reconstruction to have been: death, disease progression, or problems with colorectal anastomosis.
As a limitation, the results of the times until closing have been influenced by the increase in waiting lists secondary to the pandemic; however, these waiting list times were similar in previous years. Also, this study has limitations related to retrospective data collection, as well as the fact that it was a single-center study. In addition, the statistical analysis has been carried out with non-parametric tests.
Despite the limitations, we believe that the results obtained demonstrate a current problem, which possible solutions and alternatives should be studied.
This research has no conflict of interest and has not received any specific grants from agencies in the public, commercial, or non-profit sectors.
In conclusion, the diverting ileostomy presents considerable associated morbidity that we must take into account when indicating its performance. Therefore, the recommendations regarding its reconstruction are very difficult to carry out. Nevertheless, due to the clinical repercussions and the associated healthcare costs, intestinal transit reconstruction should be promoted as soon as possible or, failing that, the use of a continuity solution that serves as a bridging treatment until definitive closure is achieved.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- SEOM. Sociedad española de oncología médica [Internet]. Madrid: SEOM; 2022.
- Araghi M, Soerjomataram I, Bardot A, Ferlay J, Cabasag CJ, Morrison DS, et al. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol. 2019;4(7):511–518.
- Vuik FE, Nieuwenburg SA, Bardou M, Lansdorp-Vogelaar I, Dinis-Ribeiro M, Bento MJ, et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut. 2019;68(10):1820–1826.
- Conroy T, Bosset JF, Etienne PL, Rio E, François É, Mesgouez-Nebout N, et al; Unicancer Gastrointestinal Group and Partenariat de Recherche en Oncologie Digestive (PRODIGE) Group. Neoadjuvant chemotherapy with FOLFIRINOX and preoperative chemoradiotherapy for patients with locally advanced rectal cancer (UNICANCER-PRODIGE 23): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(5):702–715.
- Bahadoer RR, Dijkstra EA, van Etten B, Marijnen CAM, Putter H, Kranenbarg EM, et al; RAPIDO collaborative investigators. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(1):29–42.
- Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM, et al. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018;24(21):2247–2260.
- Vasiliu ECZ, Zarnescu NO, Costea R, Neagu S. Review of risk factors for anastomotic leakage in colorectal surgery. Chirurgia (Bucur). 2015;110(4):319–226.
- Meyer J, Naiken S, Christou N, Liot E, Toso C, Buchs NC, et al. Reducing anastomotic leak in colorectal surgery: The old dogmas and the new challenges. World J Gastroenterol. 2019;25(34):5017–5025.
- Ahmad NZ, Abbas MH, Khan SU, Parvaiz A. A meta-analysis of the role of diverting ileostomy after rectal cancer surgery. Int J Colorectal Dis. 2021;36(3):445–455.
- García-Botello SA, García-Armengol J, García-Granero E, Espí A, Juan C, López-Mozos F, et al. A prospective audit of the complications of loop ileostomy construction and takedown. Dig Surg. 2004;21(5–6):440–446.
- Pan HD, Peng YF, Wang L, Li M, Yao YF, Zhao J, et al. Risk factors for nonclosure of a temporary defunctioning ileostomy following anterior resection of rectal cancer. Dis Colon Rectum. 2016;59(2):94–100.
- Dukes’ Club Research Collaborative. Factors impacting time to ileostomy closure after anterior resection: the UK closure of ileostomy timing cohort study (CLOSE-IT). Colorectal Dis. 2021;23(5):1109–1119.
- Khoo TW, Dudi-Venkata NN, Beh YZ, Bedrikovetski S, Kroon HM, Thomas ML, et al. Impact of timing of reversal of loop ileostomy on patient outcomes: a retrospective cohort study. Tech Coloproctol. 2021;25(11):1217–1224.
- Vogel I, Reeves N, Tanis PJ, Bemelman WA, Torkington J, Hompes R, et al. Impact of a defunctioning ileostomy and time to stoma closure on bowel function after low anterior resection for rectal cancer: a systematic review and meta-analysis. Tech Coloproctol. 2021;25(7):751–760.
- Cercek A, Lumish M, Sinopoli J, Weiss J, Shia J, Lamendola-Essel M, et al. PD-1 Blockade in mismatch repair-deficient, locally advanced rectal cancer. N Engl J Med. 2022;386(25):2363–2376.
- Wang S, Liu J, Wang S, Zhao H, Ge S, Wang W. Adverse effects of anastomotic leakage on local recurrence and survival after curative anterior resection for rectal cancer: a systematic review and meta-analysis. World J Surg. 2017;41(1):277–284.
- Ha GW, Kim JH, Lee MR. Oncologic impact of anastomotic leakage following colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg Oncol. 2017;24(11):3289–3299.
- Chudner A, Gachabayov M, Dyatlov A, Lee H, Essani R, Bergamaschi R. The influence of diverting loop ileostomy vs. colostomy on postoperative morbidity in restorative anterior resection for rectal cancer: a systematic review and meta-analysis. Langenbecks Arch Surg. 2019;404(2):129–139.
- Du R, Zhou J, Tong G, Chang Y, Li D, Wang F, et al. Postoperative morbidity and mortality after anterior resection with preventive diverting loop ileostomy versus loop colostomy for rectal cancer: A updated systematic review and meta-analysis. Eur J Surg Oncol. 2021;47(7):1514–1525.
- Plasencia A, Bahna H. Diverting ostomy: for whom, when, what, where, and why. Clin Colon Rectal Surg. 2019;32(3):171–175.
- Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H; Working Group ‘Colon/Rectum Carcinoma’. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg. 2005;92(9):1137–1142.
- Nurkin S, Kakarla VR, Ruiz DE, Cance WG, Tiszenkel HI. The role of faecal diversion in low rectal cancer: a review of 1791 patients having rectal resection with anastomosis for cancer, with and without a proximal stoma. Colorectal Dis. 2013;15(6):e309–e316.
- Veenhof AAFA, van der Peet DL, Meijerink WJHJ, Cuesta MA. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2008;247(4):718–719.
- Lasithiotakis K, Aghahoseini A, Alexander D. Is Early reversal of defunctioning ileostomy a shorter, easier and less expensive operation? World J Surg. 2016;40(7):1737–1740.
- Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E. Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg. 2008;95(6):693–698.
- Ocaña J, García-Pérez JC, Labalde-Martínez M, Rodríguez-Velasco G, Moreno I, Vivas A, et al. Can physiological stimulation prior to ileostomy closure reduce postoperative ileus? A prospective multicenter pilot study. Tech Coloproctol. 2022;26(8):645–653.
Keywords
Diverting ileostomy; Rectal cancer; Reconstruction; Morbidity; Low anterior resection syndrome
Cite this article
M González-Bermúdez, ML García-Jiménez, J Aguirrezabalaga-González, JF Noguera-Aguilar. Diverting ileostomy in rectal cancer: associated morbidity and delay in reconstruction times. Clin Surg J. 2023;4(1):1–5.
Copyright
© 2023 Manuel González Bermúdez. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).