An Update on the Success Rate of the Zygomatic Implant in Orofacial Reconstructive Surgery: A 20 Years Systematic Review
* Heron Gezahegn Gebretsadik;
-
* Heron Gezahegn Gebretsadik: Department of Oral and Maxillofacial Surgery, School of Global Health & Bioethics, Euclid University, Gambia.
-
Jan 30, 2023 |
-
Volume: 4 |
-
Issue: 1 |
-
Views: 5756 |
-
Downloads: 2072 |
Abstract
Zygomatic implants are reportedly effective in replacing lost teeth and Orofacial soft and hard tissue configuration. The prime goal of this systematic review is to update the survival rate of zygomatic implants. The initial systematic review was carried out in November 2019. In this updated review, articles published between December 2019 and October 2022 were retrieved from PubMed, ISI Web of Science, Cochrane, and Google Scholar databases. The comprehensive electronic search in both systematic reviews yielded 81 relevant articles for data analysis. A total of 6628 bilateral double (quad) and single zygomatic implants were placed to restore Orofacial configuration in 2913 patients. That means an average of 2.3 implants were placed in a single patient. A 94.9% (n = 6290) cumulative success rate of the zygomatic implant was calculated in this updated review after an average follow-up period of 3.1 years. Peri-implantitis and prosthetic-related complications are the leading causes of zygomatic implant failure.
In this review a lower success rate is calculated in a relatively shorter follow-up period time compared to the initial systematic review (success rate of 96.7% after an average follow up period of 3.5 years). This shows that randomized control trials with more extended follow-up periods need to be conducted to ascertain the predictability of zygomatic implants in reconstructing the Orofacial complex. Clinical practice based on short-term outcome studies should also be cautioned.
Abbreviations
ISI: The Institute for Scientific Information; MeSH: Medical Subject Headings; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; CASP: Critical Appraisal Skills Programme; SPSS: Statistical Package for the Social Sciences
Introduction
Dental implants are commonly used in dental practices to restore aesthetic and oral functions [1]. Reports revealed a high success rate of conventional dental implants [2]. Similarly, pterygoid implants have demonstrated a high success profile in patients with the atrophic posterior maxilla {Citation}. However, conventional and pterygoid dental implants have limitations in treating patients presenting with tumor resection and trauma-induced severe maxillary bone deficits [3,4]. In this case, zygomatic implants are reportedly a viable option [3]. Zygomatic implants are anchored to the cheekbone [5]. Different surgical techniques have evolved since the introduction of the zygomatic implant by Swedish scientist Per-Ingvar Brånemark in the 1990s [4–7]. Still, treating significant maxillary atrophy with a zygomatic implant is challenging [8]. The procedure may demand bone grafting and raising micro vascularized flaps, which require a lengthy healing time that can increase patients’ morbidity due to pain. The anatomical complexity of the region is the other challenge of installing zygomatic implants [9,10]. Insufficient maxillary ridge volume/severe maxillary ridge atrophy is the other major challenge in reconstructing the Orofacial apparatus. Moreover, the surgical placement of a zygomatic implant to reconstruct an Orofacial defect is associated with varying degrees of biological and prosthetic complications, including sinusitis, Schneiderman membrane penetration, and implant fracture [1,2,11].
Nevertheless, various surgical approaches have evolved to treat these and other challenging conditions [12,13]. Placing angled implants in the para-sinus region, elevating the maxillary sinus floor with a bone substitute or graft, grafting iliac bone to increase bone volume, and installing implants in pterygoid apophysis are some of these approaches [14–19]. Zygomatic implant placement does not require adjunctive procedures such as intra or extra-oral bone harvesting [3,20]. Using a zygomatic implant reduces treatment costs, patient morbidity, the risk of developing surgical complications, and the likelihood of prolonged hospitalization [21]. Therefore, zygomatic implants are reported to be an acceptable modality to patients treat patients with severe maxillary deficits [22]. Zygomatic implants can be placed unilaterally or bilaterally, depending on the clinical indication. Accordingly, one or two zygomatic implants can be installed on each side of the zygomatic buttresses [11,23–25]. General anesthesia or intravenous sedation may need to administer to surgically attach zygomatic implants to zygomatic bone [7,13,16,26–28]. Various studies reported predictable long-term clinical outcomes of conventional implants in restoring aesthetic and oral functions [14,29–31]. But, conventional implants have limitations regarding treating patients with inadequate maxillary bone quantity [14,22,32]. The introduction of zygomatic implants has reportedly filled this gap [4]. Yet, reports on the success rate of zygomatic implants remained scarce. In this regard, a systematic review aimed at assessing the success rate of zygomatic implants in Orofacial reconstructive surgery was conducted in November 2019. The study reported a 97.6% success rate of zygomatic implants [33]. Yet, the success rate may not remain the same over time. Therefore, the present study aimed to update the success rate of the zygomatic implant by including the latest publications.
Materials and Methods
Study design: A systematic review of the literature was conducted in November 2022 to update the success rate of the zygomatic implants in Orofacial reconstruction.
Search strategy: This review searched for potentially relevant articles published between December 2019 and November 2022. The search was conducted on PubMed, ISI (The Institute for Scientific Information) Web of Science, Cochrane, and Google Scholar databases. The bibliographic software EndNote (Thomson Reuters Corp., New York City, NY, United States of America) was used to manage all retrieved references. The search strategy began with an initial electronic search to obtain the first raw hits from the databases mentioned above. From the initial raw hits, some literature was excluded as duplicates by Endnote and manual duplicate search strategies. Identifying potentially relevant articles was followed by assessing the title and/or abstract contents. These identified papers further underwent a full-text review. The full texts were accessed through EndNote full-text search, URL search, google search, and University’s library sources. After in-depth reading of the entire full texts available and conducting rigorous CASP (Critical Appraisal Skills Programme) analysis, the final articles were selected for data analysis. Only peer-reviewed articles written in English were included.
The systematic review adhered to the principles of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (2020). The keywords zygoma, zygomatic, zygomaticus implants, zygomatic dental implants, Jawsurgery, maxilla surgery, zygoma surgery, and zygomaticus were used as Subjects. Furthermore, terms such as zygomatic implant survival rate, success rate, and failure rate were used to retrieve relevant articles for data analysis. In particular, these terms were used as MeSH (Medical Subject Headings) to search the PubMed database.
{Subject AND Adjective}
{Subject: (zygomatic OR zygoma OR zygomaticus [Title])
AND
Adjective: (implant OR implants OR fixture OR fixtures [Title])}
CASP analysis was used to assess the quality of the articles selected for data analysis.
Inclusion criteria:
- Articles focused on the human zygomatic implant.
- Article’s medium of language: English.
- All articles, except for systematic review and meta-analysis (to avoid double-counting), on the abovementioned databases between December 2019 and October 2022.
- Cohort post-surgical follow-up of a minimum of 6 months.
- Cohorts control for other systemic diseases and congenital abnormalities that can confound the outcome.
- All articles reporting survival data of zygomatic implant.
Screening and selection of the literature: PubMed, ISI Web of Science, Cochrane, and Google Scholar databases were initially searched for pertinent articles. The review’s rigorous screening and selection phase started after identifying the first raw hits. From the initial raw hits, some literature was excluded as duplicates by Endnote and manual duplicate search strategies. Of these, a specific number of potentially relevant articles were selected based on the Title and/or abstract vicinity to the study subject. Eventually, the literature underwent full-text scrutiny and CASP analysis to identify the final articles for data analysis.
Extraction of data: A predesigned data extraction template was used to extract and store useful clinical information for data analysis. This clinical information was used as a core input to calculate the success rate of the zygomatic implants, which was the central aim of this review.
Data analysis: The compiled clinical data in the data extraction template was analyzed using the SPSS (Statistical Package for the Social Sciences) statistical software. Simple algebra was also used as needed to facilitate the data extraction process.
Ethical clearance: Not applicable.
Findings: This section primarily presented the database search results and the updated success rate of zygomatic implants.
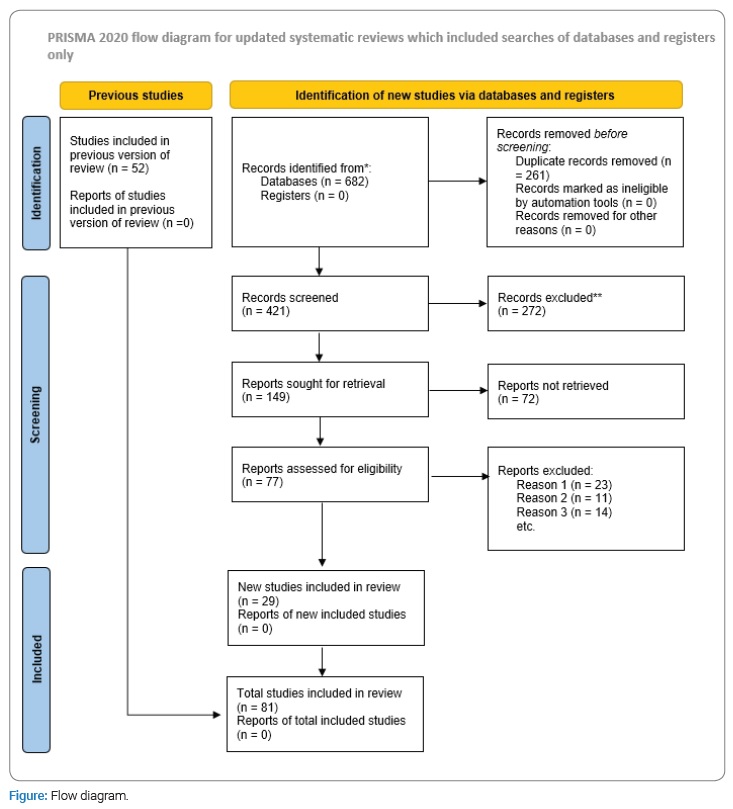
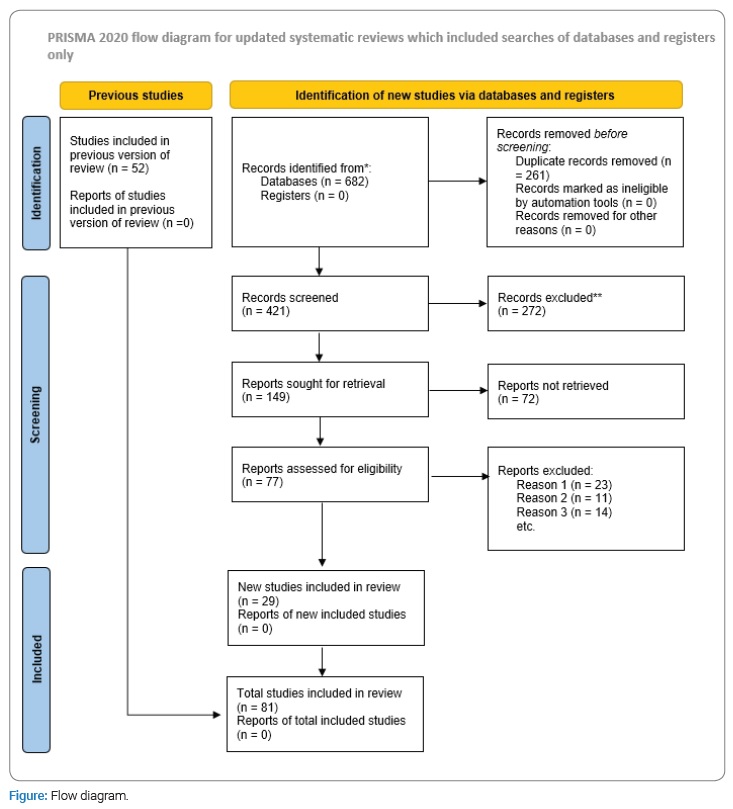
Databases search result: A total of 682 articles were identified after the initial electronic search in this updated review. Of these, 261 papers were duplicated and excluded by EndNote duplicate search (249) and Manual duplicate search (12) strategies. Of those 421 remaining articles, 149 were considered relevant based on their Title and/or abstract. After a full-text review, 77 articles were assessed for eligibility. Nevertheless, only 29 were finally selected for data extraction (Figure).
Result of CASP analysis: All 29 articles selected for data analysis underwent a CASP check. All of them were found to satisfy the core criteria of the CASP analysis.
Updated success/survival rate of zygomatic implants: A total of 6628 zygomatic implants were surgically placed in 2913 study participants. In other words, approximately 2.3 zygomatic implants were installed in a single patient. In general, the survival rate of the zygomatic implant in this updated long-term study was calculated to be 94.9% (n = 6290) after a mean follow-up period of 3.1 years. Therefore, this updated review revealed a lower success rate in a relatively shorter follow-up period compared to the initial study.
Discussion
Despite advancements in surgical technique, including bone grafting and sophisticated prosthetic reconstructions, there are limitations to what can be achieved with bone-anchored fixed prostheses in patients with advanced atrophy of the maxillae [27]. The introduction of zygomatic implants has been celebrated in the last two decades to overcome the challenge of treating patients with severe maxillary defects [6]. However, long-term success rate data is still being determined. This long-term (20-year) systematic review aims to report the cumulative success rate of zygomatic implants used in rehabilitating patients with severe maxillary defects. The systematic review included 81 articles for data analysis. A total of 6628 zygomatic implants were placed to restore Orofacial configuration in 2913 patients, meaning a mean of 2.3 implants were placed in a single patient. Accordingly, the cumulative success rate of zygomatic implants was calculated to be 94.9% after an average follow-up period of 3.1 years.
Similarly, other research works revealed a zygomatic implant success rate that ranges from 82% to 100% [34]. For instance, Parel et al. reported a 100% success rate for zygomatic implants after a 6-year follow-up [35]. Bedrossian et al. Revealed a 100% success rate after 34 months of follow-up [36]. Becktor et al. studied 16 patients who received 31 zygomatic implants over an average period of 46.4 months. This research team reported a zygomatic implant survival rate of 90.3% [32]. After a year of follow-up, a 97.9% success rate was reported by Hirsch et al. [18].
In the same way, Al-Nawas et al. and Chrcanovic et al. calculated 97% and 96.7% zygomatic implant success rates, respectively [5,37]. In other words, a considerable number of the literature disclosed the effectiveness and predictability of zygomatic implants in restoring Orofacial defects [30,38,39,40,41]. However, the surgical placement of zygomatic implants is not free from complications. Accordingly, several studies reported varying degrees of complications, such as sinusitis, oroantral opening, rhinosinusitis, soft-tissue dehiscence, zygomatic bone fracture, and intracranial penetration [19,42,43]. According to scholars, the anatomic complexity of the Orofacial region remained a major challenge for clinicians with limited experience in placing zygomatic implants [17,44–46]. As such, scientists underscore the importance of a thorough understanding of the anatomy of the zygoma, the biological fixture of the maxilla and maxillary sinus, and the biomechanical characteristics of the zygoma are crucial to coming up with excellent clinical outcomes. However, despite the anatomic complexity and the reported biological constraints and complications, clinicians and researchers praised the procedure for its high success rate [47]. The finding of this updated review and many other reports supports the above argument. For instance, an overview of systematic reviews that aimed to assess the quality of systematic reviews regarding the effectiveness of zygomatic implants reported a 96,7% success rate, which is more or less similar to the finding of this study [44]. Goker et al. Goiato et al. and Aparicio et al. also reported similar commutative success rates, which are comparable findings to this updated review [17,21,45]. In general, the results of this review and other studies suggested that the surgical placement of zygomatic implants is safe and reliable. The procedure is less invasive and more predictable than other bone grafting procedures, including sinus elevation. Moreover, the procedure is applicable in cases where autogenous bone cannot be harvested, and allograft may not be advisable for several reasons. However, it is worth enough to remind that the procedure is associated with severe complications, which, although rare, may jeopardize the outcomes of the treatment [34,48].
Conclusion
According to various reports, the success rates of zygomatic implants vary between 82% and 100%. Therefore, this updated systematic review’s findings also suit this category well. Thus, these findings support the argument that the placement of zygomatic implants to reconstruct Orofacial defects is a predictable approach. In other words, the surgical placement of zygomatic implants is a superior approach to treating severe Orofacial defects. However, the procedure is associated with considerable biological complications.
Furthermore, factors such as limited intraoperative visibility, the complexity of the anatomical structures, the anatomic proximity of delicate organs, and the intricacies of the zygomatic curve made the procedure a surgical skill demanding clinical practice. Therefore, the procedure should be carried out by highly skilled surgeons. Moreover, conducting clinical trials with longer follow-ups and larger study participants is essential to ascertain the long-term success rate of the procedure in reconstructing Orofacial deformities.
Acknowledgment
I want to express my profound appreciation to Dr. Ignacio Zapardiel and Dr. David Madruga for their valuable encouragement while writing the initial systematic review.
Conflict of Interest
The author declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- D’Agostino A, Lombardo G, Favero V, Signoriello A, Bressan A, Lonardi F, et al. Complications related to zygomatic implants placement: A retrospective evaluation with 5 years follow-up. J Cranio-Maxillofac Surg. 2021;49(7):620–627.
- Mavriqi L, Lorusso F, Conte R, Rapone B, Scarano A. Zygomatic implant penetration to the central portion of orbit: a case report. BMC Ophthalmol. 2021;21(1):121.
- Araujo RZ, Santiago Júnior JF, Cardoso CL, Condezo AFB, Júnior RM, Curi MM. Clinical outcomes of pterygoid implants: Systematic review and meta-analysis. J Craniomaxillofac Surg. 2019;47(4):651–660.
- Davó R, Malevez C, Rojas J, Rodríguez J, Regolf J. Clinical outcome of 42 patients treated with 81 immediately loaded zygomatic implants: a 12-to 42-month retrospective study. Eur J Oral Implantol. 2008;9 Suppl 1(2):141–150.
- Annibali S, Cristalli MP, Dell’Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review. J Dent Res. 2012;91(1):25–32.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and complications of zygomatic implants: an updated systematic review. J Oral Maxillofac Surg. 2016;74(10):1949–1964.
- Chow J, Wat P, Hui E, Lee P, Li W. A new method to eliminate the risk of maxillary sinusitis with zygomatic implants. Int J Oral Maxillofac Implants. 2010;25(6):1233–1240.
- Borgonovo A, Grandi T, Vassallo S, Signorini L. Extrasinus zygomatic implants for the immediate rehabilitation of the atrophic maxilla: 1-year postloading results from a multicenter prospective cohort study. J Oral Maxillofac Surg. 2021;79(2):356–365.
- Davó R, Bankauskas S, Laurincikas R, Koçyigit ID, Mate Sanchez de Val JE. Clinical performance of zygomatic implants—retrospective multicenter study. J Clin Med. 2020;9(2):480.
- Pellicer-Chover H, Cervera-Ballester J, Peñarrocha-Oltra D, Bagán L, Peñarrocha-Diago MA, Peñarrocha-Diago M. Influence of the prosthetic arm length (palatal position) of zygomatic implants upon patient satisfaction. Med Oral Patol Oral Cirugia Bucal. 2016;21(3):e380–e384.
- Yates JM, Brook IM, Patel RR, Wragg PF, Atkins SA, El-Awa A, et al. Treatment of the edentulous atrophic maxilla using zygomatic implants: evaluation of survival rates over 5-10 years. Int J Oral Maxillofac Surg. 2014;43(2):237–242.
- Aparicio C, Polido WD, Chow J, Davó R, Al-Nawas B. Round and flat zygomatic implants: effectiveness after a 1-year follow-up non-interventional study. Int J Implant Dent. 2022;8(1):13.
- Pellegrino G, Basile F, Relics D, Ferri A, Grande F, Tarsitano A, et al. Computer-aided rehabilitation supported by zygomatic implants: a cohort study comparing atrophic with oncologic patients after five years of follow-up. J Clin Med. 2020;9(10):3254.
- Wang F, Bornstein MM, Hung K, Fan S, Chen X, Huang W, et al. Application of real-time surgical navigation for zygomatic implant insertion in patients with severely atrophic maxilla. J Oral Maxillofac Surg. 2018;76(1):80–87.
- Bertolai R, Aversa A, Catelani C, Rossi A, Giannini D. Treatment of extreme maxillary atrophy with Zygoma implants. Minerva Stomatol. 2015;64(5):253–264.
- Fernández-Ruiz JA, Sánchez-Siles M, Guerrero-Sánchez Y, Pato-Mourelo J, Camacho-Alonso F. Evaluation of quality of life and satisfaction in patients with fixed prostheses on zygomatic implants compared with the all-on-four concept: a prospective randomized clinical study. Int J Environ Res Public Health. 2021;18(7):3426.
- Goker F, Grecchi F, Grecchi E, Bolzoni AR, Del Fabbro M. Insertion of zygomatic implants with a technical modification of the extrasinus protocol: a retrospective case series. Int J Oral Maxillofac Implants. 2020;35(5):974–981.
- Fernández H, Gómez-Delgado A, Trujillo-Saldarriaga S, Varón-Cardona D, Castro-Núñez J. Zygomatic implants for the management of the severely atrophied maxilla: a retrospective analysis of 244 implants. J Oral Maxillofac Surg. 2014;72(5):887–891.
- Hirsch J-M, Ohrnell L-O, Henry PJ, Andreasson L, Brånemark P-I, Chiapasco M, et al. A clinical evaluation of the Zygoma fixture: One year of follow-up at 16 clinics. J Oral Maxillofac Surg. 2004;62(9 Suppl 2):22–29.
- Vashisht R, Bhalla H, Prithviraj D. From maxilla to zygoma: A review on zygomatic implants. J Dent Implants. 2014;4:44.
- Rajan G, Natarajarathinam G, Kumar S, Parthasarathy H. Full mouth rehabilitation with zygomatic implants in patients with generalized aggressive periodontitis: 2-year follow-up of two cases. J Indian Soc Periodontol. 2014;18(1):107–111.
- Goiato MC, Pellizzer EP, Moreno A, Gennari-Filho H, dos Santos DM, Santiago Jr JF, et al. Implants in the zygomatic bone for maxillary prosthetic rehabilitation: a systematic review. Int J Oral Maxillofac Surg. 2014;43(6):748–757.
- Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: a 6-48 months follow-up study. Clin Oral Implants Res. 2004;15(1):18–22.
- Aparicio C, Manresa C, Francisco K, Aparicio A, Nunes J, Claros P, et al. Zygomatic implants placed using the zygomatic anatomy-guided approach versus the classical technique: a proposed system to report rhinosinusitis diagnosis. Clin Implant Dent Relat Res. 2014;16(5):627–642.
- Kuabara MR, Ferreira EJ, Gulinelli JL, Panzarini SR. Use of 4 immediately loaded zygomatic fixtures for retreatment of atrophic edentulous maxilla after complications of maxillary reconstruction. J Craniofac Surg. 2010;21(3):803–805.
- Maló P, de Araújo Nobre M, Lopes A, Ferro A, Moss S. Extramaxillary surgical technique: clinical outcome of 352 patients rehabilitated with 747 zygomatic implants with a follow-up between 6 months and 7 years. Clin Implant Dent Relat Res. 2015;17 Suppl 1:e153-e162.
- Brånemark P-I, Gröndahl K, Ohrnell L-O, Nilsson P, Petruson B, Svensson B, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70–85.
- Romeed SA, Malik R, Dunne SM. Zygomatic implants: the impact of zygoma bone support on biomechanics. J Oral Implantol. 2014;40(3):231–237.
- Goker F, Grecchi E, Del Fabbro M, Tedesco A, Borgonovo A, Bedendo A, et al. Oral rehabilitation with unilateral zygomatic implants: A case series of 32 patients. Int J Oral Implantol (Berl). 2022;15(2):181–190.
- Esposito M, Barausse C, Balercia A, Pistilli R, Ippolito DR, Felice P. Conventional drills vs. piezoelectric surgery preparation for placement of four immediately loaded zygomatic oncology implants in edentulous maxillae: results from 1-year split-mouth randomised controlled trial. Eur J Oral Implantol. 2017;10(2):147–158.
- Balshi SF, Wolfinger GJ, Balshi TJ. A retrospective analysis of 110 zygomatic implants in a single-stage immediate loading protocol. Int J Oral Maxillofac Implants. 2009;24(2):335–341.
- Mozzati M, Mortellaro C, Arata V, Gallesio G, Previgliano V. Rehabilitation with 4 zygomatic implants with a new surgical protocol using ultrasonic technique. J Craniofac Surg. 2015;26(3):722–728.
- Becktor JP, Isaksson S, Abrahamsson P, Sennerby L. Evaluation of 31 zygomatic implants and 74 regular dental implants used in 16 patients for prosthetic reconstruction of the atrophic maxilla with cross-arch fixed bridges. Clin Implant Dent Relat Res. 2005;7(3):159–165.
- Gebretsadik HG. The success rate of zygomatic implant in oro-facial reconstructive surgery: A systematic review. Orapuh J. 2021;2:2.
- Gil SG, Diago MP, Martínez JB, Bowen EM. Rehabilitation of severely resorbed maxillae with zygomatic implants: an update. Med Oral Patol Oral Cirugia Bucal. 2007;12(3):E216–E220.
- Parel SM, Brånemark PI, Ohrnell LO, Svensson B. Remote implant anchorage for the rehabilitation of maxillary defects. J Prosthet Dent. 2001;86(4):377–381.
- Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implants. 2010;25(6):1213–1221.
- Al-Nawas B, Wegener J, Bender C, Wagner W. Critical soft tissue parameters of the zygomatic implant. J Clin Periodontol. 2004;31(7):497–500.
- Lombardo G, D’Agostino A, Trevisiol L, Romanelli MG, Mascellaro A, Gomez-Lira M, et al. Clinical, microbiologic and radiologic assessment of soft and hard tissues surrounding zygomatic implants: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(5):537–546.
- Sharma A, Rahul GR. Zygomatic implants/fixture: a systematic review. J Oral Implantol. 2013;39(2):215–224.
- Migliorança RM, Sotto-Maior BS, Senna PM, Francischone CE, Cury AADB. Immediate occlusal loading of extrasinus zygomatic implants: A prospective cohort study with a follow-up period of 8 years. Int J Oral Maxillofac Surg. 2012;41(9):1072–1076.
- Zwahlen RA, Grätz KW, Oechslin CK, Studer SP. The survival rate of zygomatic implants in atrophic or partially resected maxillae prior to functional loading: a retrospective clinical report. Int J Oral Maxillofac Implants. 2006;21(3):413–420.
- Tzerbos F, Bountaniotis F, Theologie-Lygidakis N, Fakitsas D, Fakitsas I. Complications of zygomatic implants: our clinical experience with 4 cases. Acta Stomatol Croat. 2016;50(3):251–257.
- Corvello PC, Montagner A, Batista FC, Smidt R, Shinkai RS. Length of the drilling holes of zygomatic implants inserted with the standard technique or a revised method: A comparative study in dry skulls. J Cranio-Maxillofac Surg. 2011;39(2):119–123.
- Sales P-H, Gomes M-V, Oliveira-Neto O-B, de Lima F-J, Leão J-C. Quality assessment of systematic reviews regarding the effectiveness of zygomatic implants: an overview of systematic reviews. Med Oral Patol Oral Cirugia Bucal. 2020;25(4):e541–e548.
- Aparicio C, Manresa C, Francisco K, Ouazzani W, Clarós P, Potau JM, Aparicio A, et al. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014;16(3):447–459.
- Aparicio C, Ouazzani W, Garcia R, Arevalo X, Muela R, Fortes V. A Prospective clinical study on titanium implants in the zygomatic arch for prosthetic rehabilitation of the atrophic edentulous maxilla with a follow-up of 6 months to 5 years. Clin Implant Dent Relat Res. 2006;8(3):114–122.
- Davó R. Zygomatic implants placed with a two-stage procedure: a 5-year retrospective study. Eur J Oral Implantol. 2009;2(2):115–124.
Keywords
Maxillary; Resorption; Conventional; Unilateral; Placement; Zygomatic implant
Cite this article
Gebretsadik HG. An update on the success rate of the zygomatic implant in Orofacial reconstructive surgery: A 20 years systematic review. Clin Surg J. 2023;4(1):1–6.
Copyright
© 2023 Heron Gezahegn Gebretsadik. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).