An Update on Possible Biological Complications of the Zygomatic Implant in Orofacial Reconstructive Surgery: A 20 Years Systematic Review
* Heron Gezahegn Gebretsadik;
-
* Heron Gezahegn Gebretsadik: School of Global Health & Bioethics, Euclid University, Gambia.
-
Jan 18, 2023 |
-
Volume: 4 |
-
Issue: 1 |
-
Views: 8792 |
-
Downloads: 2437 |
Abstract
Zygomatic implants are reported to be viable treatment options to restore defective Orofacial soft and hard tissue configuration. A systematic review, which was conducted in November 2019, identified 29 relevant studies for data analysis. In this review, sinus infection, soft tissue trauma, mucositis, hematoma, and paraesthesia were found to be the leading zygomatic implant-associated complications. This systematic follow-up review was carried out in November 2022 to update the previous study’s findings. ISI Web of Science, PubMed, Google Scholar, and Cochrane databases were searched to retrieve relevant articles for data analysis. The search intrigued articles published between December 2019 and October 2022. Finally, 27 new relevant articles were identified after the electronic search. Therefore, the updated review involved a total of 56 studies for data analysis. In an average follow period of 3.7 years, 39 different types of biological complications were found to be reported by all the articles included for data analysis. In other words, comparatively more variety of complications were identified in the updated review. Sinusitis, oroantral fistula, and peri-implantitis were the most frequently reported complications, with 27%, 14%, and 7%, respectively. Generally speaking, the updated study identified a more comprehensive range of biological complications than the initial systematic review. Still, the set of complications identified in this review might still be underreported for various reasons. Hence, it is essential to conduct long-term clinical trials involving broader study participants to understand the reality better.
Abbreviations
ISI: The Institute for Scientific Information; MeSH: Medical Subject Headings; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; CASP: Critical Appraisal Skills Programme; SPSS: Statistical Package for the Social Sciences; OAF: Oroantral Fistula; OAC: Oroantral Communication
Introduction
Zygomatic implants are among the classes of dental implants that differ from conventional implants. Most importantly, they are comparatively very long (30 mm–52.5 mm) and attached to the zygomatic bone [1,2]. Zygomatic implants are self-tapping screws with a 45° angulation, making them viable options to compensate for angulation between the zygoma and the maxilla [3]. Per-Ingvar Brånemark is the first person to design zygomatic implants [4,2]. Brånemark introduced zygomatic implants to obtain posterior maxillary anchorage to replace missed teeth and rehabilitate defected anatomic facial complex [4,5]. Zygomatic implants are reported to be less morbid and play a vital role in the rehabilitation of patients with severely resorbed (atrophied) maxillary alveolar ridge, maxillary sinus pneumatization, failed sinus floor augmentation (or alternatively), failed previous bone grafts (or alternatively), failed conventional implants, congenital facial anomalies, and in post-trauma and maxillectomy defects reconstructive surgical interventions [6]. Zygomatic implants are often combined with 2 to 4 conventional dental implants [2,7].
Various surgical techniques are employed to install zygomatic implants. One or two zygomatic implants can be installed unilaterally or bilaterally [8,9]. Several scientific works since the beginning of 2000 have reported a high success rate of zygomatic implants [10–12]. Yet, a handful of complications are reported following the surgical installment of zygomatic implants [13,14]. Expert surgeons suggest good hand on skills to successfully install zygomatic implants [15,16]. Identifying contraindications associated with the procedure, includingthe presentation of acute sinusitis, history of malignancy, and smoking habits, is also reported to be crucial to enhance the success rate of the intervention. According to reports, several biological complications have been identified following the surgical placement of zygomatic implants [15,17,18]. These biological complications are the focus of this updated systematic review. This review aimed to identify the potential biological complications associated with the surgical placement of zygomatic implants and provide ample evidence to clinicians for clinical application [8]. In fact, a considerable number of surgical complication sassociated with the surgical placement of zygomatic implants were identified in the initial systematic review, which was conducted in November 2019 [19]. However, the types and nature of surgical complications may vary over time. Therefore, the present study aimed to update the biological complications related to zygomatic implant placement by including the latest publications.
Indications of zygomatic Implants: Zygomatic implants are indicated to rehabilitate patients presenting with severely resorbed (atrophied) maxillary alveolar ridge, maxillary sinus pneumatization, failed sinus floor augmentation (or alternatively), failed previous bone grafts (or alternatively), failed conventional implants, congenital facial anomalies, and post-trauma and maxillectomy defects.
Contraindications of zygomatic Implants: Acute sinus infection, maxillary or zygoma pathology, malignant condition, and debilitating immune diseases are some of the major contraindications to surgically installing zygomatic implants. Relative contraindications include chronic infectious sinusitis, the use of bisphosphonates, and smoking more than 20 cigarettes a day.
Materials and Methods
Study design: A systematic review of published literature between December 2019 and October 2022 was conducted to ascertain the study’s primary goal.
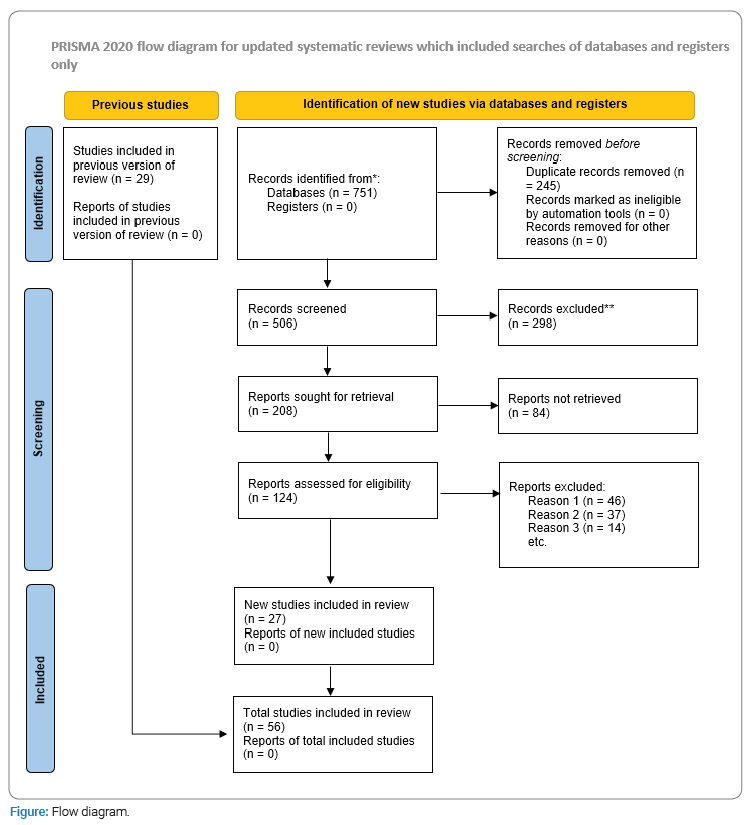
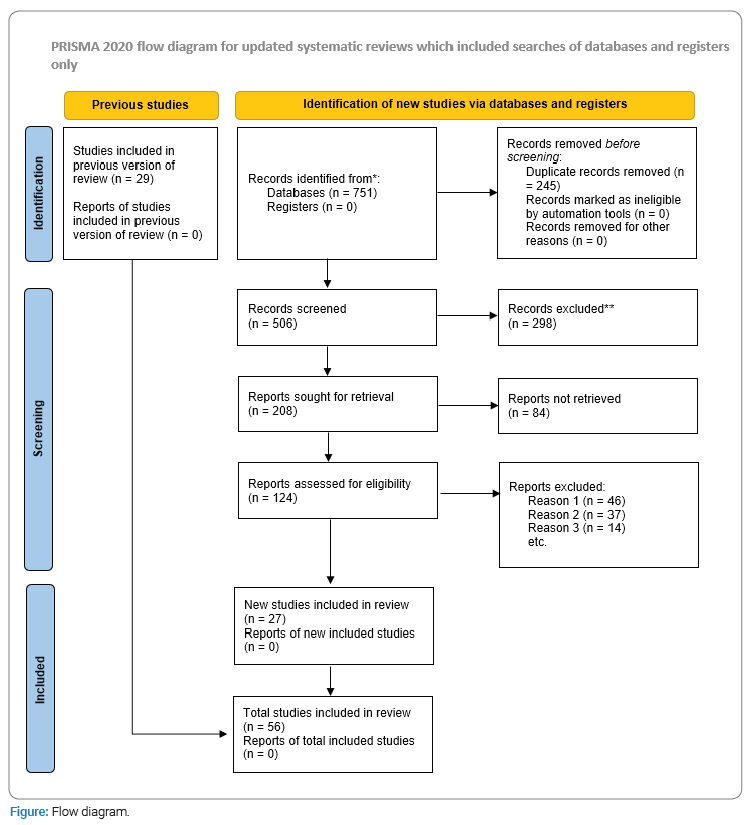
Search strategy: PubMed, ISI Web of Science, Cochrane, and Google Scholar databases were searched to fetch relevant articles for the review. The review was conducted based on the principles of the PRISMA guidelines (``PRISMA`` 2020). The search used different key terms as subjects and adjectives. In addition, CASP analysis was carried out to assess the validity of each potentially relevant article for data analysis.
Inclusion criteria: Studies on zygomatic implants in humans.
Exclusion criteria: Systematic review and meta-analysis, medium of a language other than English, studies with a follow-up period of fewer than six months, and studies on animals (to avoid double-counting) published on the abovementioned databases.
Selection and screening of the literature: The article selection and screening phase of the systematic review began after the initial electronic search. The selection and screening phase involved the identification of raw hits, exclusion of duplicates, revision of abstracts, searching for full texts, in-depth reading of the full texts, and CASP analysis. The CASP analysis was used to assess the quality of the potentially eligible articles for data analysis.
Extraction of data and data analysis: The selection of relevant articles was followed by data extraction and storage. The clinical data recorded in the data extraction template was used to identify the possible biological complications related to zygomatic implant placement. The identified biological complications were organized and presented in two forms: non-aggregated and aggregated. The non-aggregated form presents all the identified biological complications as they are. On the contrary, the aggregated form combined similar biological complications in a group for better understanding. SPSS descriptive statistical software was used to analyze the data.
Ethical clearance: Not applicable.
Results
This section presents the findings of the electronic search. The database search results and the identified biological complications are described in detail as follows.
Databases search results: A total of 751 articles were retrieved after the initial database search. Of these, 245 papers were duplicates and excluded. The remaining 506 articles underwent rigorous screening. Finally, only 27 articles were found to be eligible for data analysis (Figure).
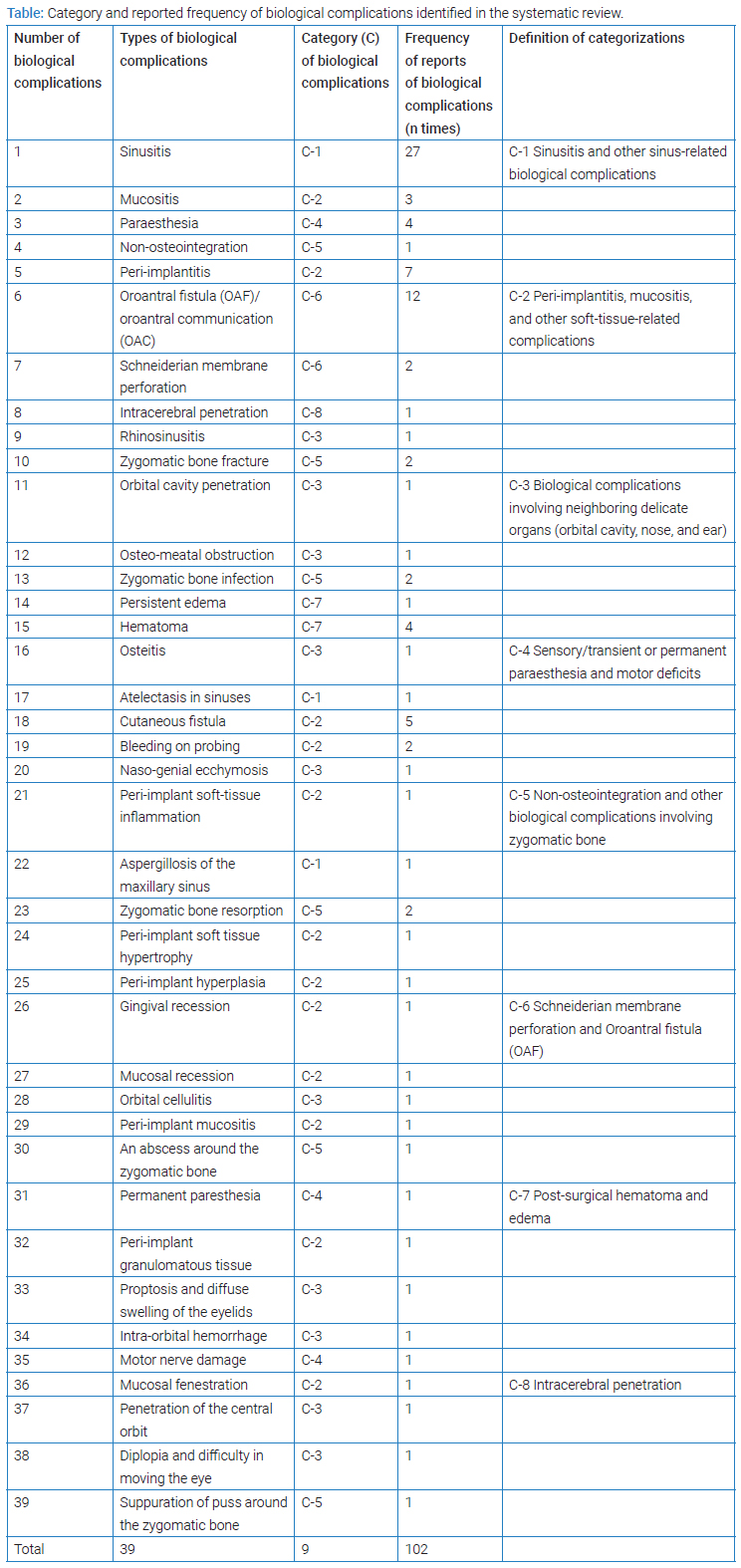
Overall biological complications identified: The articles included in the updated review reported 4840 zygomatic implants placed in 1996 patients. Thirty-nine various biological complications were reported after an average follow-up period of 3.7 years. The complications were reported 102 times, meaning each article reported an average of 1.9 biological complications. For simplicity and better understanding, these biological complications are described individually (non-aggregated) and categorically (aggregated). The categorization (C-1 to C-8) of the identified biological complications considered anatomical proximity, resemblance in types of surgical trauma encountered, similarity in tissue involvement, and affinity in the mechanism of development of the biological condition (Table).
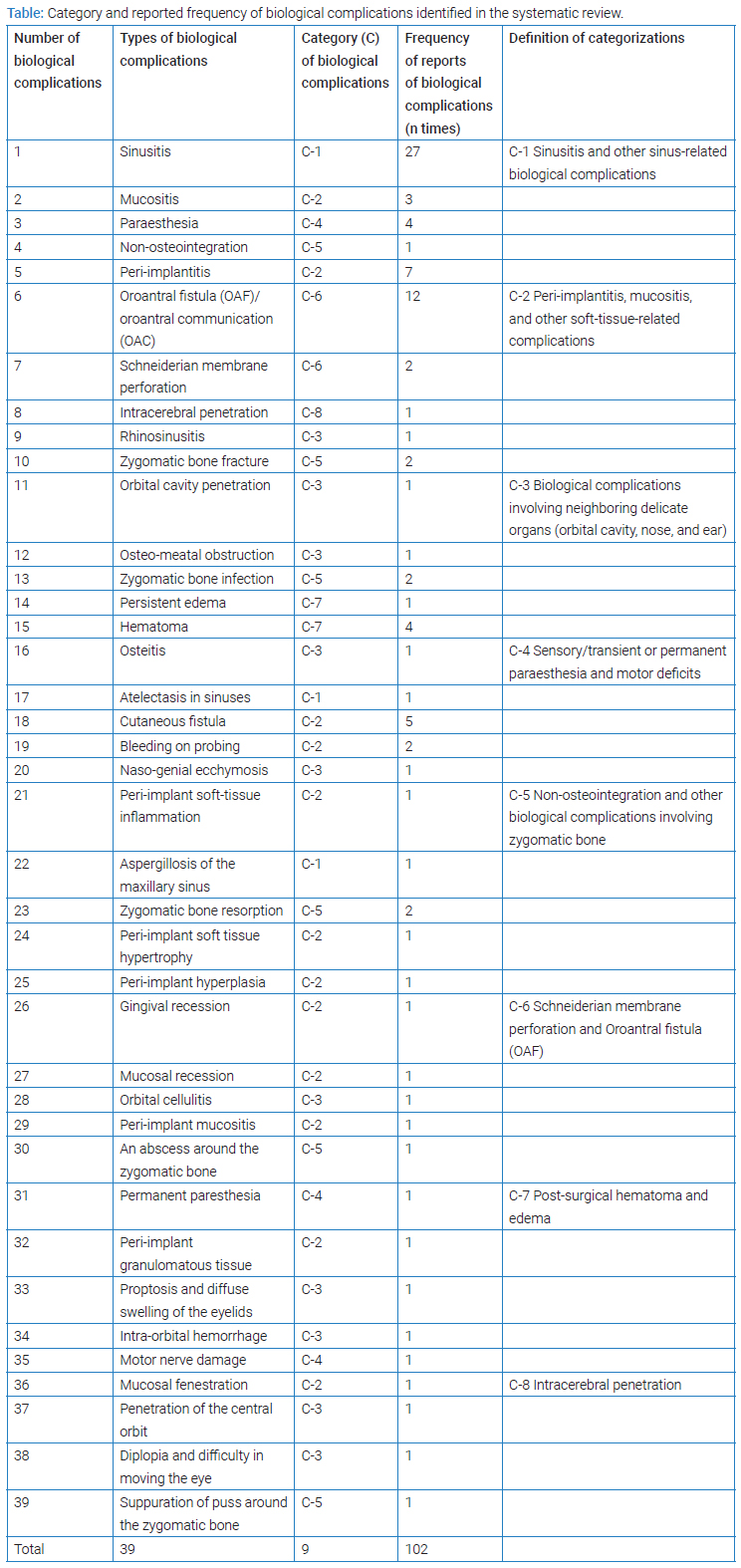
Generally, the overall biological complications identified in this systematic review are classified as aggregated and non-aggregated. Accordingly, sinusitis, oroantral fistula, and peri-implantitis were the most frequently reported non-aggregated biological complications, with 27%, 12%, and 7%, respectively. On the other hand, sinusitis and other sinus-related biological complications; peri-implantitis, mucositis, and other soft-tissue involvements; Schneiderian membrane perforation and Oroantral fistula; complications involving neighboring organs (orbital cavity, nose, and ear); and complications involving zygomatic bone are the leading categorized biological complications with 29%, 24%, 10%, and 10%, respectively (Table).
This systematic follow-up review identified more biological complications than the initial systematic review. A few severe forms of biological complications were also identified in this review. However, in both studies, sinusitis remained the leading biological complication.
Discussion
Dental implants are reported to be viable option to restore missed teeth and associated functional and aesthetic disharmony [20]. However, the surgical placement of dental implants is not free from complications [21]. Likewise, the surgical placement of the zygomatic implant is associated with various biological complications [22–24]. Similarly, various biological complications are identified in this review. Sinusitis and other sinus-related diseases are found to be the most frequently reported types of biological complications in this study. Fifty-eight percent of the papers selected for data analysis have reported sinusitis and other sinus-related diseases.
Furthermore, Oroantral fistula and peri-implantitis were reported by 25.5% and 15% of the literature included for data analysis, respectively. Therefore, Oroantral fistula and peri-implantitis were the second and third most frequently reported biological complications following the placement of zygomatic implants to reconstruct the Orofacial region. Other major biological complications include paraesthesia, mucositis, Schneiderian membrane perforation, orbital cavity involvement, zygomatic bone fracture, cutaneous fistula or fenestration, intracerebral penetration of zygomatic implant, and hematoma. In this regard, similar surgical complications were also reported by other authors [25,26]. Therefore, the most frequently reported biological complications identified in this systematic review are discussed one by one as follows.
Sinusitis and other sinus-related biological complications: Sinusitis or sinus membrane inflammation may be triggered by mechanical and biological factors [27]. The surgical placement of a zygomatic implant in the zygomatic fixture is reported to cause mechanical and/or biological-induced sinusitis [28]. Sinusitis and other sinus-related conditions are found to be the most frequently reported biological complications in this review. Twenty-nine percent of the biological complications identified in this systematic review are sinusitis and other sinus-related diseases. In fact, 27% of all the reported biological complications are sinusitis.
Similarly, Becktor et al. reported 19.4% of sinusitis among patients who underwent surgical placement of ZIs. On the other hand, Chrcanovic et al. reported a relatively low sinusitis incidence (5.2%) in patients who received ZIs to reconstruct the Orofacial region [29]. These variations can arise from different factors, including the technical skill of the operating surgeons, the implant designs, and operating settings [29–31]. Various scientific works suggest that peri-implant mucositis is the first stage of peri-implantitis [32]. Peri-implantitis, mucositis, and other soft-tissue-related problems constituted 24% of all biological complications reported in this systematic review. This set of postoperative outcomes is the second most reported biological complication identified in this study. In this regard, Chrcanovic et al. reported a 3.6% incidence of mucositis, similar to the 3% non-aggregate report in this systematic review [2]. On the other hand, several works of literature reported the occurrence of soft-tissue-related biological complications after the surgical placement of zygomatic implants [28,33].
Schneiderian membrane perforation and OAF: Schneiderian membrane perforation and OAF are the most common types of soft-tissue-related surgical complications [34]. Displacements of teeth, roots of teeth, dental implants, and other surgical instruments are the leading causes of maxillary sinus perforation. This leads to the unwanted communication of the sinus and the oral cavity [35,14]. The incidence rate of Schneiderian membrane perforation and Oroantral fistula varies in different pieces of literature [36]. Most related reports revealed between 1.5% and 7.5% incidence rates, except for Becktor et al. who reported 29% [29]. A significant proportion of soft-tissue-related biological complications have also been identified in this review. This study revealed a 10% incidence rate of Schneiderian membrane perforation and Oroantral fistula.
Non-Osseointegration and other biological complications involving the zygomatic bone: Lack of osseointegration is a major factor in the failure of zygomatic implants [37,38]. Non-osseointegration constituted 1% of all complications identified in this study. Authors such as Becktor et al. Chrcanovic et al. and Migliorança et al. reported 9.7%, 4.2%, and 2.5% incidence rates of non-osteointegration, respectively [29,39]. In this regard, the 2.08%, 1.5%, and 2.5% incidence rates reports of Duarte et al. Aparicio et al. and Migliorança et al. respectively, are comparable to the finding of this study. Zygomatic bone fracture, resorption, and infection are the other major biological complication identified in this systematic review. In general, non-Osseointegration and other biological complications involving the zygomatic bone constituted 10% of all biological complications identified in this study.
Hematoma and other biological complications involving neighboring delicate organs: Various research works have reported several uncommon biological complications after installing zygomatic implants surgically [13,40,41]. Likewise, intracerebral penetration, aspergillosis, rhinosinusitis, orbital cellulitis, otitis, motor skill deficit, orbital cavity penetration, naso-genial ecchymosis, bulging eyes, or proptosis, intra-orbital hemorrhage, diplopia, and persistent pain are identified in this review. The involvement of delicate organs comprised 10% of all biological complications identified in this study. According to reports, a hematoma is one of the most common biological complications associated with zygomatic implants [42,43]. Alike, 4% of the biological complications identified in this review were hematoma related.
Paraesthesia: Several studies have reported paraesthesia after zygomatic implant placement. Traumatic involvement of the infraorbital and zygomaticofacial nerves are the leading causes of zygomatic implant placement-related paraesthesia [2,10,44]. This review also disclosed a 4% paraesthesia that could comply with the 5.4% and 4.6% prevalence reports of Bedrossian and Aparicio et al. respectively [45,46].
Conclusion
Biological complications that are associated with the surgical placement of zygomatic implants vary from mild to severe. This review identified varying degrees of biological complications, with sinusitis being the leading cause of post-surgical morbidity among patients who underwent Orofacial reconstructive surgery using zygomatic implants. In fact the review also identified potentially fatal biological complications. Therefore, the surgical placement of zygomatic implants should be reserved only for clinicians with vast knowledge and surgical expertise. In general, the findings of this study suggest to all implant surgeons to be cautious about the many, particularly the severe biological complications that are related to zygomatic implant placement. Yet, the importance of installing more rigorous studies should be underscored.
Acknowledgment
I want to thank Dr. Ignacio Zapardiel and Dr. David Madruga for their helpful scientific recommendations during the initial phase of the study.
Conflict of Interest
The author declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Davó R, Pons O, Rojas J, Carpio E. Immediate function of four zygomatic implants: a 1-year report of a prospective study. Eur J Oral Implantol. 2010;3(4):323–334.
- Aparicio C, Manresa C, Francisco K, Ouazzani W, Clarós P, Potau JM, Aparicio A, et al. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014;16(3):447–459.
- Prithviraj DR, Vashisht R, Bhalla HK. From maxilla to zygoma: A review on zygomatic implants. J Dent Implants. 2014;4(1):44.
- Brånemark PI, Gröndahl K, Ohrnell LO, Nilsson P, Petruson B, Svensson B, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70–85.
- Fernández H, Gómez-Delgado A, Trujillo-Saldarriaga S, Varón-Cardona D, Castro-Núñez J. Zygomatic implants for the management of the severely atrophied maxilla: a retrospective analysis of 244 implants. J Oral Maxillofac Surg. 2014;72(5):887–891.
- Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: a 6-48 months follow-up study. Clin Oral Implants Res. 2004;15(1):18–22.
- Davó R. Zygomatic implants placed with a two-stage procedure: a 5-year retrospective study. Eur J Oral Implantol. 2009;2(2):115–124.
- Aparicio C, Ouazzani W, Aparicio A, Fortes V, Muela R, Pascual A, et al. Immediate/early loading of zygomatic implants: clinical experiences after 2 to 5 years of follow-up. Clin Implant Dent Relat Res. 2010;12 Suppl 1:e77–e82.
- Kuabara MR, Ferreira EJ, Gulinelli JL, Panzarini SR. Use of 4 immediately loaded zygomatic fixtures for retreatment of atrophic edentulous maxilla after complications of maxillary reconstruction. J Craniofac Surg. 2010;21(3):803–805.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and complications of zygomatic implants: an updated systematic review. J Oral Maxillofac Surg. 2016;74(10):1949–1964.
- Hirsch J-M, Ohrnell L-O, Henry PJ, Andreasson L, Branemark P-I, Chiapasco M, et al. A clinical evaluation of the Zygoma fixture: One year of follow-up at 16 clinics. J Oral Maxillofac Surg. 2004;62(9 Suppl 2):22–29.
- Zwahlen RA, Grätz KW, Oechslin CK, Studer SP. Survival rate of zygomatic implants in atrophic or partially resected maxillae prior to functional loading: a retrospective clinical report. Int J Oral Maxillofac Implants. 2006;21(3):413–420.
- Sato FRL, Sawazaki R, Berretta D, Moreira RWF, Vargas PA, de Almeida OP. Aspergillosis of the maxillary sinus associated with a zygomatic implant. J Am Dent Assoc. 2010;141(10):1231–1235.
- Bothur S, Kullendorff B, Olsson-Sandin G. Asymptomatic chronic rhinosinusitis and osteitis in patients treated with multiple zygomatic implants: a long-term radiographic follow-up. Int J Oral Maxillofac Implants. 2015;30(1):161–168.
- Davó R, Malevez C, Rojas J, Rodríguez J, Regolf J. Clinical outcome of 42 patients treated with 81 immediately loaded zygomatic implants: a 12-to 42-month retrospective study. Eur J Oral Implantol. 2008;9 Suppl 1(2):141–150.
- Maló P, de Araújo Nobre M, Lopes A, Ferro A, Moss S. Extramaxillary surgical technique: clinical outcome of 352 patients rehabilitated with 747 zygomatic implants with a follow-up between 6 months and 7 years. Clin Implant Dent Relat Res. 2015;17 Suppl 1:e153–e162.
- Yalçın M, Can S, Akbaş M, Dergin G, Garip H, Aydil BA, et al. Retrospective analysis of zygomatic implants for maxillary prosthetic rehabilitation. Int J Oral Maxillofac Implants. 2020;35(4):750–756.
- Davó R, David L. Quad zygoma: technique and realities. Oral Maxillofac Surg Clin N Am. 2019;31(2):285–297.
- Gebretsadik HG. Possible surgical complications of the zygomatic implant in oro-facial reconstructive surgery: A systematic review. Orapuh J. 2021;2(2):e818.
- Alghamdi HS, Jansen JA. The development and future of dental implants. Dent Mater J. 2020;39(2):167–172.
- Romanos GE, Delgado-Ruiz R, Sculean A. Concepts for prevention of complications in implant therapy. Periodontol 2000. 2019;81(1):7–17.
- Mavriqi L, Lorusso F, Conte R, Rapone B, Scarano A. Zygomatic implant penetration to the central portion of orbit: a case report. BMC Ophthalmol. 2021;21(1):121.
- Liaw K, Delfini RH, Abrahams JJ. Dental implant complications. Semin Ultrasound CT MR. 2015;36(5):427–433.
- Turkyilmaz I. A proposal of new classification for dental implant complications. J Contemp Dent Pract. 2018;19(8):1025–1033.
- Di Cosola M, Ballini A, Zhurakivska K, Ceccarello A, Nocini R, Malcangi A, et al. Retrospective analysis of clinical and radiologic data regarding zygomatic implant rehabilitation with a long-term follow-up. Int J Environ Res Public Health. 2021;18(24):12963.
- Annibali S, Cristalli MP, Dell’Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review . J Dent Res. 2012;91(1):25–32.
- D’Agostino A, Favero V, Nocini R, Venco J, Nocini PF, Trevisiol L. Does middle meatal antrostomy prevent the onset of maxillary sinusitis after zygomatic implant placement? J Oral Maxillofac Surg. 2019;77(12):2475–2482.
- Fernández-Olarte H, Gómez-Delgado A, López JP, Castro-Núñez J. The use of inferior meatal antrostomy to decrease sinusitis with the placement of zygomatic implants. Int J Oral Maxillofac Implants. 2021;36(1):126–130.
- Becktor JP, Isaksson S, Abrahamsson P, Sennerby L. Evaluation of 31 zygomatic implants and 74 regular dental implants used in 16 patients for prosthetic reconstruction of the atrophic maxilla with cross-arch fixed bridges. Clin Implant Dent Relat Res. 2005;7(3):159–165.
- Mozzati M, Mortellaro C, Arata V, Gallesio G, Previgliano V. Rehabilitation with 4 zygomatic implants with a new surgical protocol using ultrasonic technique. J Craniofac Surg. 2015;26(3):722–728.
- Nave PD, Queralt AV. Zygomatic implants for the rehabilitation of atrophic maxillae: a retrospective study on survival rate and biologic complications of 206 implants with a minimum follow-up of 1 year. Int J Oral Maxillofac Implants. 2020;35(6):1177–1186.
- Hamada Y, Shin D, John V. Peri-implant disease--a significant complication of dental implant supported restorative treatment. J Indiana Dent Assoc. 2016;95(1):31–38.
- French D, Grandin HM, Ofec R. Retrospective cohort study of 4,591 dental implants: Analysis of risk indicators for bone loss and prevalence of peri-implant mucositis and peri-implantitis. J Periodontol. 2019;90(7):691–700.
- Lan L, He Y, An JG, Zhang Y. [Relationship between prognosis and different surgical treatments of zygomatic defects: A retrospective study]. Beijing Da Xue Xue Bao. 2022;54(2):356–362.
- Peñarrocha-Oltra D, Alonso-González R, Pellicer-Chover H, Aloy-Prósper A, Peñarrocha-Diago M. Closure of oroantral communication with buccal fat pad after removing bilateral failed zygomatic implants: A case report and 6-month follow-up. J Clin Exp Dent. 2015;7(1):e159–e162.
- Shahrour R, Shah P, Withana T, Jung J, Syed AZ. Oroantral communication, its causes, complications, treatments and radiographic features: A pictorial review. Imaging Sci Dent. 2021;51(3):307–311.
- Franco-Carro B, Barona-Dorado C, Martínez-González MJS, Rubio-Alonso LJ, Martínez-González JM. Meta-analytic study on the frequency and treatment of oral antral communications. Med Oral Patol Oral Cirugia Bucal. 2011;16(5):e682–e687.
- Filho HN, Amaral WS, Curra C, dos Santos PL, Cardoso CL. Zygomatic implant: Late complications in a period of 12 years of experience. Rev Clínica Periodoncia Implantol Rehabil Oral. 2016.
- Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017;73(1):7–21.
- Migliorança RM, Sotto-Maior BS, Senna PM, Francischone CE, Cury AADB. Immediate occlusal loading of extrasinus zygomatic implants: a prospective cohort study with a follow-up period of 8 years. Int J Oral Maxillofac Surg. 2012;41(9):1072–1076.
- Van Camp P, Vrielinck L, Gemels B, Politis C. Intraorbital hemorrhage following a secondary intervention at integrated zygomatic implants: A case report. Int J Surg Case Rep. 2018;43:21–24.
- Reychler H, Olszewski R. Intracerebral penetration of a zygomatic dental implant and consequent therapeutic dilemmas: case report. Int J Oral Maxillofac Implants. 2010;25(2):416–418.
- Wälivaara DÅ, Isaksson S, Johansson LÅ. Frontal bone and modified zygomatic implants for retention of a nasal prosthesis: Surgical planning using a three-dimensional computer software program. J Plast Surg Hand Surg. 2011;45(2):109–112.
- Esposito M, Barausse C, Balercia A, Pistilli R, Ippolito DR, Felice P. Conventional drills vs piezoelectric surgery preparation for placement of four immediately loaded zygomatic oncology implants in edentulous maxillae: results from 1-year split-mouth randomised controlled trial. Eur J Oral Implantol. 2017;10(2):147–158.
- Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implants. 2010;25(6):1213–1221.
- Aparicio C, Ouazzani W, Garcia R, Arevalo X, Muela R, Fortes V. A prospective clinical study on titanium implants in the zygomatic arch for prosthetic rehabilitation of the atrophic edentulous maxilla with a follow-up of 6 months to 5 years. Clin Implant Dent Relat Res. 2006;8(3):114–122.
Keywords
Oroantral fistula; Cutaneous fistula; Hematoma; Paraesthesia; Sinusitis; Peri-implantitis
Cite this article
Gebretsadik HG. An update on possible biological complications of the zygomatic implant in orofacial reconstructive surgery: A 20 years systematic review. Clin Surg J. 2023;4(1):1–8.
Copyright
© 2023 Heron Gezahegn Gebretsadik. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).