Laparoscopic Intraperitoneal Onlay Mesh (IPOM) Repair in Management of Inguinal Hernia: A Retrospective Cohort Study
* Faramarz Karimian;
Mohammadzadeh N;
Jamali M;
Ataei-Ashtiani Z;
-
* Faramarz Karimian: Imam Khomeini Hospital Complex (IKHC), Tehran University of Medical Sciences, Tehran, Iran.
-
Mohammadzadeh N: Imam Khomeini Hospital Complex (IKHC), Tehran University of Medical Sciences, Tehran, Iran.
-
Jamali M: Imam Khomeini Hospital Complex (IKHC), Tehran University of Medical Sciences, Tehran, Iran.
-
Ataei-Ashtiani Z: University of Melbourne, Melbourne, Australia.
-
Aug 02, 2022 |
-
Volume: 3 |
-
Issue: 3 |
-
Views: 6694 |
-
Downloads: 1828 |
Abstract
The Laparoscopic Intraperitoneal Onlay Mesh (IPOM) technique for managing primary inguinal hernia repair has shown conflicting results in previous studies. The main concerns associated with this technique are intestinal adhesion and recurrence of a hernia. However, these concerns need to be balanced with associated advantages, including ease of performance, short operative and anesthesia time, and lower incidence of injuries to the spermatic cord and adjacent structures. Therefore, a retrospective study was conducted on a series of IPOM repairs for managing primary inguinal hernia. The study showed no additional complications related to intestinal adhesion on the mesh. Furthermore, discontinuing the hernia sac significantly reduced the recurrence rate; however, pain during follow-up was associated with recurrence.
Abbreviations
IPOM: Intraperitoneal Onlay Mesh; TEP: Total Extra-Peritoneal; TAPP: Trans-Abdominal Pre-Peritoneal; BMI: Body Mass Index
Introduction
Laparoscopic Intraperitoneal Onlay Mesh (IPOM) repair technique is an underutilized surgical option in managing primary inguinal hernia repair. The two main concerns with IPOM repair are; intestinal adhesion to the exposed mesh and recurrence. An early report of laparoscopic inguinal hernia IPOM repair in pigs [1] displayed strong evidence that indirect inguinal hernias in male pigs can be successfully repaired via laparoscopic placement of polypropylene prosthesis over the indirect inguinal hernia defect. The researchers noted a significant reduction in the rates of adhesion formation when the prosthesis was placed laparoscopically compared to open surgery. In addition, no prosthesis erosion into the viscera was observed, even with the placement of uncovered mesh [1]. Phillips et al. analyzed laparoscopic inguinal hernia repairs utilizing various surgical techniques, including IPOM repairs (345 from a sample size of n = 2,559). The IPOM group had a 2% recurrence rate and a 14% complication rate compared to Trans-Abdominal Pre- Peritoneal (TAPP) laparoscopic repair, with a 1% recurrence rate and a 7% complication rate. No intestinal obstruction or complications related to mesh adhesion in the IPOM group were reported [2].
The Laparoscopic placement of the Intraperitoneal Onlay Mesh (IPOM) technique for ventral and incisional hernia repair has been successfully taught and practiced [3]. This method is an acceptable alternative to open repair of anterior abdominal wall hernias. Recent studies have not found statistically significant differences in the rates of pain and recurrences of hernia between IPOM and open sub-lay anterior abdominal wall hernia repair, as well as no additional complications related to intestinal adhesion to the mesh [4]. Considering the results of laparoscopic IPOM repair for ventral hernia, it can be concluded that applying this technique for primary inguinal hernia repair may produce similar results.
The recently developed composite polypropylene meshes covered with collagen have shown promising results with a minimal propensity to form adhesions. Advantages of IPOM in inguinal hernia repair include; ease of performance, shorter anesthesia and operation time, and reduction in injuries to adjacent viscera in the deep inguinal ring(mainly the bladder, vascular, and cord structures). The researchers of this study report a series of IPOM repairs for patients with primary inguinal hernia, mainly focusing on the assessment of recurrence and bowel adhesion to mesh. This study aims to assess the safety and practicality of the IPOM technique, as well as obtain preliminary results for future studies.
Materials and Methods
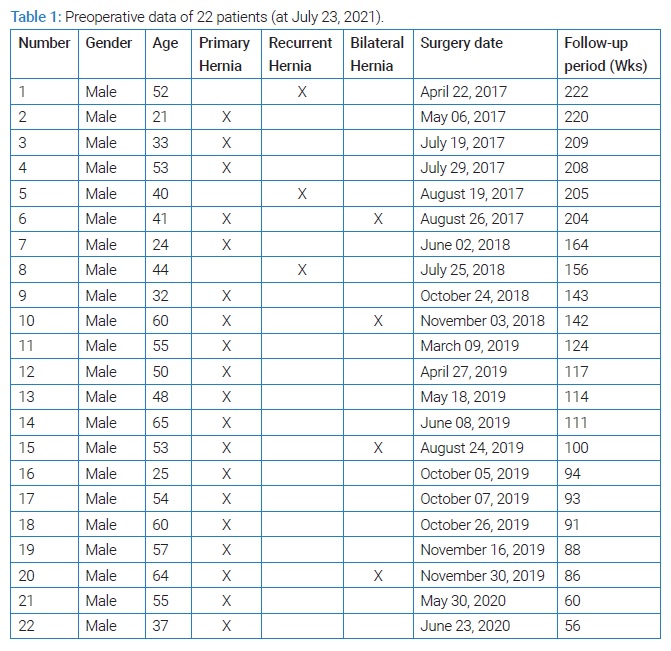
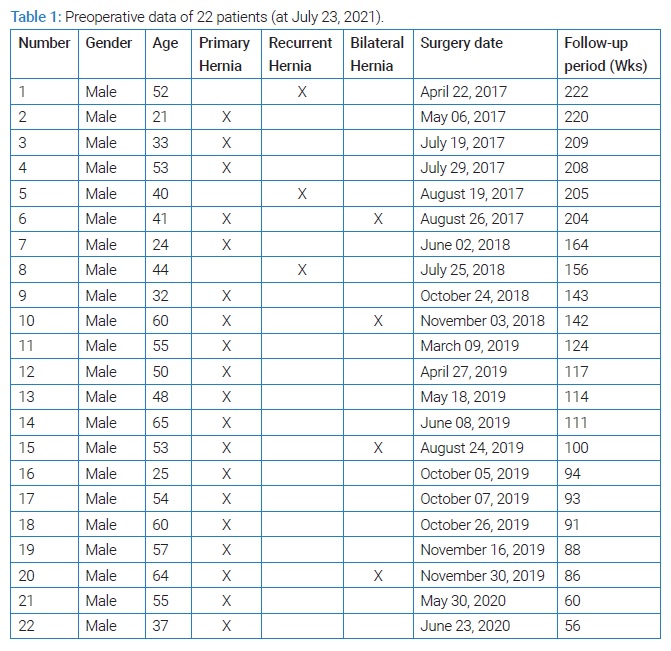
This is a retrospective cohort study performed in a tertiary care university hospital. The researchers performed no clinical intervention. Patients’ personal data remained confidential. Aspects of the inclusion criteria included patients diagnosed with an inguinal hernia who were managed surgically from April, 2017 to July, 2020. Participants who met the inclusion criteria were evaluated for eligibility. Data was collected by using outpatient clinic files, as well as patient follow-ups (refer to Table 1 for the study schematic).
Inclusion criteria: All patients with laparoscopic IPOM inguinal hernia repair from the first of April, 2017 to the first of July, 2020 (April 01, 2017 to July 01, 2020).
Exclusion criteria: Patients with missing data or who were lost during follow-up were excluded.
Data extraction: Data on surgical complications and recurrence were extracted from the inpatient as well as outpatient clinic file records and during the follow-up appointments. Surgical site complication was defined as any new regional complaint developed after surgery. Recurrence was defined as a frank reappearance of a hernia bulge or ultrasonographic finding. The endpoint of the follow-up period was at the end of the first postoperative year. This cut-off point was chosen based on the observation that new complications or recurrences did not occur after 12 months during the follow-up period. Data collection was finalized on the twenty-third of July, 2021. All the patients were contacted by phone and were asked about complications, recurrence, and any other specific concerns they may have. If there were any uncertainties, patients were asked to visit the clinic to be physically examined and undergo imaging if indicated. Postoperative follow-ups ranged from 56 weeks to 222 weeks.
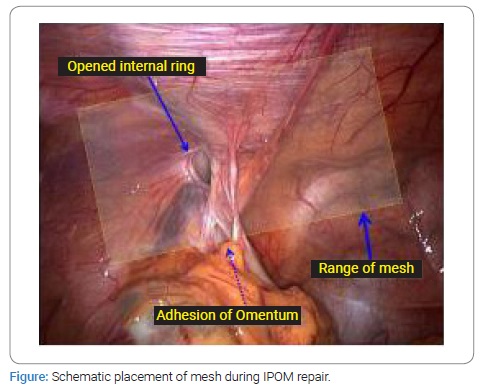
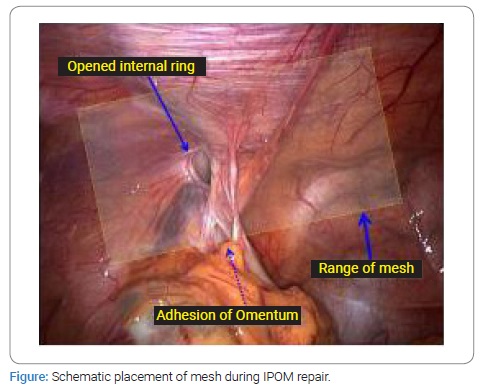
Study groups: In some patients, the hernia sac was left untouched, and the mesh was laid over the defect. In other patients, the hernia sac was cut circumferentially at the internal inguinal ring and excised if small or left to retract distally if large; and the mesh was laid over the defect (Figure). Hernia defect was covered by a 10 cm x 15 cm composite collagen-coated polypropylene mesh. 3–5 tackers fixed mesh along the upper margin. In some patients, medial, lateral, and lower margins of mesh were also fixed by tackers to prevent up-rolling. In addition, upper and lower mesh margins were placed at roughly equal distances from the upper and lower edges of the hernia defect. As a result, the medial margin of the mesh laid over the medial umbilical ligament, and the lateral margin extended to the anterior superior iliac spine.
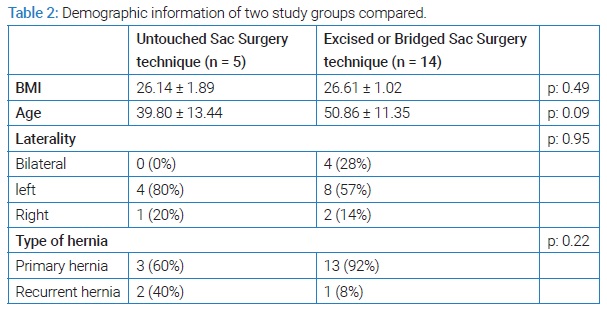
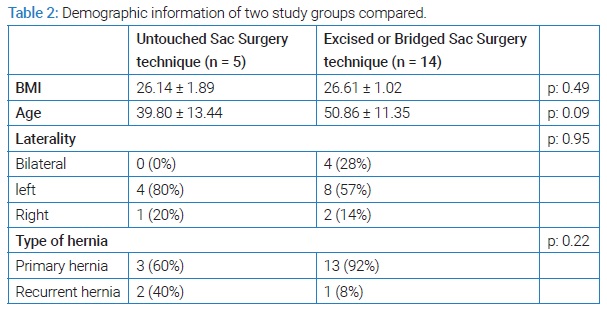
Data analysis: The participants’ data were stratified into two groups, those with untouched hernia sacs and those with excised or bridged and discontinued hernia sacs. Some demographic factors such as age, BMI, type of inguinal hernia (primary vs. recurrent), and the location of the hernia were analyzed between the two groups. The study data were analyzed using the Statistical Package for the Social Sciences (SPSS) software, version 26. The independent sample t-test and chi-square were used for the analysis. A 95% confidence interval and p-values less than 0.05 were considered statistically significant.
Results
From April, 2017 to July, 2020, 22 patients with inguinal hernia were operated on using the laparoscopic IPOM repair technique. Three patients were lost to follow-up and were thus excluded (n = 19). The patients were all male, with an age range of 21 years to 65 years (Mean: 47.95, SD: 12.581) and BMI ranging from 23.68 kg/m2 to 28.65 kg/m2 (Mean: 26.4889, SD: 1.26377). Confounding factors, such as hernia risk factors including; obstructive lung disease (i.e., chronic cough), increased intra-abdominal pressure (e.g., chronic constipation), obstructive uropathy (e.g., prostatic enlargement), and heavy physical activity (e.g., heavy manual worker) were not present in either patient group. Furthermore, diabetes or smoking habits were not found in these patients. This homogeneity in the study population demographic was most likely due to the narrow selection criteria and the IPOM technique repair eligibility.
There was no conversion to open surgery. The untouched sac group included five patients. Patients with excised or bridged and discontinued sacs included 14 patients. Groups were matched by age, BMI, location of the hernia, and incidence of primary or recurrent hernia (Table 2). The total number of recurrences was 6 out of 19 (31.5%). The recurrence number in those with an untouched sac was 4 out of 5 (80%) vs. 2 out of 14 (14.2%) in those with a discontinued sac; results showed a statistically significant reduction in patients managed by IPOM and the discontinued sac method (p-value = 0.017). No complication related to intestinal adhesion to the mesh was observed in both groups. Surgical site complications were as follows; two patients with an untouched sac had surgical site pain and developed recurrence two weeks after surgery, and another patient with a discontinued sac and surgical site pain developed recurrence 13 weeks after surgery. Statistical analysis showed that surgical site pain significantly correlated with recurrence (p-value = 0.021). Two patients (one with dysuria and another with dysuria in addition to urinary frequency), both with a discontinued sac, did not develop recurrence on long-term follow-up (more than 12 months). Their complaints were managed by medical treatment.
Discussion
The largest comparative systematic review on outcome analysis of laparoscopic inguinal hernia repair, comparing 345 IPOM repairs to 2,559 other types of laparoscopic hernia repairs, was published in 1995 [2]. Since then, no similar large-scale study has provided further guidance on the best evidence-based approach. A smaller study encompassing a series of 52 IPOM inguinal hernia repairs in 50 patients reported two recurrences (near 4%) and no complications related to mesh adhesion during a 7 months–31 months follow-up [5]. Hatzitheofilou and his team concluded that the IPOM method was less time-consuming, associated with minimal postoperative pain, shorter hospital stay, and lower hospital costs [5]. During the same period, a prospective randomized clinical trial including 59 TAPP and 56 IPOM repairs demonstrated 11.1% early recurrence for IPOM and no recurrence for TAPP (p < 0.01). No complications related to mesh adhesion to intestines were reported, leading the research team to conclude that TAPP was an excellent technique with no early recurrence and suggesting avoiding IPOM laparoscopic hernia repair where possible [6]. One study recommended IPOM for inguinal hernia repair in patients with chronic obstructive pulmonary disease under spinal anesthesia when there is a risk of ventilator dependence following general anesthesia. Similar to preceding studies, no recurrence or mesh-related complications were recorded after six months of follow-up [7].
Laparoscopic IPOM repair was found to be as effective as open tension-free repair, even in physically active young men and heavy-duty workers, some with bilateral and recurrent hernias [8]. At the end of the 12-month follow-up period, there were minor complications unrelated to mesh and no recurrence; however, at the 18-month follow-up, there was a 3.3% recurrence following IPOM repair, and no major visceral complication was reported [8,9]. Composite meshes were successfully fixed by fibrin glue in the IPOM technique with no recurrence after almost two years and only one trocar site hematoma while decreasing the mean operative time by 10-minutes [10]. The feasibility of IPOM was assessed in patients with previous lower abdominal surgeries as an alternative to Total Extra-Peritoneal (TEP) laparoscopic repair, which is deemed surgically complex in this patient group. One out of 43 patients developed recurrence. There was no major mesh-related complication [11]. IPOM repair is suggested for patients with preperitoneal fibrosis as an alternative to Lichtenstein tension-free open repair, resulting in an equal or better profile in terms of re-recurrence and chronic pain. No major complication related to intestinal adhesion to mesh was found [12]. Single-incision laparoscopic (SIL) intraperitoneal Onlay mesh (IPOM) repair was successfully performed in a small series of patients with a recurrent hernia after conventional anterior and laparoscopic repairs. There were no intra-/postoperative complications, port site hernias, chronic groin pain, or hernia recurrence during a mean follow-up of 24 months [13]. Once again, fibrin glue is suggested for fixation of the lower edge of IPOM, along with tackers at the upper edge, with no complications or recurrence at the end of a one-year follow-up [14]. IPOM repair has been successfully used for inguinal hernia repair following radical prostatectomy when TAPP was impeded by dense preperitoneal fibrosis. For a median period of 36 months, follow-up showed no recurrence; whilst complications following IPOM were comparable to those after TAPP with no major mesh-related visceral complication [15]. In a retrospective comparative series, 176 patients undergoing TAPP repair with their peritoneal flaps left open were compared to 231 patients with peritoneal closure over the mesh. The coated mesh was inserted in both groups. The average follow-up range was 21.6 months ± 23.8 months; within this period, recurrence rates were similar and postoperative complications were not significantly higher in the non-closure group, with p-value = 0.68 and p-value = 0.36 respectively. No bowel obstruction or unplanned reoperation due to intestinal adhesion to mesh was reported [16].
A major concern with IPOM has been intestinal adhesion to mesh and subsequent complications. However, the first animal experiment, as well as more recent studies, have shown that the real incidence is much less than presumed. This is especially true with the new generation of coated meshes. Mesh fixation leads to more complications than mesh adhesion [17]. All the meshes used in this study series were collagen-coated, and no complication related to intestinal adhesion to mesh was observed.
Dissection of the hernia sac during IPOM inguinal hernia repair has been reported as early as 1992 [18]; however, no report could be found regarding the role of hernia sac dissection on recurrence. Although incision of the medial umbilical ligament (fold) to facilitate flat mesh placement and dissection of underlying area to expose Cooper ligament for fixation of mesh is recommended; discontinuation of hernia sac at the internal ring is not a common practice. The sac is always transected during TAPP, TEP, and tension-free open inguinal hernia repair. This study shows that adding the same step to the IPOM technique leads to a significantly lower recurrence rate, p-value = 0.017. It can be hypothesized that discontinuing the hernia sac leads to better mesh adhesion to an underlying unepithelialized raw surface. Therefore, we conclude that when the IPOM technique is chosen for inguinal hernia repair, the sac should be dissected and discontinued, but not necessarily excised.
There was no complication related to intestinal adhesion to mesh in this study. A recent study also showed the safety of TAPP with little or no peritoneal coverage over the mesh [16]. We found that laparoscopic IPOM repair for primary inguinal hernia did not result in complications related to intestinal adhesion to mesh when composite collagen-coated polypropylene mesh was used. Furthermore, recurrence after laparoscopic IPOM repair for primary inguinal hernia was significantly less when the hernia sac was excised or discontinued. Therefore, laparoscopic IPOM repair for primary inguinal hernia with discontinuation of hernia sac can be recommended. Another statistically significant finding of this study was that surgical site pain after laparoscopic IPOM repair was always associated with recurrence (p-value = 0.021). Thus, site pain after laparoscopic can be assumed as a predictor of recurrence.
The main limitations of this study were the retrospective nature of the study, small sample size, and low diversity in patients’ pre-op comorbidities. Ideally, to generalize this recommendation, further research such as a randomized controlled trial with calculated samples with minimum bias and confounding and a larger and more diverse patient demographics is required. This will assist clinicians in stratifying patients and making a patient-focused surgical approach.
Conclusion
Laparoscopic IPOM repair for primary inguinal hernia does not result in visceral adhesion to mesh and subsequent complications when composite collagen-coated polypropylene mesh is used. Recurrence after laparoscopic IPOM repair for primary inguinal hernia is significantly less when excised or discontinued the hernia sac. Surgical site pain after laparoscopic IPOM repair can be a predictor of recurrence.
Acknowledgments
Author’s contribution: The authors would like to acknowledge the contribution made by Ms. Soudabeh Khodarahmi to data collection. She was the senior staff of our research office.
Ethical approval: This is a retrospective cohort study, and no intervention was performed on the patients. Patients’ personal data remained confidential. Therefore, ethical approval was not necessary.
Consent: Not applicable since it is a retrospective study.
Sources of funding: This research did not receive any specific grant from the public, commercial, or not-for-profit funding agencies.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Jr Fitzgibbons RJ, Salerno GM, Filipi CJ, Hunter WJ, Watson P. A laparoscopic intraperitoneal onlay mesh technique for the repair of an indirect inguinal hernia. Ann Surg. 1994;219(2):144–156.
- Phillips EH, Arregui M, Carroll BJ, Corbitt J, Crafton WB, Fallas MJ, et al. Incidence of complications following laparoscopic hernioplasty. Surg Endosc. 1995;9(1):16–21.
- Aura T, Habib E, Mekkaoui M, Brassier D, Elhadad A. Laparoscopic tension- free repair of anterior abdominal wall incisional and ventral hernias with an intraperitoneal Gore-Tex mesh: prospective study and review of the literature. J Laparoendosc Adv Surg Tech A. 2002;12(4):263–267.
- Köckerling F, Simon T, Adolf D, Köckerling D, Mayer F, Reinpold W, et al. Laparoscopic IPOM versus open sublay technique for elective incisional hernia repair: a registry- based, propensity score-matched comparison of 9907 patients. Surg Endosc. 2019;33(10):3361–3369.
- Hatzitheofilou C, Lakhoo M, Sofianos C, Levy RD, Velmahos G, Saadia R. Laparoscopic inguinal hernia repair by an intraperitoneal onlay mesh technique using expanded PTFE: a prospective study. Surg Laparosc Endosc. 1997;7(6):451–455.
- Sarli L, Pietra N, Choua O, Costi R, Cattaneo G. Laparoscopic hernia repair: a prospective comparison of TAPP and IPOM techniques. Surg Laparosc Endosc. 1997;7(6):472–476.
- Catani M, De Milito R, Spaziani E, Chiaretti M, Manili G, Capitano S, et al. [Laparoscopic inguinal hernia repair “IPOM” vs “open tension free”. Preliminary results of a prospective randomized study]. Minerva Chirurgica. 2003;58(6):783–789.
- Catani M, De Milito R, Materia A, Chiaretti M, Spaziani E, G Manili, et al. [Laparoscopic inguinal hernia repair “IPOM” with Dual-Mesh]. Ann Ital Chir. 2003;74(1):53–60;discussion 60–62.
- Olmi S, Scaini A, Erba L, Bertolini A, Croce E. Laparoscopic repair of inguinal hernias using an intraperitoneal onlay mesh technique and a Parietex composite mesh fixed with fibrin glue (Tissucol). Personal technique and preliminary results. Surg Endosc. 2007;21(11):1961–1964.
- Jeon YB, Kim MJ, Hur KY. Laparoscopic Inguinal Hernia Repair by Intraperitoneal Onlay Mesh (IPOM) Technique in Specific Cases as an Alternative Method. Journal of Minimally Invasive Surgery. 2014;17(2):30–35.
- Hyllegaard GM, Friis-Andersen H. Modified laparoscopic intraperitoneal onlay mesh in complicated inguinal hernia surgery. Hernia. 2015;19(3):433–436.
- Tran H, Tran K, Zajkowska M, Lam V, Hawthorne WJ. Single-port onlay mesh repair of recurrent inguinal hernias after failed anterior and laparoscopic repairs. JSLS. 2015;19(1):e2014.00212.
- Mathur RK, Dubey S, Odiya S, A prospective study of laparoscopic repair of inguinal hernia by intraperitoneal onlay mesh technique using fibrin glue. Int Surg J. 2016;3(3):1107–1111.
- Ohuchi M, Inaki N, Nagakari K, Kohama S, Sakamoto K, Ishizaki Y. Surgical procedures and results of modified intraperitoneal onlay mesh repair for inguinal hernia after radical prostatectomy. J Laparoendosc Adv Surg Tech. 2020;30(11):1189–1193.
- Kane ED, Leduc M, Schlosser K, Parentela N, Wilson D, Romanelli JR. Comparison of peritoneal closure versus non-closure in laparoscopic trans-abdominal preperitoneal inguinal hernia repair with coated mesh. Surg Endosc. 2018;32(2):627–637.
- Hanada K, Narita M, Goto K, Okada H, Okura K, Jikihara S, et al. Chronic inguinal pain after laparoscopic intraperitoneal onlay mesh (IPOM) repair for inguinal hernia treated successfully with laparoscopic selective neurectomy: A case report. Int J Surg Case Rep. 2017;38:172–175.
- Jr. Fitzgibbons R, Camps J, Cornet DA, Nguyen NX, Litke BS, Annibali R, et al. Laparoscopic inguinal herniorrhaphy. Results of a multicenter trial. Ann Surg. 1995;221(1):3–13.
- Yang XF, Liu JL. Laparoscopic repair of inguinal hernia in adults. Ann Transl Med. 2016;4(20):402.
Keywords
Laparoscopic surgery; Inguinal hernia repair; Intraperitoneal onlay mesh; IPOM
Cite this article
Karimian F, Mohammadzadeh N, Jamali M, Ataei-Ashtiani Z. Laparoscopic intraperitoneal onlay mesh (IPOM) repair in management of inguinal hernia: a retrospective cohort study. Clin Surg J. 2022;3(3):1–6.
Copyright
© 2022 Faramarz Karimian. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).