Proliferating Trichilemmal Tumor of the Scalp: A Case Report and Literature Review
Xu-Lei Jiang;
* Ying Yang;
* Shao-Rong Lei;
-
Xu-Lei Jiang: Department of Plastic Surgery, Xiangya Hospital, Central South University, Changsha 410008, Hunan, PR China.
-
* Ying Yang: Department of Plastic Surgery, Xiangya Hospital, Central South University, Changsha 410008, Hunan, PR China.
-
* Shao-Rong Lei: Department of Plastic Surgery, Xiangya Hospital, Central South University, Changsha 410008, Hunan, PR China.
-
Jul 27, 2022 |
-
Volume: 3 |
-
Issue: 3 |
-
Views: 6941 |
-
Downloads: 1731 |
Abstract
Introduction: Proliferating trichilemmal tumor (PTT), also known as hyperplastic hair cyst or hyperplastic hair follicle cyst, is common in women over 60 years of age and mainly presents as a painless scalp mass. Malignant one was very rare.
Case Presentation: We reported a 27-year-old female patient with a palpable, painless mass at the top of the left head. Pathologic findings suggested a hyperplastic external hair sheath scalp tumor (low-grade malignancy).
Clinical Discussion: PTT is also called the proliferative hair cyst, easily misdiagnosed as squamous cell carcinoma, and is a rare tumor from trichilemmal cells. The onset age of the disease is about 60 years. The malignant transformation is very rare. In this case, the first postoperative pathological findings suggested low-grade malignancy. The patient’s postoperative pathologic result indicates a low grade for the first time. Unfortunately, it has recurred, and it was necessary to remove the lesion again. We needed to make sure the nature of the mass after the pathological examination was so as to provide a basis for subsequent treatment.
Conclusion: Similar to a painless scalp mass, we should consider the possibility of PTT. However, complete case data and pathological diagnosis should confirm the final diagnosis. According to the understanding of this case and related literature, the PTT is a benign lesion but prone to recurrence. Some researchers believe that PTT is malignant because the lesion is initially considered benign but is prone to recurrence and metastasis. Multiple relapses or trauma can cause malignant changes. Currently, the treatment of PTT includes local surgical resection, lymph node dissection, radiotherapy, or chemotherapy. There are currently no clear clinical guidelines for patients with metastatic disease because of the small number of cases of the disease and the rarer incidence of malignancy.
Introduction
Proliferating trichilemmal tumor, also known as hyperplastic hair cyst, is common in women over 60 years of age and occurs mainly on the scalp but also on the back [1–4,8]. The lesion was subcutaneous nodules at the beginning and gradually increased, with a diameter of 0.4 cm ~ 1 cm, and could form plaques that were higher than the skin surface or lobulated [5]. Sometimes ulcerated to resemble squamous cell carcinoma, usually solitary, with occasional two lesions. Rapid enlargement indicated malignancy and could cause regional metastases [6]. It was called Malignant Proliferating Trichilemmal Tumor (MPTT). Malignant was very rare [7]. They usually grew rapidly based on nodules of PTT, resulting in malignant transformation and regional or systemic metastasis [10].
Case Presentation
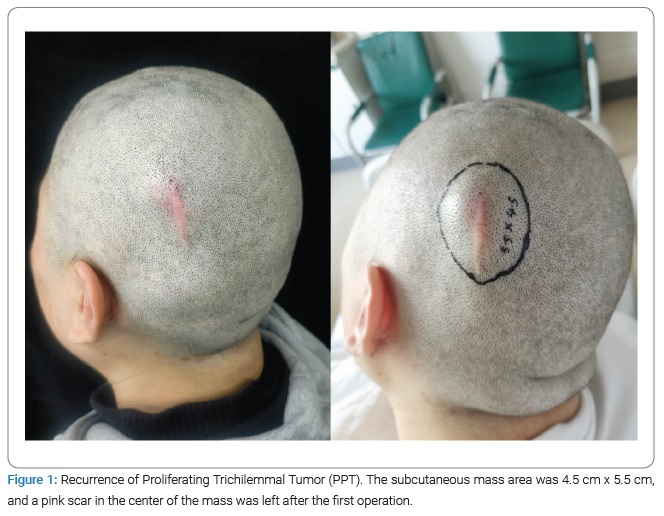
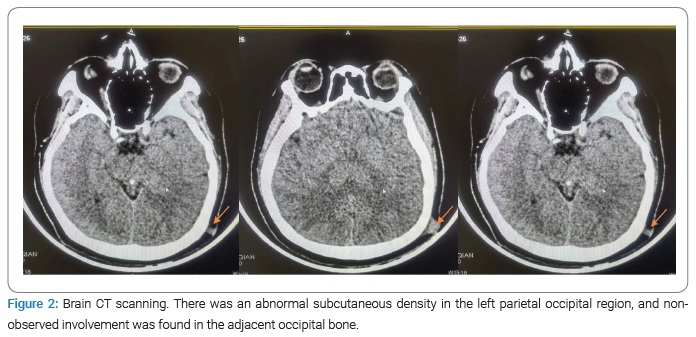
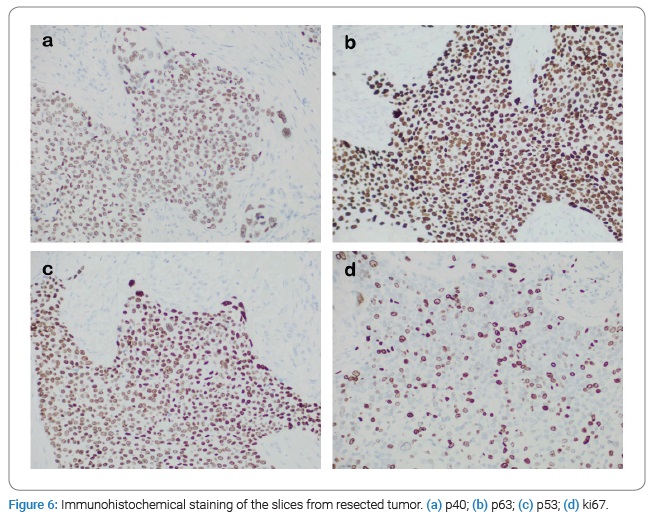
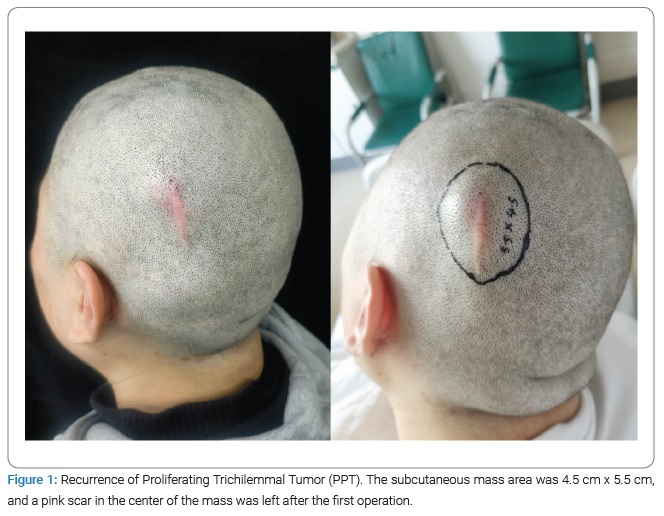
The patient, a 27-year-old female, had accidentally developed a painless quail egg-sized mass on the top of her left head four months ago. In September 2021, left top scalp mass resection was performed in the Outpatient department of Shaoyang Central Hospital. Postoperative pathology suggested Proliferating trichilemmal tumor (PTT). In October 2021, the tumor recurred in situ and gradually increased. In January 2022, pathological sections were sent to our hospital for consultation as PTT: low-grade malignant. She was admitted to our hospital in February 2022, and her mass was about 4.5 cm x 5.5 cm in size, which was almost round. Physical examination: There was no abnormality in the heart, lung, and abdomen during physical examination, and a palpable mass at the left top of the scalp, about 4.5 cm x 5.5 cm in size, slightly hard, relatively regular oval, with a good range of motion, no tenderness (Figure 1). The skin was tight, red, and swollen, with hair growth and no ulceration or pus (Figure 1). No metastasis was found on the chest radiograph and regional lymph node ultrasound. Head CT showed an abnormal subcutaneous density of the left parietal and occipital region without obvious involvement of the adjacent occipital bone (Figure 2).
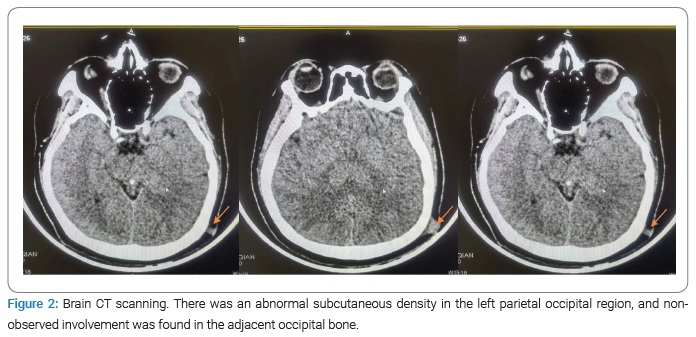
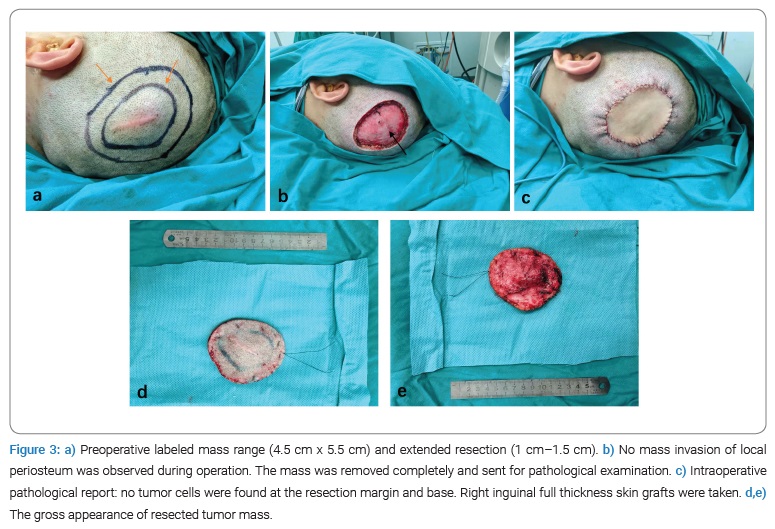
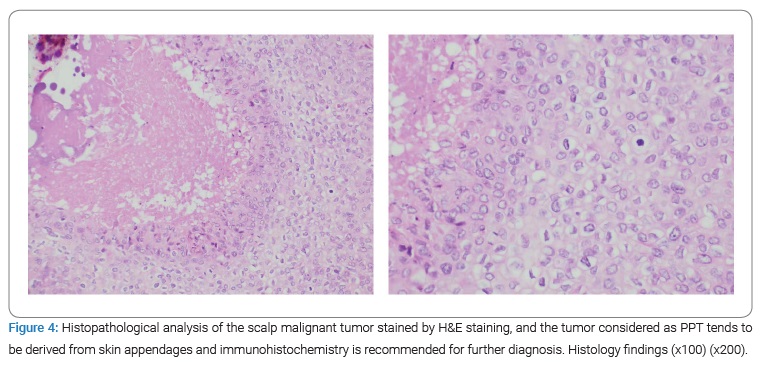
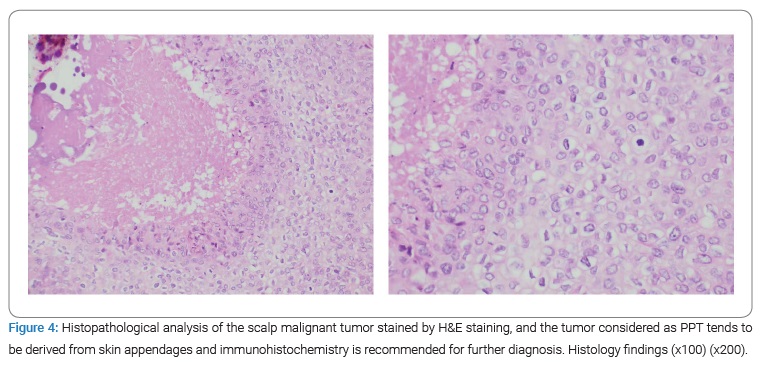
On February 25, 2022, the patient received mass scalp resection, pedicled flap transplantation, skin extraction, and free skin graft in our hospital. Intraoperatively, a complete resection of the frontal periosteum was performed at the edge of the mass 1 cm–1.5 cm (Figure 3). Quick intraoperative pathological suggested: Combined with previous pathological consultation reports, the submitted tissues were consistent with PTT of the scalp, and no tumor residue was found in each base and incision margin. The whole thick skin was taken to cover the wound. Postoperative pathological results showed that: (scalp) malignant tumors tended to be derived from skin appendages.
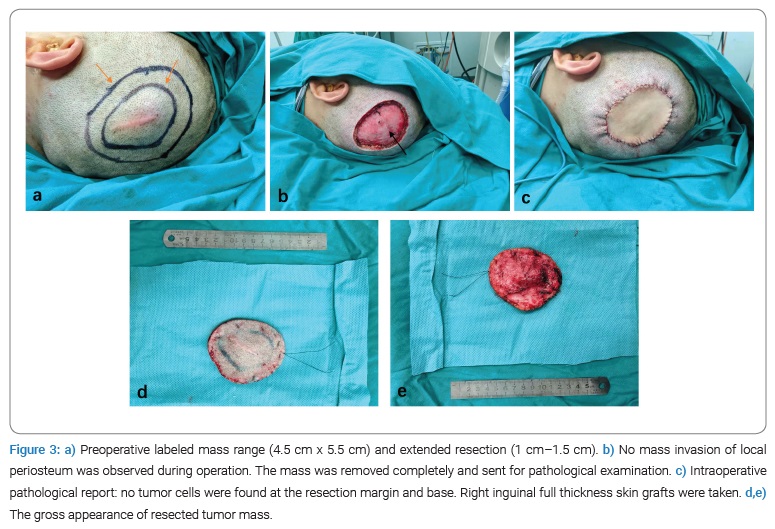
We were considering MPTT. Immunohistochemistry was suggested for further diagnosis (Figure 4). 12 days–14 days after the operation, the unpacking situation is shown in the (Figure 5a). The skin graft area survived well, and the wound healing was good (Figure 5a). Postoperative supplementary pathological diagnosis showed that: (scalp) Proliferating trichilemmal tumor (size: 4 cm x 2.5 cm x 1.6 cm, low grade malignant), immunohistochemical results showed that no tumor plug was found in the vessel, no obvious nerve invasion.

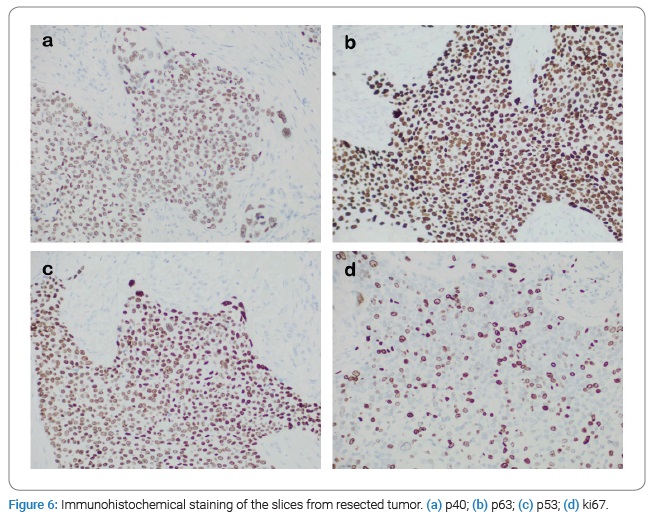
Immunohistochemical results: Ki67 (about 20% (+), CK5/6 (+), P40 (+), P63, GCDFP-15 (-), p53 (+), CD34 (-), D2-40 (+)) (Figure 6). The patient came to the Department of Oncology with the postoperative results. The opinion of the Department of Oncology was as follows: According to the postoperative results, the tumor cell proliferation was relatively inactive and was not prone to recurrence and metastasis. There was no need for follow-up treatment (radiotherapy, chemotherapy, etc.) and regular follow-up (1 month–3 months). One month later, the wound healing and tumor recurrence follow-up showed that the wound in the skin graft area was basically healed, with a scab on the surface, and no local and surrounding tumor recurrence was observed (Figure 5b).
Clinical Discussion
PTT was uncommon and required a relatively high degree of suspicion, especially if it was a rapidly growing, painless mass on the scalp. It was more common in women than men and affected people around the age of 60 years [3,4]. However, this patient was a 27-year-old female. The most common symptom was a painless mass, usually on the scalp, that grew gradually and was prone to recurrence [6,9]. The patient, in this case, had a history of mass scalp resection, and the tumor recurred in situ one month after surgery.
The causes of recurrence after the first operation are summarized as follows:
- Although PTT is a benign tumor, its biggest characteristic is the high recurrence rate, which is also the biggest problem for patients.
- Local hospitals have a limited understanding of the disease and have not made correct judgments.
The disadvantages of the first surgery are: Due to the limited understanding of the disease in local hospitals, preoperative pathological diagnosis and rapid intraoperative pathological examination was not carried out, so the nature of the mass could not be clarified. Therefore, only local resection of the mass was performed without expanded resection. The patient had a history of mass scalp resection, a history of in situ recurrences one month after surgery, and a postoperative pathological diagnosis, which could be clearly diagnosed as a hyperplastic external hair sheath tumor. However, due to the infrequency and rarity of malignant cases of this disease, there were no clear guidelines or consensus for its comprehensive examination and systematic treatment. Some reports suggested that the disease was related to P53 gene mutation [11].
The differential diagnosis is as follows:
- It is often differentiated from squamous cell carcinoma: histologically, malignant hyperplasia of Trichophyton presents with severe nuclear atypia, marked cellular atypia, atypical mitosis, mal keratinized cells, and infiltrating margins. In contrast to squamous cells, squamous cell carcinoma has no external root sheath keratosis, and the process of keratosis is gradual. In contrast, in this tumor, the boundary is clear, and the keratosis is sudden.
- Neurofibroma: Both are benign tumors with a high recurrence rate. PTT and MPTT did not have typical signs of neurofibroma, which is characterized by scattered coffee and milk patches.
- Malignant melanoma: the tumor is often black in color, mostly from the rapid enlargement of the nevus at the beginning, with a high degree of malignancy, often accompanied by ulceration, and even surrounded by satellite foci.
The reasons for not conducting an MR examination in this study are as follows:
- Physical examination: the mass was regular, and the activity was reasonable.
- Preoperative CT of our hospital showed no obvious occipital involvement.
- The price of MR examinations is relatively high, considering the limited economic situation of patients.
MR has many parameters and soft-tissue resolution several times higher than CT. The image obtained by MR is clear, fine, high resolution, with good contrast, and informative, especially for the soft tissue layer. It can detect lesions more effectively and earlier.
Conclusion
Complete case data and pathological diagnosis should probably diagnose similar painless scalp masses that were considered PTT. According to the understanding of this case and relevant literature, PTT is a benign lesion. However, it is prone to recurrence, and the recurrence can also occur malignant, causing regional and systemic lymph node metastasis. Surgical treatment is the preferred early treatment for both benign and malignant patients. There are no clear clinical guidelines for metastatic patients due to the small number of cases of this disease and the rarer occurrence of malignant changes. In this case, we will continue to follow-up, collect more case data, expand more information about the disease, and achieve more accurate and effective treatment.
Acknowledgments
Author contribution: Concept design and preparation of the manuscript: Shaorong Lei, Ying Yang; Literature search: Xulei Jiang; Preparation of draft manuscript: Xulei Jiang, Shaorong Lei, Ying Yang.
Sources of funding: This article received no funding.
Ethical approval: No ethics approval was sought as this was a case report with no direct impact on patient outcome.
Consent: Written informed consent was obtained from the patient to publish this case report and accompanying images.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Garg PK, Dangi A, Khurana N, Hadke NS. Malignant proliferating trichilemmal cyst: a case report with review of literature. Malays J Pathol. 2009;31(1):71–76.
- Deshmukh BD, Kulkarni MP, Momin YA, Sulhyan KR. Malignant proliferating trichilemmal tumor: a case report and review of literature. J Cancer Res Ther. 2014;10(3):767–769.
- Janitz J, Wiedersberg H. Trichilemmal pilar tumors. Cancer. 1980;45(7):1594–1597.
- Brownstein MH, Arluk DJ. Proliferating trichilemmal cyst: a simulant of squamous cell carcinoma. Cancer. 1981;48(5):1207–1214.
- Ackerman AB. On the nature of adnexal neoplasms. J Am Acad Dermatol. 2009;60(3):515.
- Satyaprakash AK, Sheehan DJ, Sangüeza OP. Proliferating trichilemmal tumors: a review of the literature. Dermatol Surg. 2007;33(9):1102–1108.
- Filippou DK, Filippou G, Trigka A, Condilis N, Kiparidou E, Skandalakis P, et al. Malignant proliferating trichilemmal tumour of the scalp. Report of a case and a short review of the literature. Ann Ital Chir. 2006;77(2):179–181.
- Markal N, Kurtay A, Velidedeoğlu H, Hücümenoğlu S. Malignant transformation of a giant proliferating trichilemmal tumor of the scalp: patient report and literature review. Ann Plast Surg. 1998;41(3):314–316.
- Casas JG, Woscoff A. Giant pilar tumor of the scalp. Arch Dermatol. 1980;116(12):1395.
- Weiss J, Heine M, Grimmel M, Jung EG. Malignant proliferating trichilemmal cyst. J Am Acad Dermatol. 1995;32(5 Pt 2):870–873.
- Takata M, Rehman I, Rees JL. A trichilemmal carcinoma arising from a proliferating trichilemmal cyst: the loss of the wild-type p53 is a critical event in malignant transformation. Hum Pathol. 1998;29(2):193–195.
Keywords
Malignant proliferating pilar tumor; Malignant proliferating trichilemmal tumor; Trichilemmal cyst; Proliferating pilar tumor
Cite this article
Jiang XL, Yang Y, Lei SR. Proliferating trichilemmal tumor of the scalp: a case report and literature review. Clin Surg J. 2022;3(3):1–6.
Copyright
© 2022 Shao-Rong Lei. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).