Abstract
A 42-year-old male who had a colonoscopy to investigate symptoms of altered bowel habit, low abdominal pain and fatigue. He went on to develop pain 8 hours after his procedure. At the time investigations were all normal, however, due to ongoing pain, two days later a CT scan demonstrated acalculous cholecystitis. He was not known to have gallbladder stones in the past. He had further investigations which did not confirm presence of gall stones. There have previously been 11 case reports of acute cholecystitis after colonoscopy in the literature. Here we discuss the cases which were admitted to our department and potential mechanisms for this link.
Introduction
Endoscopies are very commonly performed screening investigations. Whilst they are generally considered to be safe, there are a series of well recognised complications. The commonest of these are perforation and bleeding. A very rare but documented complication is the development of acute cholecystitis soon after colonoscopy. Previously there have 11 cases reported in the literature. All of these were after colonoscopies with patients developing symptoms within 72 hours of the investigation. Acute cholecystitis is a relatively common condition charachterised by fever, right upper quadrant pain and leukocytosis with associated gallbladder inflammation. It is a clinical diagnosis which is confirmed, most commonly by ultrasonography. Whilst the exact pathogenesis is not fully understood, it is thought to be caused by obstruction of the cystic duct (commonly by a gall stone) in combination with a further irritant to the gallbladder wall. Inflammatory mediators such as prostaglandins further propagate this inflammatory response.
Case Presentation
Our patient was a 42-year-old male with no significant past medical history, who had undergone a colonoscopy to investigate altered bowel habit, low abdominal pain and fatigue. His colonoscopy revealed a small sessile polyp in his caecum which was removed with cold biopsy forceps. He also had biopsies taken from his right colon and rectum. The histology of the polyp revealed a tubular adenoma with the other biopsies showing normal histology. He presented to ED later that day with generalised abdominal pain. Bloods on admission showed a WCC of 11.3 and a CRP of < 4 and normal liver function tests, a CT was performed to look for perforation but, revealed no abnormality. Two days later he re-attended the ED due to increasing abdominal pain. At that time he was pyrexial and WCC has risen to 19.4 with a CRP of 326. A repeat CT was performed. This showed acute cholecystitis. He also had an ultrasound scan to look for gall stones, however none were seen. He was treated with IV co-amoxiclav and discharged 6 days later. He had further investigation which did not show presence of gall stones. He has been well after discharge and follow-up of 6 months. He has been managed conservatively after further consultation and detailed discussion.
Discussion
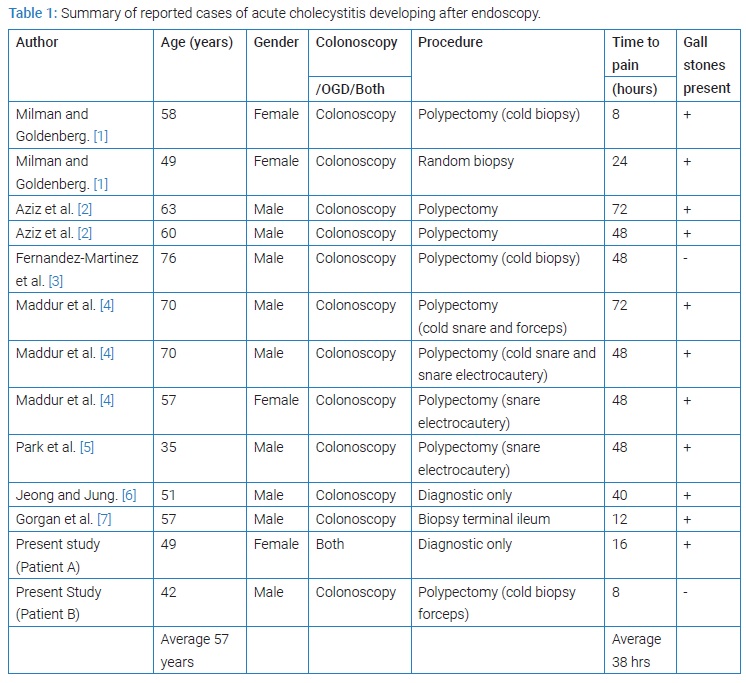
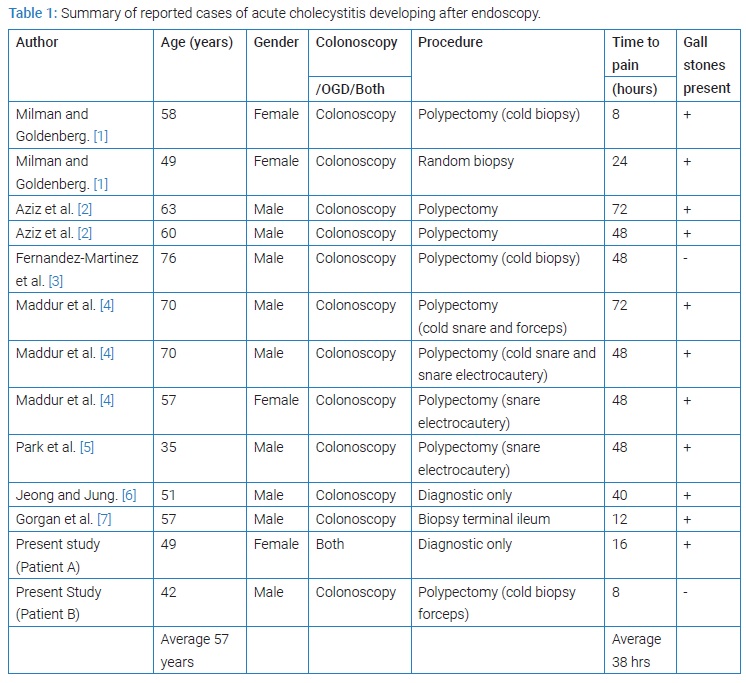
Previously there have been 11 reported cases in the literature of patients developing cholecystitis after colonoscopies (Table 1). There have been no reports of a link between OGDs and development of cholecystitis. Therefore, it seems most likely, that if there is a link with endoscopy, it is with colonoscopies. The time to symptoms varies from 8–72 hours with a mean time of 38 hours between colonoscopy and pain. 11 of the 13 patients were found to have gall stones. The majority had had an additional procedure performed, most commonly a polypectomy by varying modalities. Clearly, the sample size is too small to draw any meaningful conclusions. Several possible mechanisms have been proposed previously. One is that the use of bowel preparation leads to a state of relative dehydration, causing increased lithogenicity of the bile, bile stasis and gall bladder distention promoting local inflammation. We have also considered whether vigorous gas insufflation of the colon and manipulation of the scope around the hepatic flexure could cause physical irritation of the gall bladder. Finally, a transient bacteraemia associated with polypectomy/biopsy in the context of gas insufflation could inoculate the bile with bacteria and initiate the pathological process in an already predisposed patient. Given that some of these patients were being investigated for abdominal pain, it’s possible this was in fact an atypical presentation of their gall stone disease.
Learning Points/Take Home Messages
- Pain immediately after endoscopy should be considered as a possible perforation as this remains the most likely serious diagnosis.
- It is possible that by some as yet unclear mechanism, colonoscopies predispose patients to developing acute cholecystitis.This could also just be coincidence.
- Currently very few cases have been reported worldwide, however this may not be representative of the true prevalence if a link is not recognised by the treating clinician.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Acute cholecystitis; Endoscopy; Abdominal pain
Cite this article
Guru Raghavendra GK, Willows R. Acute cholecystitis after endoscopy – a review. Clin Surg J. 2022;3(3):1–3.
Copyright
© 2022 Gargeshwari Krishnamurthy Guru Raghavendra. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).