Benefits of Colonoscopy in Various iFOBT Cut-off Limits
* Mirwais Khan Dawar;
Anders Husted Madsen;
-
* Mirwais Khan Dawar: Department of General Surgery, Herning Hospital, Central Jutland, Denmark.
-
Anders Husted Madsen: Department of General Surgery, Herning Hospital, Central Jutland, Denmark.
-
Jun 10, 2022 |
-
Volume: 3 |
-
Issue: 2 |
-
Views: 2357 |
-
Downloads: 1506 |
Abstract
Introduction: Colorectal cancer (CRC) is one of the major causes of cancer deaths in developed countries. Population-based screening programs in various countries are implemented. CRC Screening Program was implemented in Denmark, aiming at detecting early cancer and precursors of cancer by screening citizens aged 50 years–74 years. Immunohistochemistry is used to detect occult hemoglobin in the feces. Various cut-off levels are used in different countries to guide and choose which patients should be offered a colonoscopy. The study aims to investigate the benefits of various cut-off limits for iFOBT in more detail.
Method and Design: This study is a retrospective cohort study and was conducted at the Department of Surgery at Herning Hospital. The study comprised a total of 2,676 patients aged 50 years–74 years in the years 2017 & 2018. Data were obtained from the Electronic Patient Journal (EPJ). For each of the participants in the study, parameters such as F hemoglobin level, symptoms in the form of bleeding, pain, weight loss, and stool changes were reviewed.
Findings and Discussion: The largest amount of polyp findings (637) is at the lowest cut-off limit (100–199). In total, there are 1,669 cases of polyp found through colonoscopies in a total of 2,676 citizens, which corresponds to 62.36%. Therefore, the total cancer findings at all colonoscopies are 136 out of 2,676 participants, corresponding to 5.08%.
Moreover, the study reveals that 55.96% of the overall cases are detected in the early stages, which is 1.96% higher than national-wide cancer findings in the early stages.
Conclusion: This study concludes that the quality of Screening Colonoscopy is higher at the Herning Hospital, as shown by the higher polyp detection rate. Moreover, the study considers it reasonable for a low cut-off limit to be used in Denmark, as 30% of all cancers and polyps are found in the lowest levels of F-hemoglobin.
Introduction
Colorectal cancer incidents are on the rise in Denmark and world wide as it’s the third most common cancer in the world now. In 2018 alone, 4,900 new colorectal cancer cases were registered in Denmark out of more than 1.8 million new cases that were registered worldwide [1,2]. Each year, approx. 2,000 patients die from colorectal cancer (KRC) in Denmark, which is among the most frequent cancer-related deaths in this country [3–5].
Given that colorectal cancer is a potentially curable disease, it is astonishing to see that the mortality rate in such cancer patients is considerably high. Studies have shown that the key reason is that the majority of patients are diagnosed in the later stages of cancer. This is because of the reason that colorectal cancer can be difficult to identify in the early stages, as the symptoms are often weak and may be reminiscent of common stomach problems. On the other hand, the symptoms often become very clear and specific in the later and advanced stages of cancer. The later the diagnosis is made, the worse the prognosis and survival for colorectal cancer patients. The expected 5-year survival rate is below 5% for stage IV cancer, while it is approx. 50% for Stage II-III and 75% for Stage I [3].
In 2014, the National Colorectal Cancer Screening Program was implemented in Denmark allowing all citizens aged 50 years–74 years being screening biannually. The screening program consists of screening feces for occult blood [6]. It is estimated that approx. 60% of colorectal carcinomas occur from conventional adenomas, 35% from serrated adenomas, and approx—5% as part of Lynch syndrome. Regardless of the histological origin of the polyps, polypectomy is likely to prevent the development of cancer [3].
The screening program uses a stool sample called the Immunochemical Faecal Occult Blood Test (iFOBT) to diagnose occult bleeding. In iFOBT, immunochemical techniques are used to identify traces of F-hemoglobin in the feces, indicating lower gastrointestinal bleeding. In Denmark, the cut-off limit is 100 μg /l, which signifies that the test is considered positive if the F-hemoglobin level in the feces is equal to or above 100 μg /l [7]. If the test is positive, a colonoscopy is offered [6]. Research suggests that the test will be positive for 5%–6% of the patients [8,9]. Moreover, the false-negative rate is 20%–30%, which means that a negative result from the iFOBT test does not exclude cancer [8,9]. However, other countries have different cut-off values than the one used in Denmark.
A low cut-off limit gives an increased sensitivity but a lower specificity [10]. Studies indicate that the iFOBT diagnostic performance is in several ways superior to the older Guaiac-FOBT test (gFOBT). These studies also show that the sensitivity is about 80%–90%, specificity above 90%, and a Positive Predictive Value (PPV) of 10% for the iFOBT test [9].
A cut-off limit for a positive i-FOBT test in Denmark is 100 μg/l. Citizens with higher hemoglobin levels in the stools will be offered a colonoscopy. However, the actual hemoglobin concentration in the stool is measured in each patient as long as the concentration does not exceed 1000 μg/l.
This study aims to investigate endoscopic findings in patients with different levels of occult hemoglobin. Therefore, this study will investigate different cut-off limits for iFOBT in more details and look into the benefits of having different iFOBT cut-off limits (100 μg/l or over).
Material and Methods
Study design: This study was conducted as a retrospective cohort study, in which recorded data from previous screening colonoscopies were used.
Setting and study population: This study was conducted at the Department of Surgery at Herning Hospital in the Central Jutland Region. All patients referred for screening colonoscopy from January 01, 2017 to December 31, 2018 were included in this study. The study population comprised 2,852 persons in age 50 years–74 years. All these individuals have participated in the screening program, have been tested positive by iFOBT, and been referred for colonoscopy screening.
Inclusion and exclusion criteria: This study’s inclusion and exclusion criteria were set to include the most appropriate participants. The inclusion criteria were as follows:
- All the participants should have completed a screening colonoscopy.
- Participants with incomplete colonoscopy because of tumor stenosis, the exclusion criteria were as follows.
- Participants who had a colonoscopy outside of the screening program.
- Participants who underwent regular control colonoscopies.
- Participants with IBD.
A total of 2,852 participants aged 50 years–74 years were referred for screening colonoscopy, out of which 176 persons were excluded from this study based on the exclusion criteria. Therefore, the remaining 2,676 people were included in the study. Data for the study was obtained from a special booking software that is used for screening colonoscopy and the Electronic Patient Journal (EPJ). For each of the participants in the study, parameters such as F hemoglobin level, symptoms in the form of bleeding, pain, weight loss, and stool changes were reviewed. Furthermore, it was investigated whether the patients received anti-coagulation medication. In addition, participants’ colonoscopy results, polyps, number and degree of dysplasia, as well as the size of the largest polyp, were looked at.
In contrast, hyperplastic and inflammatory polyps were not registered as polyp findings in the study. In addition, cancer and the different stages of cancer and colitis changes in the participants were examined. These parameters were recorded in Research Electronic Data Capture (REDcap), an online recording program for building and managing databases and online questionnaires [11]. The data was then analyzed in Stata (ver 15, StataCorp) [12]. The analysis results were used to design a statistical analysis across the different cut-off limits. In addition, the findings were also used for comparison with data from the screening database to examine and perform a quality contro lof screening colonoscopies at the department of Gastrointestinal Surgery at Herning Hospital.
Colonoscopy strategy: The IFOBT test is centralized to ensure uniformity and raise the quality of the test results. To ensure that there is a basis for a high level of competence, a colonoscopy strategy has been introduced where each laboratory must analyze a minimum of 25,000 samples annually. The regional screening secretariats are informed electronically about the stool test result and then send a written answer to the citizen.
Depending on whether the test is negative or positive, the citizen will receive a written answer.
After negative tests, the individual will be invited to participate in the screening program again in two years. In case of unsuitable samples, a new sample set is sent.
In the event of a positive answer, where blood has been found in the stool during the test, the concerned citizen will be summoned for a colonoscopy within 14 days after a positive test result.
A booklet that informs about the advantages and disadvantages of colonoscopy and information that detecting blood in feces is not necessarily synonymous with cancer is also sent to the citizen.
Ethics and approvals: According to current guidelines (Kilde) for quality control study, the consent and approval were obtained from the ward and hospital management and the Danish data protection agency. According to these guidelines, it was not necessary to ask for the consent of the participants in person, nor was it necessary to seek approval from the ethics committee.
Results
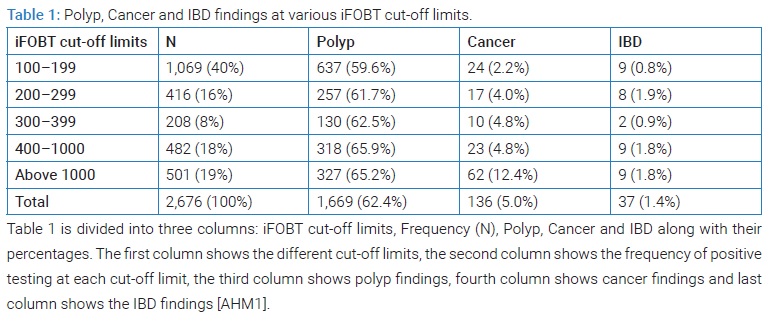
As seen in (Table 1), all polyp except hypoplastic polyps is included. Furthermore, it shows that the largest amount of polyp findings (637) is at the lowest cut-off limit(100–199) but the lowest percentage (59.6%). Moreover, at the cut-off limit of 300–399, the polyp findings (130) are at the lowest but a considerably higher percentage (62.5%). However, the percentage differences are not of much concern at this point, considering the large differences in the amount of poly findings at different cut-off limits. In total, there are 1,669 cases of polyp found through colonoscopies in a total of 2,676 citizens, which corresponds to 62.4%.
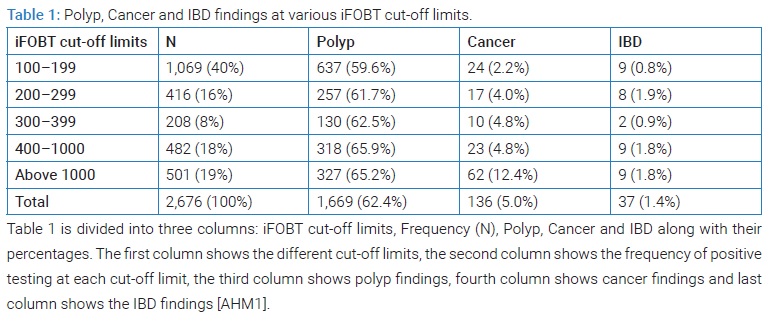
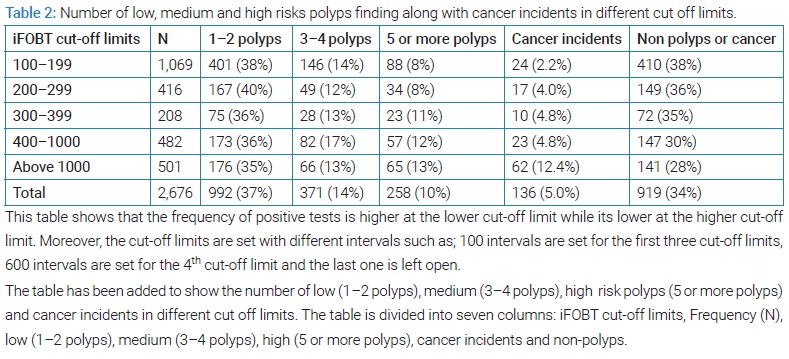
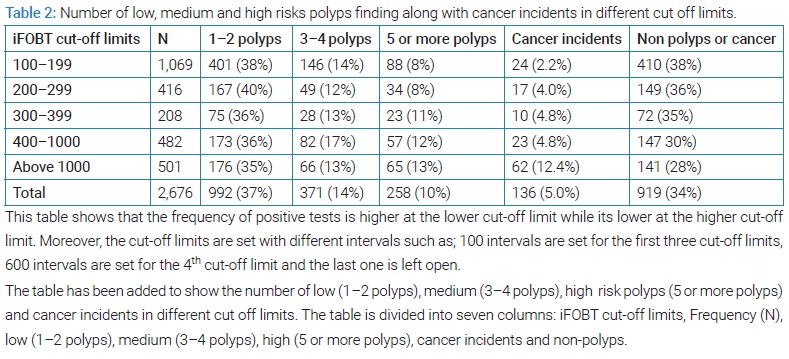
Looking at (Table 2), It is clear that the cut-off limit of 100–199 shows the lowest percentage (2.2%) of cancer incidents while the cut-off limit of above 1,000 shows the highest percentage (12.4%) of cancer incidents. Moreover, the total cancer findings at all colonoscopies are 136 out of 2,676 participants, corresponding to 5.08%. Furthermore, it can be deduced that out of 2,676 positive tests for F-hemoglobin, low polyps (1–2) have the highest percentage (37%), while high polyps (5 or more) have the lowest percentage (10%). The medium polyps (3–4) are found to have a 14% presence.
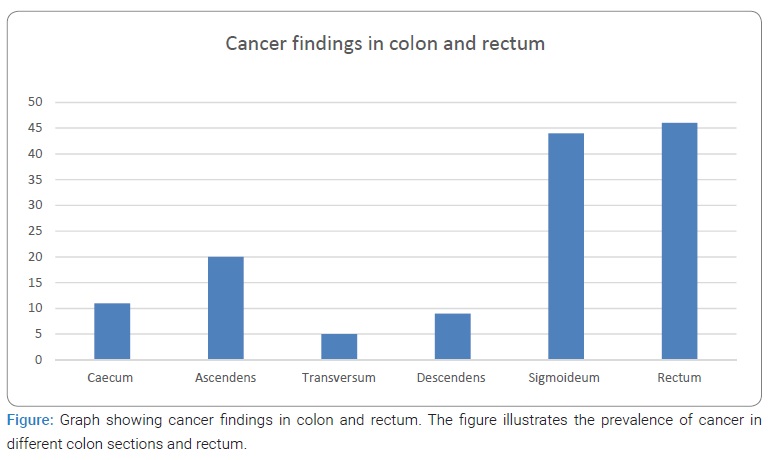
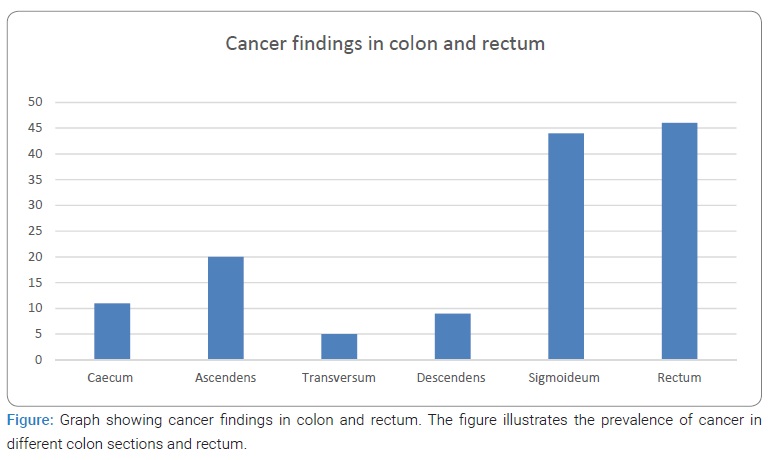
The highest found of cancer was detected in the sigmoid colon (32,3%) and rectum (33,8%), and the lowest amount of cancer was detected in the transversum, which was at 3,6% (Figure).
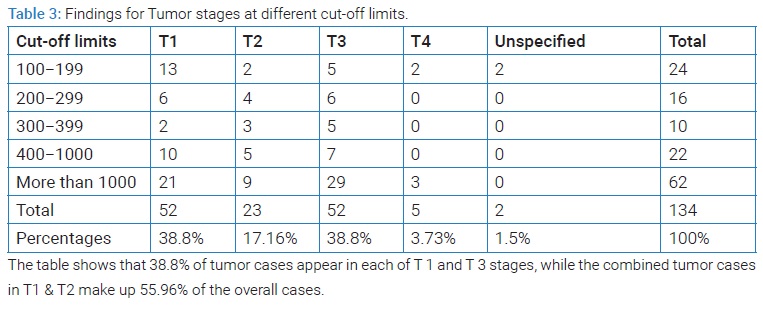
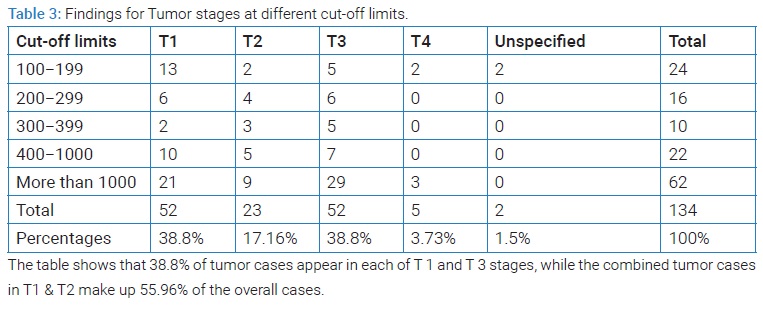
Tumor findings were significantly higher in T1 and T3 (Table 3). Compared to the other stages, the appearance of tumor cases in each T1 and T3 was 38%, while the combined tumor cases in T1 & T2 make up 55.96% of the overall cases.
Discussion
In the present paper, we present data on endoscopic findings in patients with different hemoglobin concentrations in the stool. The study is based on data collected over the period of two years using the Danish Colorectal Cancer Screening Database. Also, the high participation rate of people in this study adds more credibility to the results as all citizens aged 50 years–74 years were invited to contribute. With a data collection of two years period, statistics on the quality of sensitivity and specificity in various cut-off limits regarding the iFOBT test were compiled. Moreover, the study shows that the iFOBT test is more sensitive at low cut-off limits. As shown in (Table 1), 40% of all the tested participants have been positive at the cut-off limits of 100 μg/l–199 μg/l; out of the 40% positive participants, 60% were positive for colonoscopies.
(Table 1) also shows that there is a large difference between the positive detection rates at various cut-off limits. For instance, at the low cut-off limit (100 μg/l–199 μg/l), the positive iFOBT is 40%, while the positive iFOBT rate declines at the higher cut-off limit. It also shows that the polyp detection rate at the low cut-off limit of 100 μg/l–199 μg /l is 59.6%, while it is around 65% at the higher cut-off limits. This is also consistent with the fact that specificity increases at higher cut-off limits. Although a higher detection rate (65%) is seen at the high cut-off limits compared to the lower one, it is still considered an advantage to measure at the low cut-off limit of 100–199. This is because of the reason that one will probably overlook many positive patients at the high cut-off limits who would otherwise have been detected at the lower one. Therefore, it can be stated that the lower the cut-off limit, the higher the positive detection rate. However, this does not mean that this is necessarily an advantage because if we get more positive results at low cut-off limits, this could mean that more false positives have been detected. On the other hand, if we set the cut-off limit too high, the chance is that we will miss many positive tests. There foregone must be a balance between sensitivity and specificity.
This is also consistent with the study by Chen et al. [13], which considers the optimal cut-off value to be 100 μg/l. Moreover, another study by Sisse Helle Njor et al. [14] finds the optimal cut-off value to be between 80 μg/l–350 μg/l, where about 16–14 coloscopies will be needed to find one cancer. The study also mentions that if the cut-off value is set too low, such as 45 μg/l, this will put a big burden on the healthcare system since this would cause too many colonoscopies to find one cancer.
The report from the Danish Colorectal Cancer Group Database [8] and other publications [8,10,15] indicate that the quality of screening colonoscopy for polyp findings at Herning Hospital is high. Also, the Danish Health and Medicines Authority’s monitoring report 8 states that nationwide, 33% of medium and high-risk polyps were found by colonoscopy in 2017. Moreover, this study shows that polyps findings at Herning Hospital are 62.4% (table 2-results section) compared to the findings in the monitoring report, which suggests that the polyp detection rate at Herning Hospital is 41%. The reason for this difference in polyps’ findings detection rates could be due to various factors. Such as this study is based on data from both 2017 and 2018, while the Danish Health and Medicines Authority’s monitoring report only includes data from 2017. Moreover, the monitoring report only contains medium and high-risk polyps, while this study contains low, medium, and high-risk polyps. We also assume that since this study includes all polyps’ sizes, including the small polyps, which do not necessarily have significance, the monitoring report may not have included all polyps’ sizes, hence explaining the difference in polyps’ findings. This has also been taken into account in the 2018 report, where instead of including only medium and high-risk polyp, a more generally desired level of polyp detection rate of > 50% has been used.
Moreover, the cancer detection rate at Herning Hospital is 5.08% (table 3-results section), while the acceptable limit in the monitoring report from 2018 is > 4% [15]. Therefore, the cancer findings of this study seem to be satisfactory in relation to the acceptance limit from the 2018 monitoring report. While the acceptable limit in the monitoring report of 2017 was 5.40%. A possible reason could be the general declining trend in cancer development in elderly citizens aged 50 years plus [1], which may have been the reason why a larger finding of cancer has not been achieved as per the general acceptance limit. This tendency is also consistent with the 2018 monitoring report, where the acceptance limit has dropped to > 4% [15].
We also assume that although the age limits of the participants in both studies are 50 plus, there may have been a different number of participants at different age intervals. For example, such different numbers of participants in the age group 70 years–74 years plus, who are probably at greater risk of colon cancer than those aged 50 years–60 years, may have been included in the two studies. Therefore, there may be some deviation in the results if one has a larger group of those included aged 50 years–60 years compared to a group with participants 70 years–74 years plus.
Conclusion
Denmark’s low cut-off limit (100 μg/l) seems reasonable to maintain, as 30% of all cancers and polyps are found in the lowest levels of F-hemoglobin. In addition, it can be concluded that the quality of screening colonoscopy in the Herning Hospital is high compared to the national level. Moreover, the Herning Hospital achieves a 55.96% cancer detection in the early stages compared to the national percentage of 54%.
Conflict of Interest
Mirwais Khan Dawar and Anders Husted Madsen is both consultant surgeon at hospital unit west, Herning hospital, and have no conflict of interest in connection with this study.
References
- Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–1953.
- Hawk ET, Limburg PJ, Viner JL. Epidemiology and prevention of colorectal cancer. Surg Clin North Am. 2002;82(5):905–941.
- DCCG. Nationale retningslinier for diagnostik og behandling af kolorektal cancer. Primaer Forebyggelse Af Kolorektalcancer. Aarhus: DCCG; 2019.
- Patai ÁV, Molnár B, Tulassay Z, Sipos F. Serrated pathway: Alternative route to colorectal cancer. World J Gastroenterol. 2013;19(5): 607–615.
- Snover DC. Update on the serrated pathway to colorectal carcinoma. Hum Pathol. 2011;42(1):1–10.
- Sundhedsstyrelsen. The general covid-vaccination programme in Denmark has been paused for the time being. It is still possible to get vaccinated. Denmark: Sundhedsstyrelsen; 2020.
- Kraeftscreening. Screening for bowel cancer. Denmark: Kraeftscreening; 2020.
- Regionernes Kliniske Kvalitestsudviklings Program (RKKP). Dansk tarmkraeft screenings database, Årsrapport 2017,Nationale paevalens screeningsrunde. 2018.
- Screening for tarmkræft i Vejle og Københavns Amter Tværgående evaluering af pilotprojekter. Region Hovedstaden. 2020.
- Aniwan S, T Ratanachu Ek, Pongprasobchai S, Limsrivilai J, Praisontarangkul OA, Pisespongsa P, et al. The optimal cut-off level of the fecal immunochemical test for colorectal cancer screening in a country with limited colonoscopy resources: A multi-center study from Thailand. Asian Pacific J Cancer Prev.2017;18(2):405–412.
- REDCap. How REDCap is being used in response to COVID-19. USA: REDCap; 2020.
- STATA. Why Stata. Texas: STATA; 2020.
- Chen LS, Liao CS, Chang SH, Lai HC, Hsiu-Hsi Chen T. Cost-Effectiveness Analysis for Determining Optimal Cut-off of Immunochemical Faecal Occult Blood Test for Population-Based Colorectal Cancer Screening (KCIS 16). J Med Screen. 2007;14(4):191–199.
- Njor SH, Andersen B, Friis-Hansen L, de Haas N, Linnemann D, Nørgaard H, et al. The optimal cut-off value in fit-based colorectal cancer screening: An observational study. Cancer Med. 2021;10(5):1872–1879.
- Dansk Tarmkraeftscreenings database Årsrapport. 2018.
Keywords
Benefits of colonoscopy; Colorectal cancer; Screening colonoscopy; iFOB test; iFOBT; iFOBT cut-off limits
Cite this article
Dawar MK, Madsen AH. Benefits of colonoscopy in various iFOBT cut-off limits. Clin Surg J. 2022;3(2):1–6.
Copyright
© 2022 Mirwais Khan Dawar. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).