Malignancy Rates and Predictors of Malignancy in Bethesda III and IV Classes: A Retrospective Study
* Clara Leal;
Santos C;
Fernandes U;
Guidi G;
Martins D;
Vieira B;
Gaspar J;
Pinto-de-Sousa J;
-
* Clara Leal: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Santos C: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Fernandes U: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Guidi G: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Martins D: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Vieira B: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Gaspar J: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Pinto-de-Sousa J: Department of General Surgery, Centro Hospitalar De Trás-Os-Montes E Alto Douro, Vila Real, Portugal.
-
Jun 09, 2022 |
-
Volume: 3 |
-
Issue: 2 |
-
Views: 6646 |
-
Downloads: 2227 |
Abstract
Background: The optimal approach for Bethesda III and IV classes is not yet defined, largely because the malignancy rate remains unknown. This study aimed to determine the rate of malignancy and to find any possible association between features of Bethesda categories III and IV patients and the presence of malignancy.
Methods: The electronic medical records of 335 consecutive cases classified as Bethesda III–VI, selected from the total of 711 cases, were reviewed, and the following parameters were analyzed: age and gender of the patients, location of the largest nodule, and its FNA cytology result prior to surgery, a surgical technique performed, size of the largest nodule measured at the preoperative ultrasound and pathology surgical specimen evaluation, and postoperative pathological diagnosis. Parameters were compared within BIII and BIV Bethesda classes and between Bethesda III/IV and V/VI groups.
Results: In the present study, malignancy rates of 21.2% for the Bethesda III category and 15.2% for the Bethesda IV category were observed. There was a statistically significant association between the postoperative malignancy diagnosis and age (60.2 vs. 56.0 years, p = 0.004) and the size of the largest nodule at ultrasound (2.00 vs. 1.80 cm, p = 0.001). No other features were associated with malignancy prediction.
Conclusions: The malignancy rate of Bethesda III and IV categories observed in this series justifies the demands of an optimized approach, which cannot be established based on the current predictors available only. Further studies are needed to build a tailored approach to avoid unnecessary surgery and consequent morbidity.
Abbreviations
FNA: Fine-Needle Aspiration; NIFTP: Non-invasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features; BIII: Bethesda Category III; BIV: Bethesda Category IV; AUS/FLUS: Atypia, or Follicular Lesion of Undetermined Significance; FN/SFN: Follicular Neoplasm or Suspicious for Follicular Neoplasm; CHTMAD: Centro Hospitalar de Trás-os-Montes e Alto Douro; RLN: Recurrent Laryngeal Nerve; ROM: Risk of Malignancy; BS: Bethesda System.
Introduction
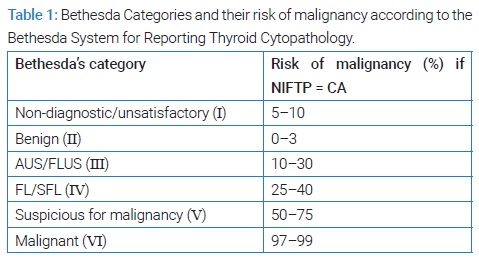
Diagnosis of thyroid nodules in adulthood has been increasing over the years due to the growing use of sensitive imaging in clinical practice, improving detection [1–5]. In an ultrasound examination, the prevalence is up to 50% in female and 30% in male patients [6]. Even though most of these lesions are benign, 5% to 15% turn out to be malignant [2,7,8], which enhances the importance of studying these nodules to exclude the possibility of cancer. In this sense, ultrasound-guided fine-needle aspiration (FNA) has been used as part of the preoperative study of suspicious thyroid nodules to stratify cancer risk [1,9]. The Bethesda System for Reporting Thyroid Cytopathology includes six categories and recommends the subsequent approach to each one of them (Table 1), therefore avoiding unnecessary diagnostic thyroidectomies [1,10].
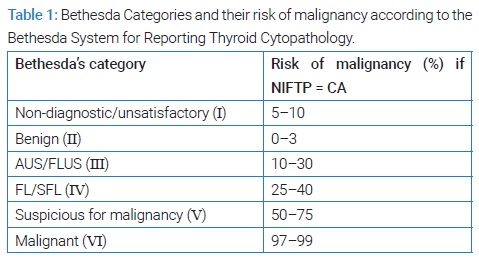
The risk of malignancy of Bethesda categories III and IV ranges from 10% to 30% and 25% to 40%, respectively, considering non-invasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) as part of the group of malignancy [10,11]. Bethesda category III (BIII) includes cytopathologic findings which are not easily defined as benign, suspicious, or malignant [12], the so-called “atypia of undetermined significance” or “follicular lesion of undetermined significance” (AUS/FLUS). These nodules can be managed either with clinical follow-up, performing another FNA or molecular testing, or surgery considering the clinical and/or ultrasound risk features [10]. Bethesda category IV (BIV) represents “follicular neoplasm” or “suspicious for a follicular neoplasm” (FN/SFN), and it implies, ad minimum, a diagnostic lobectomy, given that a follicular carcinoma cannot be excluded based on cytomorphological analysis [10,12]. Thyroid surgery is not exempt from risks, including serious complications such as recurrent laryngeal nerve lesion or hypocalcemia when total thyroidectomy is performed. Therefore, controversy in the clinical approach of these categories remains, mainly because of the limited role of FNA in diagnosing some malignancy features such as capsular and/or lymphatic and/or vascular invasion and the different malignant rates among the literature [11].
This study aimed primarily at knowing the Bethesda categories III and IV malignancy rates at our institution. The secondary endpoint was to evaluate any possible associations between features of Bethesda categories III and IV patients and the presence of malignancy.
Material and Methods
This study is based on the retrospective analysis of a prospective database of patients admitted for surgery due to thyroid nodule pathology, from January 2013 to December 2020, in Centro Hospitalar de Trás-os-Montes e Alto Douro (CHTMAD), a Portuguese Hospital. Seven hundred eleven patients with nodular thyroid pathology were treated at the institution during this period. A total of 335 consecutive cases, classified as Bethesda III, IV, V, and VI, were included in the study. Patients younger than 18 years old, cases without records of FNA biopsy prior to surgery, and those without postoperative histopathological results available were excluded from the study. In addition, the study did not include Bethesda I and II cases (n = 376).
The electronic medical records were reviewed, and the following parameters were analyzed:
- Age and gender of the patients.
- Location of the largest nodule and its FNA cytology result prior to surgery.
- Surgical technique performed (lobectomy with isthmectomy/hemithyroidectomy, total thyroidectomy, or thyroid totalization).
- Size of the largest nodule measured at the preoperative ultrasound and pathology surgical specimen evaluation.
- Postoperative pathological diagnosis.
Concerning surgical technique performed, thyroid totalization cases were included in the “hemithyroidectomy” category. In addition, common or worrisome postoperative complications in thyroid surgery were evaluated, namely, transient and permanent hypocalcemia, transient dysphonia, permanent Recurrent Laryngeal Nerve (RLN) injury, and cervical hematoma. The minimum follow-up period for patients who experienced complications after surgery was six months. Whenever hypocalcemia persisted after six months despite replacement therapy, it was considered permanent hypocalcemia. The category “transient dysphonia” included patients with clinical evidence of dysphonia that did not persist beyond six months after surgery. Some cases of dysphonia were subject to further evaluation by Otorhinolaryngology, Physical Medicine, and Rehabilitation, with proven immobility of the vocal fold, which led to speech therapy. Upon re-evaluation, such immobility proved temporary, given that laryngoscopy showed a return to normal mobility. Permanent RLN injury was considered whenever there was clinical evidence (one case of persisting dysphonia, without an electronic record of laryngoscopy) or the laryngoscopy/ nasolaryngofibroscopy showed compromised mobility of vocal fold persisting beyond six months after surgery. The occurrence of cervical hematoma was considered a postoperative complication if longer in-hospital stay, re-admission, or surgical re-intervention were required.
FNA cytopathology results were cataloged according to the Bethesda System [10].
The study’s primary objective was the evaluation of the malignancy rate of the Bethesda categories III and IV at our institution. The secondary endpoint was to study possible associations between Bethesda categories III and IV features and the presence of malignancy. Considering the study’s aims, cases were cataloged into two groups: Bethesda III and IV (III/IV) group; and Bethesda V and VI (V/VI) group.
Statistical analysis was performed using IBM SPSS Statistics software, version 27. Statistical significance was indicated by p ≤ 0.05. Categorical variables are presented as absolute (n) and relative (%) frequencies. Continuous variables are presented as means and standard deviations, or median and first and third quartiles, according to normal distribution tests (skewness and kurtosis or Shapiro-Wilk test). In addition, when applicable, Chi-square or Fisher’s Exact tests were performed to check for the association between two qualitative variables. t-Student test for independent samples or Mann-Whitney test were implemented to compare quantitative variables between two groups, when applicable.
Results
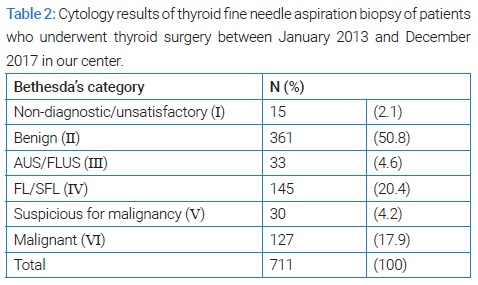
From January 2013 to December 2020, a total of 711 cases of nodular thyroid pathology were admitted to the institution for treatment. A sample of 335 consecutive cases classified as Bethesda other than I and II were included in this study. Of all the thyroid FNAs performed, 33 (4.6%) were classified as AUS/FLUS and 145 (20.4%) as FN/SFN, Bethesda System grades III and IV, respectively (Table 2).
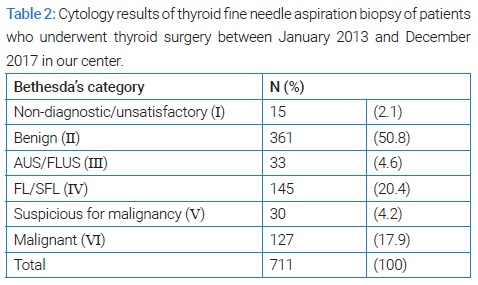
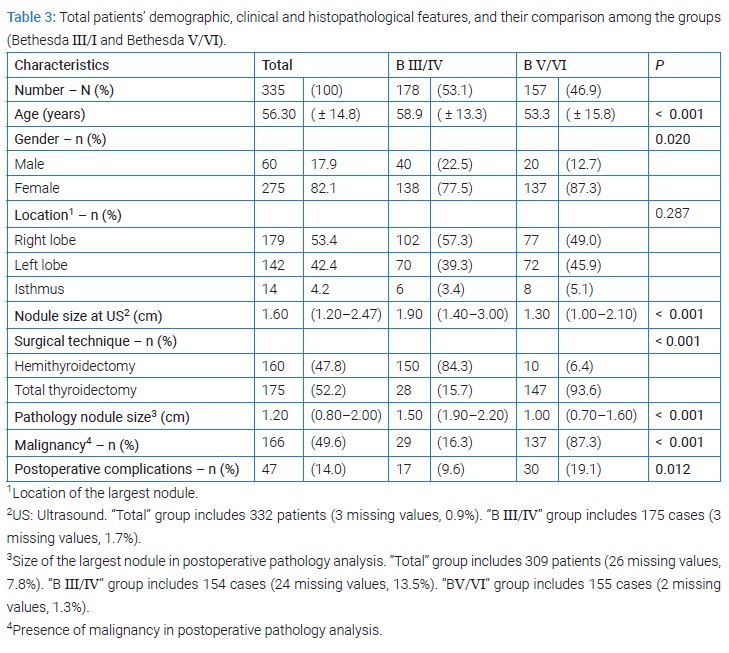
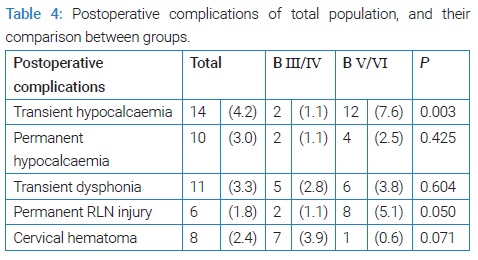
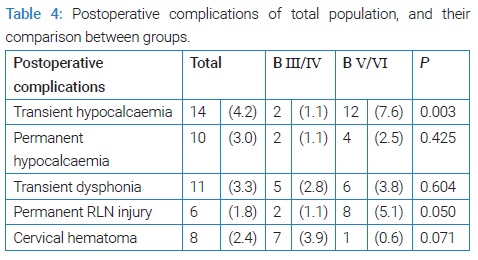
(Table 3) documents the features of the total population and the distribution of parameters of the two groups created in the study according to the Bethesda classification. The mean age of the total population was 56.3 ( ± 14.8) years, and the female gender prevailed (82.1% vs. 17.9%) (Table 3). FNA results were classified into nondiagnostic/unsatisfactory (2.1%), benign (50.8%), AUS/FLUS (4.6%), FL/SFL (20.4%), suspicious for malignancy (4.2%) and malignant (17.9%) (Table 2). Total thyroidectomy was performed in most of the patients (52.2%). Postoperative diagnosis of malignancy occurred in 166 patients (49.6%), the mean size of the largest nodule at ultrasound was 1.60 centimeters (cm), and the median size of the largest nodule at pathology evaluation was 1.20 cm (Table 3). Transient hypocalcemia was the most common postoperative complication observed (4.2%) (Table 4).
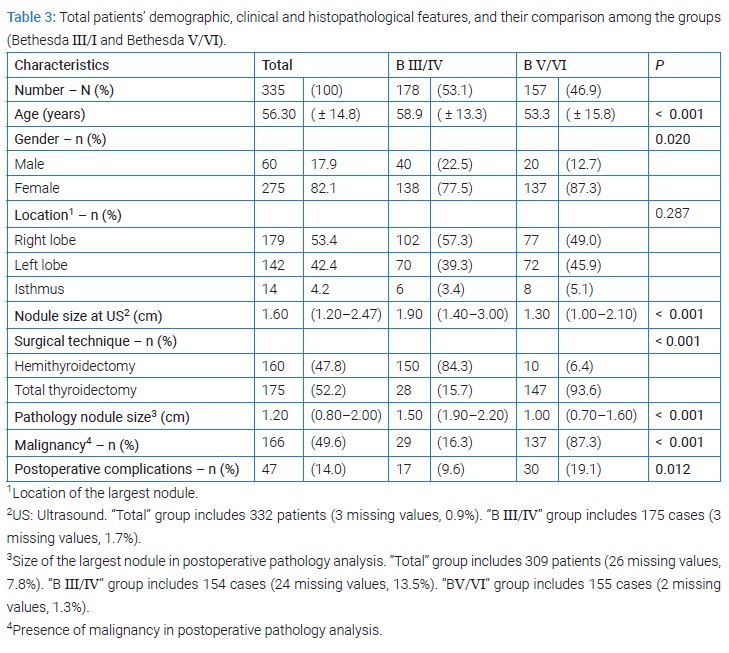
The distribution of cases between the two groups considered documents significant differences according to age (p < 0.001), gender (p = 0.020), size of the nodule (p < 0.001), surgical technique p < 0.001), rate of malignancy (p < 0.001) and postoperative complications (p = 0.012).
The age of patients cataloged as BIII/IV (58.9 years) was higher than those belonging to the group of BV/VI. The relative frequency of male patients in the group Bethesda III/IV (22.5%) was higher than that of the other group (12.7%) (p = 0.020). The size of Bethesda III/IV cases nodules at preoperative ultrasound (1.90 cm) was higher than that of the other group (1.30 cm) (p < 0.001) as well as was the size of the largest nodule at postoperative surgical specimen examination (1.50 vs. 1.00 cm, respectively) (p < 0.001). The relative frequency of postoperative diagnosis of malignancy in the Bethesda III/IV group (16.3%) was lower than that of the other group (87.3%) (p < 0.001). The percentage of Bethesda III/IV patients submitted to total thyroidectomy (15.7%) was lower than that observed in the other group of patients (93.6%).
No significant differences were observed in the comparison of postoperative complications between the two groups considered but in the case of transient hypocalcemia and permanent RLN injury (Table 4), which was less frequent in Bethesda III/IV cases than in the other group (1.1% vs. 7.6% and 1.1 vs. 5.1%, respectively).
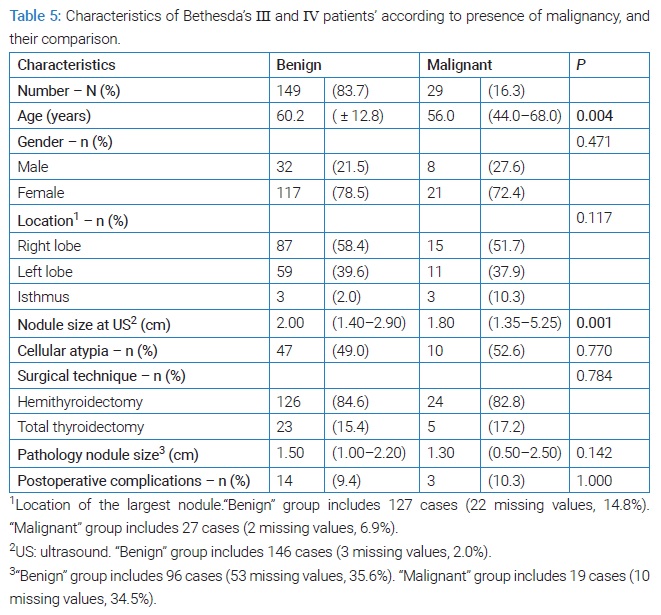
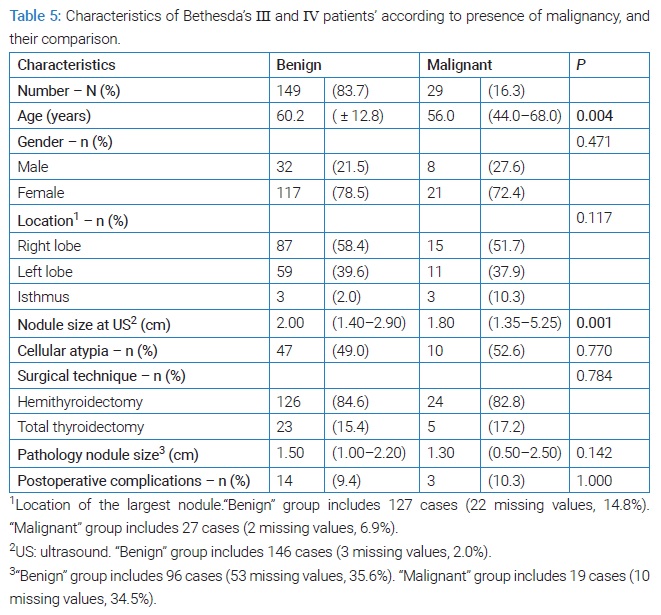
In this series, the malignancy rate in Bethesda III and IV cases was 16.3%. (Table 5) summarizes the distribution between Bethesda III and IV cases according to the presence of malignancy. Significant differences were observed according to the age of patients (p = 0.004) and the size of nodules evaluated by ultrasound (p = 0.001). In this subgroup of cases, the mean age of patients with benign nodules (60.2 years) was higher than that of malignant (56.0 years). In addition, the mean size of benign nodules evaluated by ultrasound (2.00 cm) was higher than that observed in malignant cases (1.80 cm). No significant differences were observed according to the other parameters evaluated.
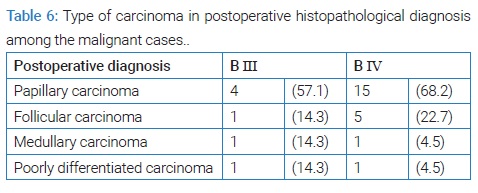
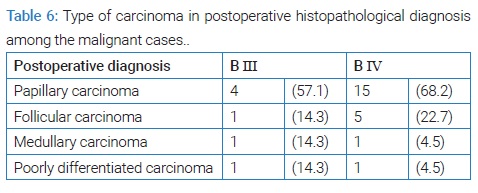
Regarding the ultimate type of malignant lesions in patients previously diagnosed with indeterminate cytology Bethesda III and IV categories, papillary carcinoma was the most reported cancer type (57.1% and 68.2%, respectively). In the BIV group, follicular carcinoma followed 22.7% of the cases (Table 6).
Discussion
The increasing use of ultrasound and FNA has led to increased detection of thyroid nodules, and therefore the frequency of indeterminate cytology has been rising as well [13]. However, indeterminate cytology represents a “gray zone” of thyroid cytology [14], and its management remains a challenge for clinicians. On the one hand, the inability to distinguish benign from malignant in cytology samples often results in an increased surgical indication. However, on the other hand, patients are being overexposed to thyroid surgery morbidity because 70% to 80% of these nodules are diagnosed as benign at surgical specimen histopathological analysis [14].
In the present study, the overall malignancy rate was 26.6% (n = 189/711), which is higher than the values mentioned above in some other series (5% to 15%) [2,7,8]. For the BIII group, a malignancy rate of 21.2% was observed in this series, which is in line with the risk of malignancy (ROM) reported in the Bethesda System (BS) [10] (10% to 30%). On the other hand, for the BIV group, the malignancy rate observed was 15.2%, which is a lower value than the ROM reported in the BS (25% to 40%) [10].
Differences in subjective classification can explain the variation of malignancy rates for each BS category in the literature [15–17]. In fact, the cytologic and architectural pattern changes seen in AUS/FLUS category are not easily defined as benign or malign [12]. Common benign condition ith category III [18]. In addition, intrathyroidal parathyroid adenomas can mimic a lesion suspicious for follicular neoplasm [18].
Bongiovanni et al. considering Bethesda categories IV–VI, compared FNA cytology with postoperative histopathologic results and identified a diagnostic accuracy and a positive predictive value of 68.8% and 55.9%, respectively [17]. When the authors added Bethesda category III to this analysis, the same values decreased to 60.2% and 46.9% [17]. There may be an overuse of the AUS/FLUS category in our institution.
In this series, there was a statistically significant association between the size of the largest nodule at the preoperative ultrasound and belonging to the Bethesda III/IV or BV/VI groups (1.90 cm vs. 1.30 cm, p < 0.001), as well as for the size of the largest nodule at postoperative surgical specimen examination (1.50 vs. 1.00 cm, p < 0.001).
Bethesda V/VI group displayed a statistically significant association with the presence of malignancy (16.3% vs. 87.3%, p < 0.001), as expected, because of higher risks of malignancy in these Bethesda categories [10].
The occurrence of transient hypocalcemia showed a statistically significant association with the BV/VI group (1.1% vs. 7.6%, p = 0.003). Higher relative frequency of malignant cases (fixed lesions, possible invasion of adjacent structures) and total thyroidectomies in this group can lead to more extensive and/or harder dissection, leading to this injury.
When the Bethesda III/IV group was isolated and analyzed, the mean age was slightly higher, the nodule size was smaller than those reported by other authors, and gender distribution was similar to other studies. In the current study, the mean age was 58.9 (± 13.3) years, 77.5% of the 178 patients were female, the median nodule size on ultrasonography was 1.90 (1.40–3.00) cm, and the median nodule size on the surgical specimen was 1.50 (1.00–2.20) cm. Alexander et al. analyzed a total of 378 patients with indeterminate cytology (BS categories III, IV, and V) and subsequent surgery. They reported a median age of 51.8 (range 19–85) years, a female dominance (77.8% vs. 22.2%), and a median nodule size on ultrasonography of 2.3 (range 0.75–10.3) cm [19]. Castro et al. analyzed 462 patients with suspicious cytological diagnoses (including BS categories III, IV, and V). They showed a mean age of 53.7 (± 15.2) years and a mean nodule size on ultrasonography of 2.8 (± 1.7) cm [7]. Bayrak et al. reported a mean age of 52.5 years and female prevalence (85.2% of the 155 patients classified as BS III and IV categories) [11]. Cavalheiro et al. studied a total of 582 patients and showed a higher percentage of the female gender than the previous studies (89.6%), and the mean age at diagnosis was 54 years [15].
Some clinical features such as age, gender, nodule size, and history of exposure to radiation to the head and neck have been recognized as malignancy predictors [7]. A statistically significant association between age and the postoperative diagnosis of malignancy in the Bethesda III/IV patients (60.2 ± 12.8 vs. 56.0 (44.0–68.0) years, p = 0.004) was observed too. Although some authors did not find age as a predictor of malignancy [7,20], Scerrino et al. observed that the mean age was significantly different between malignant and benign groups (52 vs. 58 years, p < 0.001) and showed that age > 60 years seemed to be protective against malignancy [21]. Other authors reported that, in studies addressing only Bethesda IV cases, patients older than 50 or 40 years old had a higher risk of malignancy [14,22,23].
In the present study, there was a statistically significant association between the size of the largest nodule on ultrasonography and the presence of malignancy (2.00 vs. 1.80 cm, p = 0.001). The value of nodule size remains controversial as a predictor of malignancy [14]. In fact, some authors found that a larger size was associated with malignancy [14,20,22,24]. Castro et al. reported that a smaller nodule size measured by preoperative ultrasound was associated with ROM [7], and Rago et al. studied 505 patients with follicular and Hurthle cell thyroid lesions and did not find an increase in ROM to nodules bigger than 3 cm concerning those smaller than 3 cm [25].
In this series, no significant statistical difference between the male gender and the presence of malignancy in Bethesda III/IV was observed, which is in agreement with some other studies [21,22,24]. In contrast, Tuttle et al. and Baloch et al. observed that the male gender was associated with malignancy [14,20,23].
No significant differences were observed concerning cytologic atypia in this study, as opposed to Teixeira et al. The latter studied 229 cytology samples classified as follicular neoplasms and reported a significant difference between the presence of cytologic atypia and malignancy (12.5% vs. 33.3%, p = 0.02) [26].
Among the malignant lesions, papillary carcinoma was the most common diagnosis (57.1% in the BIII group and 68.2% in the BIV group). Bayrak et al. observed that from the malignant lesions, 81.5% of the AUS/FLUS and 69.2% of the FN/SFN were papillary carcinomas [11].
Concerning surgical complications, transient and permanent hypocalcemia occurred in 4.2% and 3.0% of BIII–VI patients who underwent thyroid surgery, respectively. Rosato et al. reported that 8.3% of the 14934 patients with operated on thyroids experienced transient hypocalcemia, and 1.7% had definitive hypocalcemia [27]. Eleven patients out of 335 (3.3%) experienced transient dysphonia, and six (1.8%) showed evidence of permanent RLN injury. Iyomasa et al. studied 151 patients submitted to thyroidectomy and reported temporary paralysis of the vocal folds secondary to recurrent laryngeal nerve injury in 21.2% of all patients and persisting injury after six months in 6.6% of cases [28]. Rosato et al. reported relative frequencies of 2.0% to RLN monoplegia, 1.0% to definitive lesion, and 0.4% to diplegia [27]. Cervical hematoma occurred in 2.4% of all patients (n = 8/335). Rosato et al. reported a percentage of 1.2% of all patients for intra and postoperative hemorrhage occurrence [27]. Bergenfelz et al. observed that 76 patients (2.1% of all 3660 patients) were operated on due to re-bleeding with compressive hematoma [29].
Extensive analysis of postoperative complications is outside the scope of the present study. However, it is important to note that they are not so uncommon, and it is crucial to be aware of their frequency when deciding the therapeutical approach for each patient.
Limitations of the current study include its retrospective design, with data collected prospectively by different physicians. The same physician reviewed all patients’ medical records and data included in this study to minimize heterogeneity. Due to the nature of the study, the authors cannot guarantee that the biopsied nodule was the same on pathology evaluation diagnosing malignancy; and it was not possible to define if some cases of dysphonia and RLN injury occurred as postoperative complications or if they were already present preoperatively. Moreover, we studied patients who underwent surgery and did not analyze Bethesda III and IV patients who underwent medical follow-up. To know if it is safe to adopt a wait and see strategy in these patients, it would be important to compare the outcomes of both arms (patients who underwent surgery vs. wait and see).
Summing up, this study provides further information on malignancy rates among Bethesda III and IV categories and patient features associated with the presence of malignancy in a study conducted with 335 patients. First and foremost, our research contributed to a better understanding of our institution rates and allowed us to compare them with other centers.
Conclusion
In the present study, a malignancy rate of 21.2% for the Bethesda III category and 15.2% for the Bethesda IV category were observed. In addition, there was a statistically significant association between the postoperative malignancy diagnosis and the age and size of the largest nodule at the ultrasound. Further studies are needed to determine malignancy predictors, including ultrasound features and molecular tests, to optimize preoperative risk stratification in Bethesda III and IV categories, thus being able to tailor the approach to patients better, avoiding unnecessary surgery and its morbidity when possible.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Pasha HA, Dhanani R, Mughal A, Ahmed KS, Suhail A. Malignancy rate in thyroid nodules with atypia or follicular lesion of undetermined significance. Int Arch Otorhinolaryngol. 2020;24(2):e221–e226.
- Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133.
- Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140(4):317–322.
- Dean DS, Gharib H. Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab. 2008;22(6):901–911.
- Durante C, Costante G, Lucisano G, Bruno R, Meringolo D, Paciaroni A, et al. The natural history of benign thyroid nodules. JAMA. 2015;313(9):926–935.
- Papini E, Monpeyssen H, Frasoldati A, Hegedüs L. 2020 European thyroid association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. Eur Thyroid J. 2020;9(4):172–185.
- Castro MR, Espiritu RP, Bahn RS, Henry MR, Gharib H, Caraballo PJ, et al. Predictors of malignancy in patients with cytologically suspicious thyroid nodules. Thyroid. 2011;21(11):1191–1198.
- Medas F, Erdas E, Gordini L, Conzo G, Gambardella C, Canu GL, et al. Risk of malignancy in thyroid nodules classified as TIR-3A: What therapy? Int J Surg. 2017;41 Suppl 1:S60–S64.
- Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19(11):1167–1214.
- Cibas ES, Ali SZ. The 2017 bethesda system for reporting thyroid cytopathology. Thyroid. 2017;27(11):1341–1346.
- Yaprak Bayrak B, Eruyar AT. Malignancy rates for Bethesda III and IV thyroid nodules: a retrospective study of the correlation between fine-needle aspiration cytology and histopathology. BMC Endocr Disord. 2020;20(1):48.
- Cibas ES, Ali SZ. The bethesda system for reporting thyroid cytopathology. Thyroid. 2009;19(11):1159–1165.
- Valderrabano P, McIver B. Evaluation and management of indeterminate thyroid nodules: The Revolution of Risk Stratification Beyond Cytological Diagnosis. Cancer Control. 2017;24(5):1073274817729231.
- Trimboli P, Treglia G, Guidobaldi L, Saggiorato E, Nigri G, Crescenzi A, et al. Clinical characteristics as predictors of malignancy in patients with indeterminate thyroid cytology: a meta-analysis. Endocrine. 2014;46(1):52–59.
- Godoi Cavalheiro B, Kober Nogueira Leite A, Luongo de Matos L, Palermo Miazaki A, Marcel Ientile J, Aurelio VKM, et al. Malignancy rates in thyroid nodules classified as bethesda categories III and IV: Retrospective Data from a Tertiary Center. Int J Endocrinol Metab. 2018;16(1):e12871.
- Wang CC, Friedman L, Kennedy GC, Wang H, Kebebew E, Steward DL, et al. A large multicenter correlation study of thyroid nodule cytopathology and histopathology. Thyroid. 2011;21(3):243–251.
- Bongiovanni M, Spitale A, Faquin WC, Mazzucchelli L, Baloch ZW. The bethesda system for reporting thyroid cytopathology: a meta-analysis. Acta Cytol. 2012;56(4):333–339.
- Rossi ED, Adeniran AJ, Faquin WC. Pitfalls in thyroid cytopathology. Surg Pathol Clin. 2019;12(4):865–881.
- Alexander EK, Kennedy GC, Baloch ZW, Cibas ES, Chudova D, Diggans J, et al. Preoperative diagnosis of benign thyroid nodules with indeterminate cytology. N Engl J Med. 2012;367(8):705–715.
- Tuttle RM, Lemar H, Burch HB. Clinical features associated with an increased risk of thyroid malignancy in patients with follicular neoplasia by fine-needle aspiration. Thyroid. 1998;8(5):377–383.
- Scerrino G, Cocorullo G, Mazzola S, Melfa G, Orlando G, Laise I, et al. Improving diagnostic performance for thyroid nodules classified as bethesda category III or IV: How and by whom ultrasonography should be performed. J Surg Res. 2021;262:203–211.
- Davis NL, Gordon M, Germann E, Robins RE, McGregor GI. Clinical parameters predictive of malignancy of thyroid follicular neoplasms. Am J Surg. 1991;161(5):567–569.
- Baloch ZW, Fleisher S, LiVolsi VA, Gupta PK. Diagnosis of “follicular neoplasm”: a gray zone in thyroid fine-needle aspiration cytology. Diagn Cytopathol. 2002;26(1):41–44.
- Banks ND, Kowalski J, Tsai HL, Somervell H, Tufano R, Dackiw APB, et al. A diagnostic predictor model for indeterminate or suspicious thyroid FNA samples. Thyroid. 2008;18(9):933–941.
- Rago T, Di Coscio G, Basolo F, Scutari M, Elisei R, Berti P, et al. Combined clinical, thyroid ultrasound and cytological features help to predict thyroid malignancy in follicular and Hupsilonrthle cell thyroid lesions: results from a series of 505 consecutive patients. Clin Endocrinol (Oxf). 2007;66(1):13–20.
- Teixeira S, Amaral C, Giestas A, Silva AM, Borges F. Tumor folicular - entidade benigna ou maligna? Casuística de 5 anos. Rev Port End Diab Metabolismo. 2010;1:7–13.
- Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28(3):271–276.
- Iyomasa RM, Tagliarini JV, Rodrigues SA, Tavares ELM, Martins RHG. Laryngeal and vocal alterations after thyroidectomy. Braz J Otorhinolaryngol. 2019;85(1):3–10.
- Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihner E, Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008;393(5):667–673.
Keywords
Bethesda categories; Thyroid nodule; Thyroid neoplasm; Thyroidectomy; Predictive value; Morbidity
Cite this article
Leal C, Santos C, Fernandes U, Guidi G, Martins D, Vieira B, et al. Malignancy rates and predictors of malignancy in Bethesda III and IV classes: a retrospective study. Clin Surg J. 2022;3(2):1–7.
Copyright
© 2022 Clara Leal. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).