Primary Anterior Abdominal Wall Abscess
* Samia Mohan;
Akshat Sudhanshu;
Syed Ahamad;
Kuldeep Singh Mehta;
Kamya Bhasin;
Priyanka Sharma;
-
* Samia Mohan: Department of Surgery, Acharya Shri Chander College of Medical Sciences and Hospital, Sidhra, Jammu, India.
-
Akshat Sudhanshu: Department of Surgery, Acharya Shri Chander College of Medical Sciences and Hospital, Sidhra, Jammu, India.
-
Syed Ahamad: Department of Surgery, Acharya Shri Chander College of Medical Sciences and Hospital, Sidhra, Jammu, India.
-
Kuldeep Singh Mehta: Department of Surgery, Acharya Shri Chander College of Medical Sciences and Hospital, Sidhra, Jammu, India.
-
Kamya Bhasin: Department of Surgery, Acharya Shri Chander College of Medical Sciences and Hospital, Sidhra, Jammu, India.
-
Priyanka Sharma: Department of Surgery, Acharya Shri Chander College of Medical Sciences and Hospital, Sidhra, Jammu, India.
-
Apr 20, 2022 |
-
Volume: 3 |
-
Issue: 1 |
-
Views: 8499 |
-
Downloads: 1761 |
Abstract
Introduction: Abscess can be intra peritoneal, extraperitoneal, retroperitoneal or in the abdominal wall. Abdominal wall abscesses are generally seen in diabetics, immunocomprised or as a sequelae of cutaneous tuberculosis.
Observation: A 50-year-old nondiabetic non hypertensive male presented in the outpatient department with chief complaint of swelling in the left upper abdomen since 3 months. The swelling progressively increased in size and was associated with feeling of heaviness and discomfort. There was no history of fever, malaise, loss of appetite. There was no history of trauma. Serology for HIV infection was negative. Hydatid cyst agglutination tests were also negative. Ultrasonography of the abdominal wall showed a cystic lesion in subcutaneous plane. CT scan abdomen showed cystic lesion in subcutaneous plane with thick material. FNAC showed features of abscess. Incision and drainage was done and pus was sent for culture. No growth was obtained. Patient underwent dressings daily for 1 week with metronidazole locally. Patient recovered uneventfully and remained in follow-up for a month.
Conclusion: Primary abdominal wall abscess is diagnosed once other factors that can lead to abscesses secondarily are ruled out. Treatment is antibiotics and drainage.
Introduction
An abscess is a pocket of pus, usually caused by a bacterial infection. Abscesses can be found anywhere in the body. An abscess can be intraperitoneal, retroperitoneal, extraperitoneal or even I the abdominal wall. They are can be secondary to an underlying pathology or can be primary. Abscesses also may form in or around any abdominal organ, such as the kidneys, spleen, pancreas, or liver, or in the prostate gland. Untreated abscesses can grow and damage nearby blood vessels and organs. Sometimes, bacteria enter the bloodstream (sepsis) and spread to distant organs and tissues. Such spread can be fatal [1]. Primary abscess are rarely seen .The diagnosis and management involves Ultrasonography, CT scan and biopsy. Antibiotics and drainage is usually done.
Case Presentation
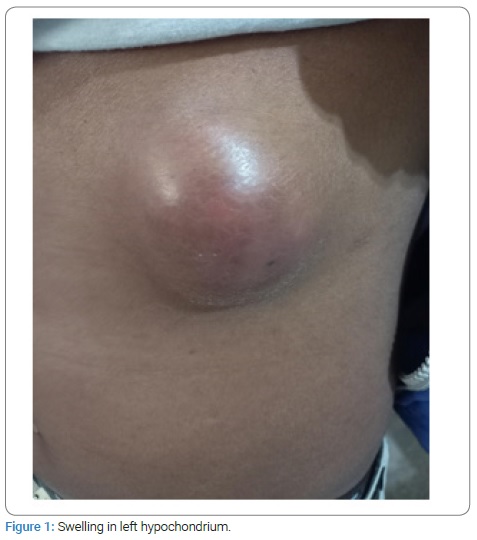
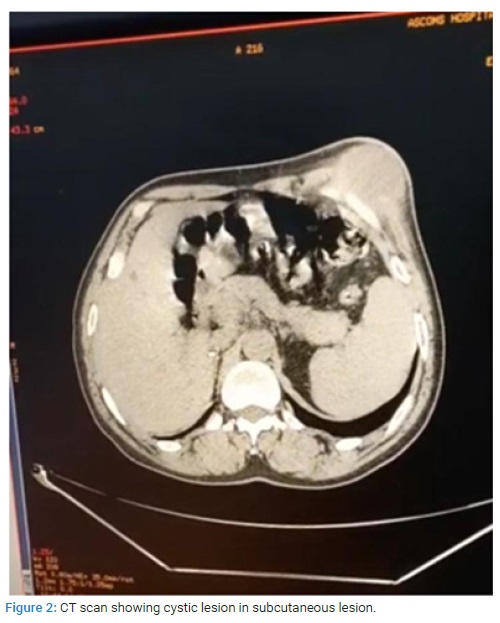
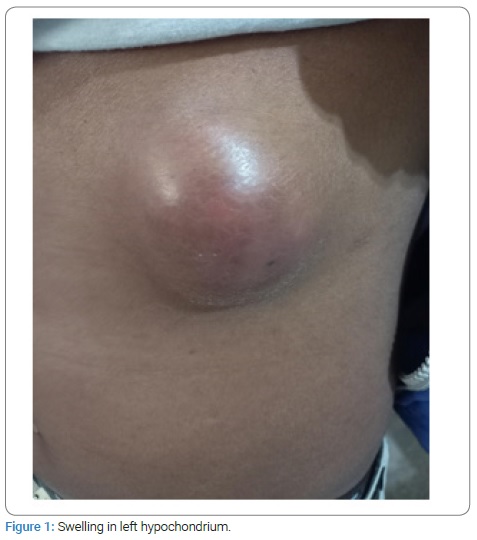
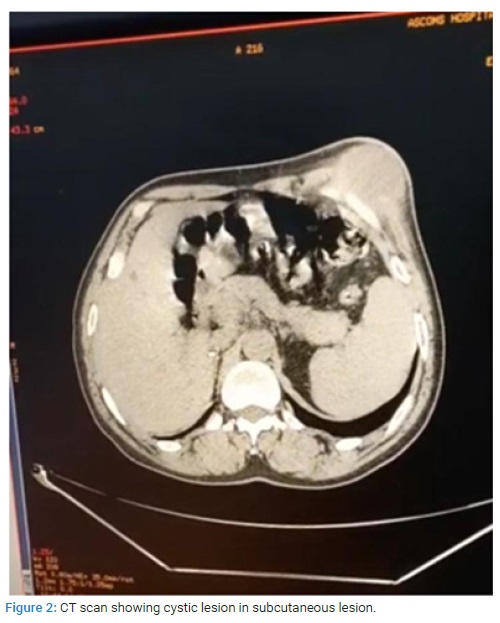
A 50-year-old male patient with no history of any chronic illness presented to the Opd with history of swelling in left hypochondrium since 3 months. The swelling was associated with mild discomfort on walking and was gradually increasing in size. There was no history of tuberculosis, no fever, loss of appetite, trauma (Figure 1) Patient showing lump in left hypochondrium. On local examination, there was a 9 cm × 5 cm swelling in left hypochondrium. There was slight erythema. It was fixed to underlying tissue, but became more prominent when muscles were made taut. The blood investigations: Haemoglobin-12 g%, Tlc-6000 (predominately neutrophils) HIV, HbsAg, HCV- negative. PTI = 86.6 UREA/CREAT = 16/0.9, LFTs-normal, X-Ray chest was normal. Ultrasonography -showed cystic swelling in subcutaneous plane below left costal margin. There was no intra-abdominal pathology. CT scan (Figure 2) showed cyst about 9 cm × 6 cm, separate from ribs, well defined with thick material. Differential diagnosis was hematoma, cold abscess and Lipoma. FNAC showed thick cheesy material, with cytology showing polymorphonuclear cells with features of abscess. Culture showed no growth. ZN Staining was negative. Fungal culture was also negative. Incision and drainage was done and patient was started on amoxicillin and clavulinic acid. Culture was repeated again for atypical organisms and tubercular bacilli. The cultures showed no growth. The patient was started on amoxicillin and clavulinic acid for a week and underwent dressings daily for a week, then on alternate days for 5 days. The wound healed in about 2 weeks and patient recovered completely. He remained in follow-up for 1 month and did not present with any complaints.
Discussion
Primary Anterior Abdominal Wall (AAW) abscess is a rare pathology owing to the limited vascularity of the AAW. Most cases of AAW abscesses described in the literature are secondary to intra-abdominal pathology [2–7]. Only seven cases of primary AAW abscesses have been reported in the literature till date [8–14]. Weiner et al. concluded that ultrasound B mode scanning was an accurate diagnostic test that was particularly useful in demonstrating disease of the AAW because it had no known adverse effects [14]. Understanding of the pathophysiology of AAW abscesses and a high clinical index of suspicion, earlier detection, and apt treatment is possible which ultimately leads to lower morbidity and mortality. Diagnostic imaging like ultrasound, CT, and MRI allow non-invasive examination of the AAW, complementing the clinical evaluation of the patient.
Authors Contribution
Samia Mohan: Admission, evaluation and management including operating on the patient. Concept, collecting the literature, review of the literature, writing the article, critically evaluating the article. Submission of the article. operating surgeon.
Akshat Sudhanshu: Collecting the literature, critically evaluating the article.
Syed Ahamad: Collecting literature.
Kuldeep Singh Mehta: Critically evaluating the article.
Kamya Bhasin: Collecting the literature.
Priyanka Sharma: Collecting the literature.
Consent from the Patient
An informed consent had been obtained from the parents.
Source of Funding
The authors received no financial support for the research, authorship, or publication of this article.
Acknowledgment
Authors would like thank the Head of the department, surgical colleagues, anaesthetists and OT staff of ASCOMS.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Abdominal Abscesses Parswa Ansari, Hofstra Northwell-Lenox Hill Hospital, New York.
- Panchagnula K, Yalla P, Lakshminarayana B, Hegde K, Singaraddi R. Anterior abdominal wall abscess: an unusual presentation of carcinoma of the colon. Arch Surg Clin Res. 2019;3:70–71.
- Kamble PM, Patil A, Jadhav S, Rao SA. Anterior abdominal wall abscess with epididymo-orchitis: an unusual presentation of acute pancreatitis. J Postgrad Med. 2011;57:335–337.
- Eisenstat S. Abdominal wall abscess due to spilled gallstones. Surg Laparosc Endosc. 1993;3:485–486.
- Sakurai Y, Tonomura S, Yoshida I, Masui T, Shoji M, Nakamura Y, et al. Abdominal wall abscess associated with perforated jejunal diverticulitis: report of a case. Surg Today. 2005;35(8):682–686.
- Desai N, Patil S, Thakur BS, Das HS, Manjunath SM, Sawant P, et al. Abdominal wall abscess secondary to subcapsular tubercular liver abscess. Indian J Gastroenterol. 2003;22(5):190–191.
- Neufeld D, Keidar A, Gutman M, Zissin R. Abdominal wall abscesses in patients with Crohn’s disease: clinical outcome. J Gastrointest Surg. 2006;10(3):445–449.
- Hefny AF, Joshi S, Saadeldin YA, Fadlalla H, Abu-Zidan FM. Primary anterior abdominal wall actinomycosis. Singapore Med J. 2006;47(5):419–421.
- Srivastava P, Gupta N, Mishra V, Misra SP, Dwivedi M. Tuberculosis presenting as abdominal wall abscess in an immunocompetent adult. pdf Int J Res Rev. 2020;7:502–505.
- Mitulkumar P, Shailesh P, Purvi D. Cold abscess of the anterior abdominal wall: an unusual primary presentation. Eurorad. 2017;14(3):11–21.
- Malhotra MK. Cold abscess of the anterior abdominal wall: an unusual primary presentation. Niger J Surg. 2012;18(1):22–23.
- Sahu SK, Rawat J, Sindhwani G, Raghuvanshi S, Sachan PK. Primary cold abscess of the anterior abdominal wall: an unusual site of presentation. Internet J Surg. 2008;16:1.
- Nuwal P, Dixit R. Tuberculosis of rectus abdominis muscle. Indian J Chest Dis Allied Sci. 2007;49(3):239–240.
- Weiner CI, Diaconis JN. Primary abdominal wall abscess diagnosed by ultrasound. Arch Surg. 1975;110(3):341–342.
Keywords
Abdominal wall; Abscess; Primary abscess
Cite this article
Mohan S, Sudhanshu A, Ahamad S, Mehta KS, Bhasin K, Sharma P. Primary anterior abdominal wall abscess. Clin Surg J. 2022;3(1):1–3.
Copyright
© 2022 Samia Mohan. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).