First Year Results of Open-Heart Surgery in a New Cardiac Centre
* Muhammad Anwar Azrin;
John Chan Kok Meng;
Yahya Awang;
-
* Muhammad Anwar Azrin: Department of Cardiothoracic Surgery, Cardiac Vascular Sentral Kuala Lumpur (CVSKL) Hospital, Kuala Lumpur, Malaysia.
-
John Chan Kok Meng: Department of Cardiothoracic Surgery, Cardiac Vascular Sentral Kuala Lumpur (CVSKL) Hospital, Kuala Lumpur, Malaysia.
-
Yahya Awang: Department of Cardiothoracic Surgery, Cardiac Vascular Sentral Kuala Lumpur (CVSKL) Hospital, Kuala Lumpur, Malaysia.
-
Dec 30, 2021 |
-
Volume: 2 |
-
Issue: 5 |
-
Views: 3517 |
-
Downloads: 1652 |
Abstract
Background: Cardiac Vascular Sentral Kuala Lumpur (CVSKL) is a newly built private hospital, specialising in cardiac, thoracic and vascular cases. Since its establishment in 2017, we have performed over 100 open-heart surgeries and thus it is important to have an analytical report of all the cases to help us improve our patient safety and quality of care.
Objective: We sought to review the performance of all open-heart surgeries performed at Cardiac Vascular Sentral Kuala Lumpur (CVSKL) since its opening.
Methods: Between November 2017–December 2018, we recorded 124 patients who underwent open-heart surgery at our centre and the data was extracted from the National Cardiovascular and Thoracic Surgical Database (NCTSD). We used univariate analysis and multivariate logistic regression to identify the potential and independent predictors respectively for in-hospital mortality and prolonged postoperative ICU stay (> 2 days).
Results: The in-patient mortality rate was 2.4% (n = 3). All mortalities were high risk patients (EuroSCORE II > 5). There was no mortality reported in low-to-medium risk patients (EuroSCORE II < 5). The most common early postoperative complication was new arrhythmia (28.2%) with atrial fibrillation being the most common type (22.6%). Renal disease was identified as the independent variable for in-hospital mortality (adjusted odds ratio, 34.3; 95% confidence interval, 1.3 to 874.9; p-value of 0.03). In terms of prolonged postoperative ICU stay more than 2 days, hypertension (adjusted odds ratio, 4.9; 95% confidence interval, 1.5 to 15.9; p-value of 0.008) and poor left ventricular function (adjusted odds ratio, 5.0; 95% confidence interval, 1.4to18.5; p-value of 0.015) were found to be the significant independent predictors. Pulmonary complications and duration of postoperative intubation were associated with prolonged postoperative ICU stay more than 2 days with p-values of 0.008 and 0.010 respectively.
Conclusion: Cardiac surgery is a safe procedure in those with low-to-medium risk (EuroSCORE II < 5). Risk stratification of patients is important to better identify patients who are at increased risk following cardiac surgery. The excellent results in the first year at CVSKL demonstrate that open-heart surgery can be safely performed and quality assured in new hospitals with the right team and expertise.
Key Points
What is already known about this subject?
- EuroSCORE II has been widely used as a risk stratification tool to identify patients who are at high risk following open-heart surgery.
- Previous studies have shown renal disease as a significant predictor for mortality following open-heart surgery.
- What does this study add?
- Cardiac surgery is a safe procedure in low-to-medium risk patients (EuroSCORE II < 5).
- Hypertension is found to be associated with prolonged postoperative ICU stay > 2days. Further clinical studies are required to find out about this correlation.
How might this impact on clinical practice?
- Risk stratification is important to identify patients who are at risk following open-heart surgery.
- Multidisciplinary approach is required in managing patients who at high risk especially those with pre-existing renal disease as it is associated with higher mortality rate following open-heart surgery.
Introduction
Open-heart surgery is a complex surgical procedure involving the heart and its surrounding structures. Since its pioneering, open-heart surgery has become a routine procedure that is performed to treat various diseases involving the heart. The development of the cardiopulmonary bypass machine and myocardial protection has made open-heart surgery a safe procedure. Although the surgical techniques and outcomes have advanced in the recent decades, there are still considerable risks for in-hospital mortality and morbidity following open-heart surgery. Therefore, various risk stratification models have been established to help cardiothoracic surgeons predict the outcomes of patients following open-heart surgery. EuroSCORE II is the most widely accepted risk model used to estimate the risk of in-hospital mortality following cardiac surgery [1,2]. Since the introduction of cardiothoracic services in Malaysia in the 1980s, there have been no formal statistical reports on the number of open-heart surgeries performed in the country. This has led to difficulty for the local clinicians and researchers in analysing the performance of cardiothoracic services and the outcomes of open-heart surgeries. Knowing how essential it is to keep track of all the cardiothoracic cases, the Malaysian Association of Thoracic and Cardiovascular Surgery (MATCVS) with the collaboration from the Ministry of Health (MOH) have established the National Cardiovascular and Thoracic Surgical Database (NCTSD) in order to collect and keep records of all cardiothoracic procedures nationwide. Cardiac Vascular Sentral Kuala Lumpur (CVSKL), which is a newly built cardiac hospital in Kuala Lumpur, is one of the centres registered with the NCTSD. Since the beginning of its operation in November 2017, CVSKL has performed more than 120 open-heart surgeries. With this database, we are able to review the clinical outcomes of all the cardiothoracic procedures performed at our centre and improve our patient safety and quality of care.
Objectives
The aim of this study is to:
- Provide comprehensive review of all open-heart surgeries performed at CVSKL.
- Assess the demographic characteristics, preoperative risk factors and comorbidities of all patients who underwent open-heart surgeries at CVSKL.
- Compare the observed mortality with the expected mortality using the EuroSCORE II, and
- Analyse the early postoperative complications following open-heart surgeries.
Materials and Methods
This is a retrospective cross-sectional observational study conducted at Cardiac Vascular Sentral Kuala Lumpur (CVSKL). The data of patients who underwent open-heart surgery from November 2017 until December 2018 were prospectively recorded in the NCTSD. Below is the list of surgeries that were included:
- Coronary artery bypass graft (CABG) surgery
- Valve surgery
- Combined CABG and valve surgery
- Surgery on the thoracic aorta
- Surgery for congenital heart disease
The data were collected from our Hospital Information System (HIS), patient charts, verbal interview with the patients and information gathered from specialists which were then entered into the NCTSD system. The preoperative clinical status and operative interventions were classified using the European System for Cardiac Operative Risk Evaluation (EuroSCORE). The data included were demographic characteristics, angina status using Canadian Cardiovascular Society grading of angina pectoris (CCS), New York Heart Association (NYHA) class, history of Percutaneous Coronary Intervention (PCI), history of previous cardiac surgery, history of myocardial infarction, diabetic status, hypertension, hypercholesterolemia, smoking status, renal disease, pulmonary disease, neurological disease, preoperative heart rhythm, ejection fraction, left main stem disease and critical preoperative state. The expected mortality rate was calculated using the EuroSCORE II. The patients were risk stratified to either low-to-medium risk (EuroSCORE II less than 5) or high risk (EuroSCORE II of 5 and above). The critical preoperative state was defined as aborted sudden cardiac arrest, preoperative use of Intra-Aortic Balloon Pump (IABP), acute renal failure or preoperative inotropes. The operative data that were included were operative urgency status (urgent defined as surgery during the same admission as angiography), redo-procedures, types of cardiac procedure, number of procedures, cardioplegia solution, cumulative CPB time, cross clamp time and use of Intra-Aortic Balloon Pump (IABP). Early postoperative complications during hospital and intensive care stay were also collected. The data included were length of ICU stay from the day of surgery, length of postoperative intubation, readmission to ICU within 24 hours of discharge, reintubation within 24 hours of extubation, in-hospital mortality, unplanned reoperation, pulmonary complications (defined as prolonged ventilation > 48 hours, pneumonia or tracheostomy), new arrhythmias, new renal failure (requiring dialysis), graft harvest site infection or sternal wound infection (requiring surgical intervention).
Statistical Analysis
Statistical analysis was carried out using the IBM SPSS Version 23.0. The prevalence of categorical variables was presented in frequency tables while the continuous variables were presented in terms of mean and standard deviation. All continuous variables were tested for degree of skewness. Variables which did not follow normal distribution such as length of postoperative ICU stay and duration of postoperative intubation were expressed with median value and interquartile range. A cut-off value was decided to delineate between normal and prolonged duration for statistical analysis. Predictors for in-hospital mortality and prolonged postoperative ICU stay > 2 days were analysed using the univariate analysis. All variables that were significant in the previous analysis were included in the multivariate logistic regression to identify the significant independent variables. Postoperative complications and prolonged postoperative ICU stay were analysed using either Chi-square test or Fisher’s exact test whichever is suitable. Significance was defined as a p-value less than 0.05.
Results
Demographic Distribution
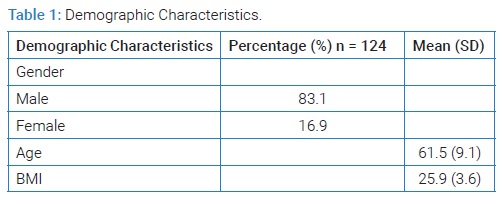
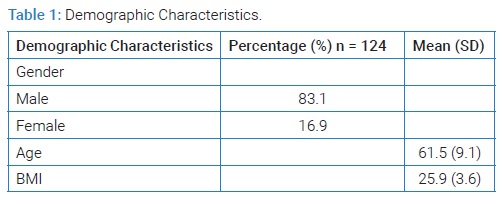
There were 124 open-heart surgeries performed at CVSKL from November 2017 until December 2018. Majority of the patients aged between 60 years–69 years old with a mean age of 61.5 (SD9.1). 83.1% of the patients were male and 16.9% of them were female. 87.1% of the cases were elective (Table 1).
Cardiac History
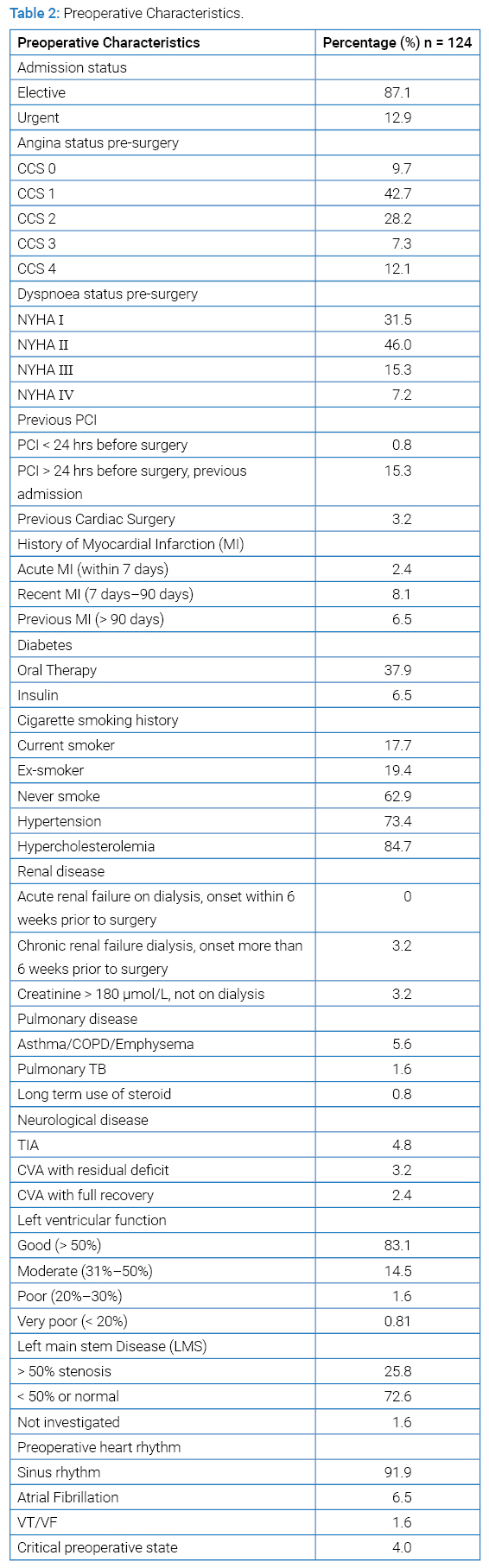
Preoperatively, 42.7% of the patients were in the Canadian Cardiovascular Society grading of angina pectoris (CCS)class 1 and 46.0% were in the New York Heart Association (NYHA) Class II. 16.1% of the patients had a previous PCI, 3.2% had previous history of cardiac surgery in which 2 of them were CABG, 1 was valve surgery and 1 was thoracic endovascular aortic repair. 17.0% of the patients had a prior history of Myocardial Infarction (MI) (Table 2).
Risk Factors & Co-morbidities
In terms of risk factors for coronary artery disease, 6.5% of our patients were insulin-dependent diabetic and 17.7% of them were active smokers. Majority of our patients had hypertension (73.4%) and 84.7% had hypercholesterolemia. We identified three main comorbidities which were renal disease, pulmonary disease and neurological disease. 3.2% of the patients had chronic renal failure on dialysis and creatinine more than 180 µmol/L not on dialysis respectively, 5.6% of the patients had obstructive pulmonary disease, 1.6% had pulmonary tuberculosis and 0.8% was on long-term steroid use for pulmonary disease. With regards to neurological disease, 4.8% of them had Transient Ischaemic Attack (TIA), 3.2% had Cerebrovascular Accident (CVA) with residual deficit and 2.4% had CVA with full recovery (Table 2).
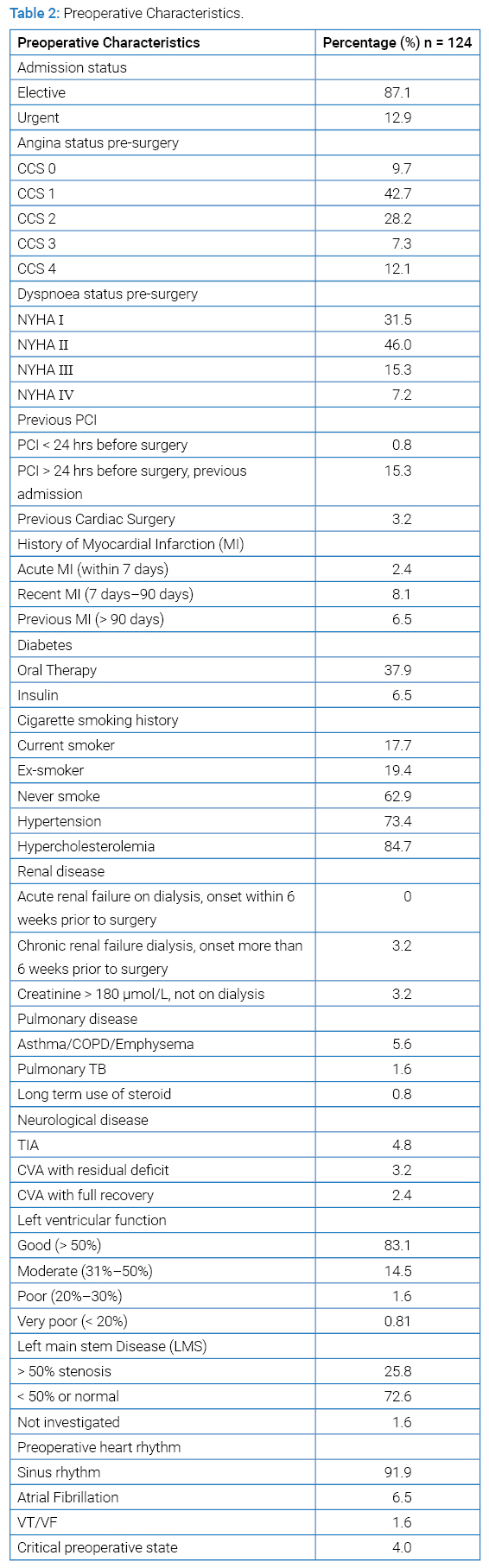
Preoperative Cardiac Status and Cardiac Investigations
In terms of cardiac function, 83.1% of our patients had normal ejection fraction (> 50%), 14.5% had moderate EF of 31%–50%, 1.6% with poor EF (20%–30%) and 0.8% had very poor EF (< 20%). 25.8% had left main stem disease or stenosis more than 50%. With regards to preoperative heart rhythm, majority of our patients had normal sinus rhythm (91.9%), 6.5% had atrial fibrillation and 1.6% had either any episode of ventricular fibrillation or ventricular tachycardia. 4.0% of our patients were in the critical preoperative state (Table 2).
Operative Procedures
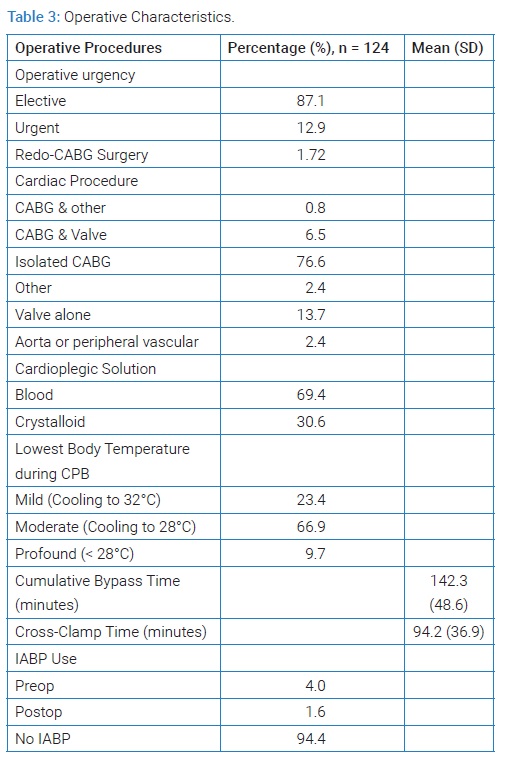
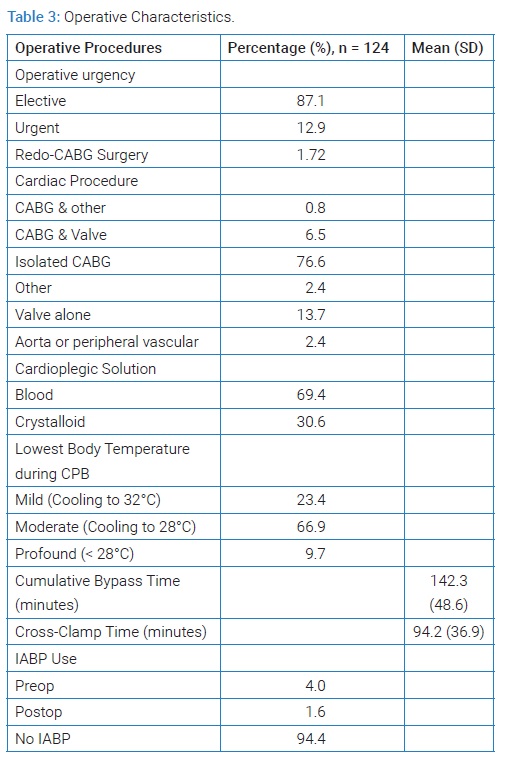
12.9% of the cases required urgent operation. 1.7% was redo-CABG surgeries. Isolated CABG accounted about 76.6% of the total cases, followed by valve alone (13.7%) and combined CABG & valve (6.5%). 0.8% was a case of CABG with ventricular septal defect (VSD) closure and 2.4% were surgeries on the thoracic aorta. Blood cardioplegia solution was used in 69.4% of the patients. The mean cumulative CPB time was 142.3 minutes (SD 48.6) and the mean cross clamp time was 94.2 minutes (SD 36.9). 4.0% of the patients required preoperative IABP use and 1.6% required postoperative IABP use. The indications were prophylactic measure, unstable angina or haemodynamic instability (Table 3).
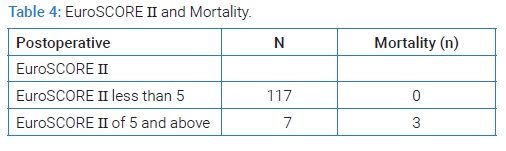
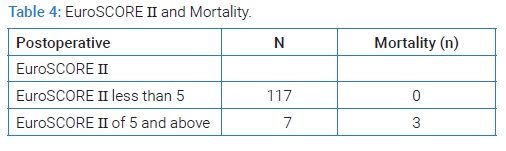
Risk of Mortality using EuroSCORE II & In-hospital Mortality
The overall in-patient mortality rate was 2.4% (n = 3). All mortalities were high risk patients (EuroSCORE II ≥ 5). There was no mortality reported in low-to-medium risk patients (EuroSCORE II < 5) (Table 4).
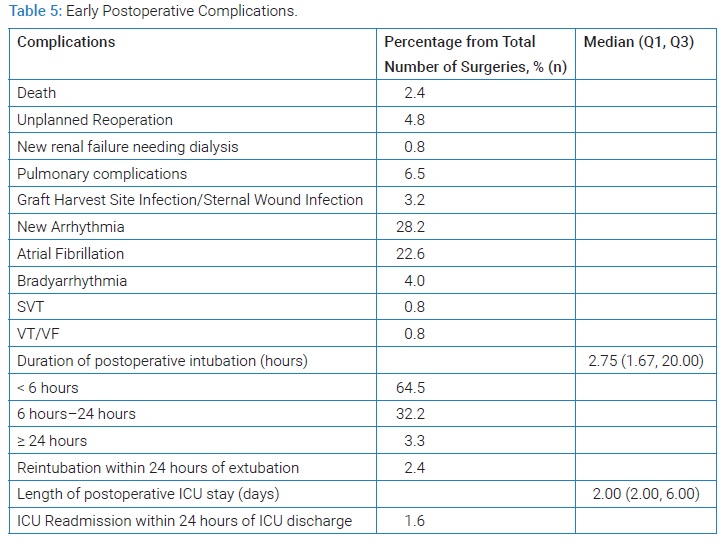
Postoperative Care & Complications
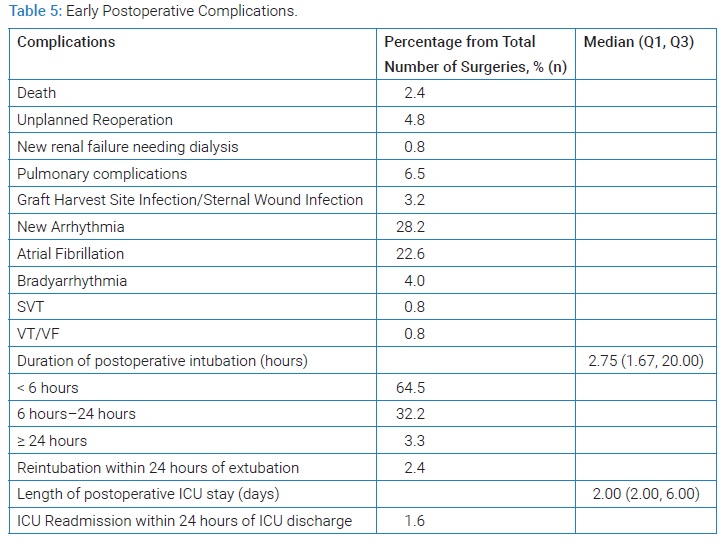
There were 3 mortalities reported within one year period and all of them were due to cardiogenic shock secondary to ventricular failure. The median length of postoperative ICU stay was 2.0 days. ICU readmission within 24 hours of discharge was less than 1.6%.The median duration of postoperative intubation was 2.75 hours. 2.4% of the cases required reintubation within 24 hours of extubation. 64.5% of the patients were extubated within 6 hours, 32.2% between 6 hours–24 hours and 3.3% had a prolonged postoperative intubation > 24 hours. 35.5% were prolonged intubation > 6 hours. 4.8% of the cases underwent reoperation due to bleeding, 0.8% developed renal failure needing dialysis, 6.5% had pulmonary complications and 3.2% were complicated with either graft harvest site or sternal wound infection. Arrhythmias were reported to be 28.2% of the total cases, with atrial fibrillation being the most common type at 22.6% (Table 5).
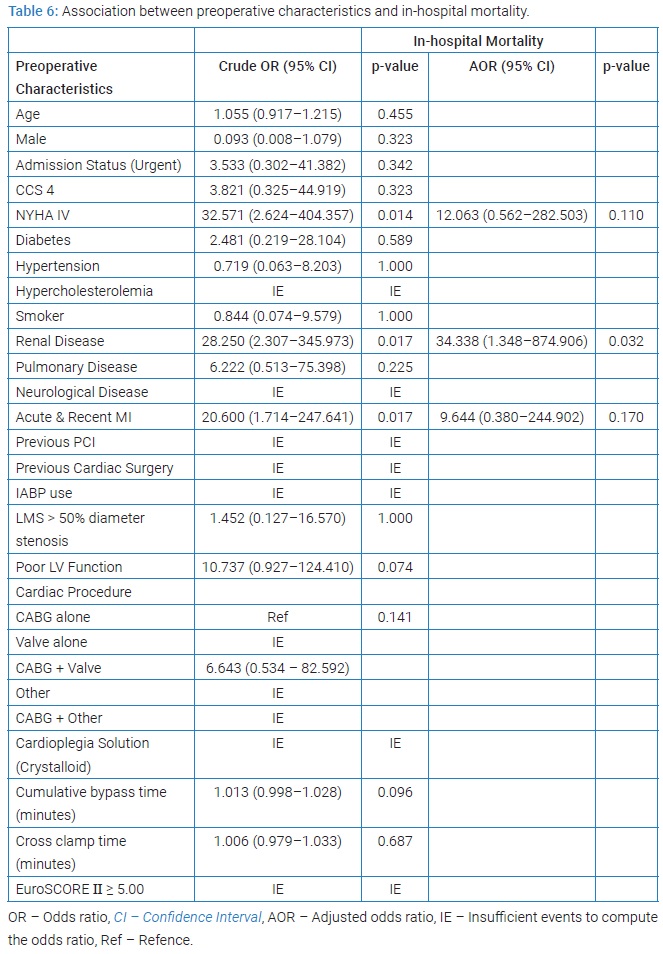
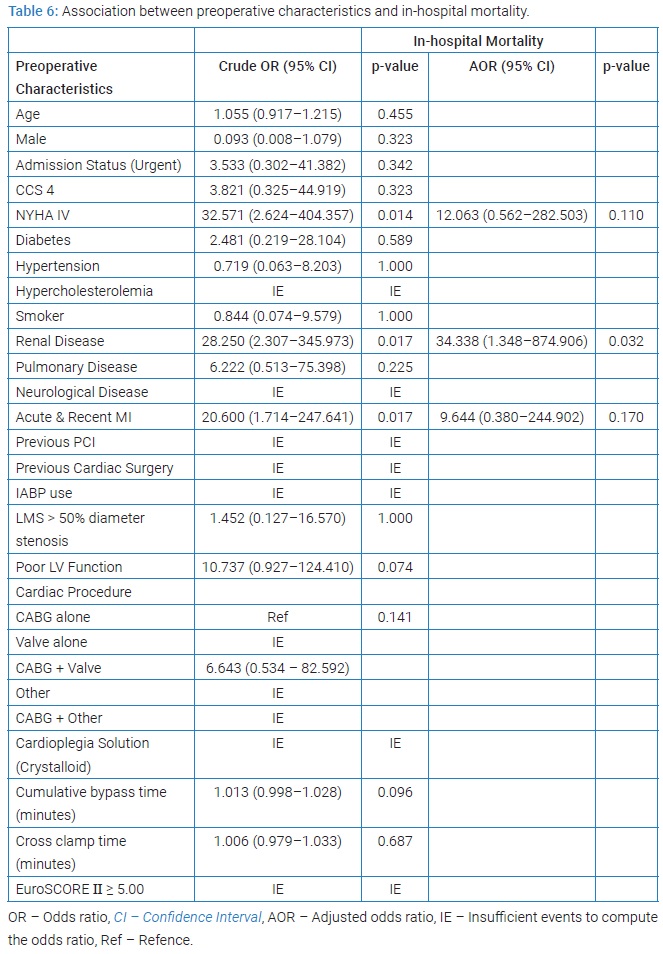
Predictors for in-hospital mortality
In the univariate analysis, NYHA IV, renal disease and acute and recent myocardial infarction were found to be potential predictors for early postoperative mortality. However, only renal disease was identified to be the independent predictor for in-hospital mortality (AOR, 34.3; 95% CI, 1.2 to 794.7; p-value of 0.04) in the multivariate logistic regression (Table 6).
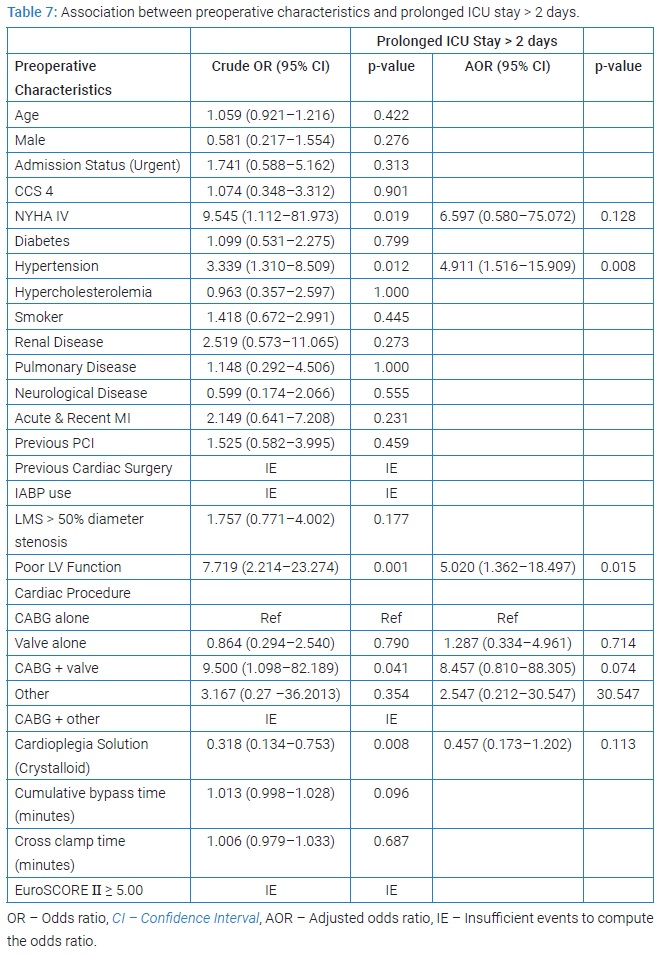
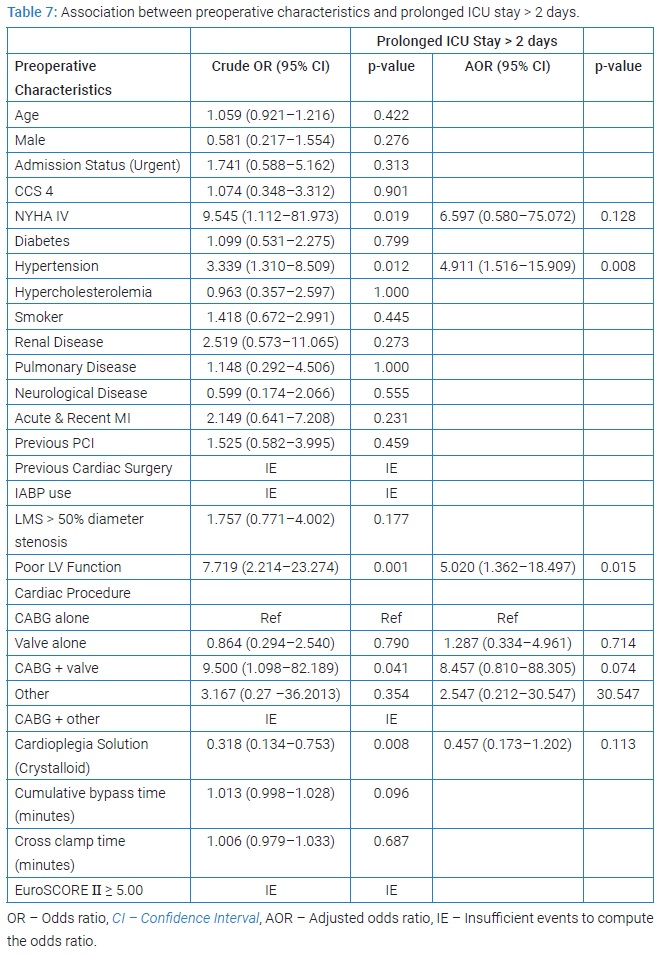
Predictors for prolonged postoperative ICU stay
The potential predictors for prolonged ICU stay were NYHA IV, hypertension, poor LV function, longer CPB time and cross clamp time. Meanwhile, crystalloid cardioplegia solution was found to have less effect on the length of postoperative ICU stay compared to blood cardioplegia in the univariate analysis. However, using the multivariate logistic regression, the independent predictors were only hypertension (AOR, 4.9; 95% CI, 1.5 to 15.9; p-value of 0.008) and poor LV function (AOR, 5.0; 95% CI, 1.4 to 18.5; p-value of 0.015) (Table 7).
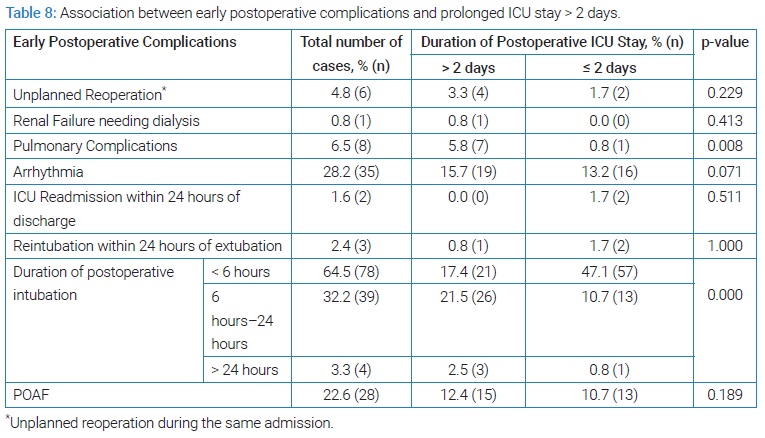
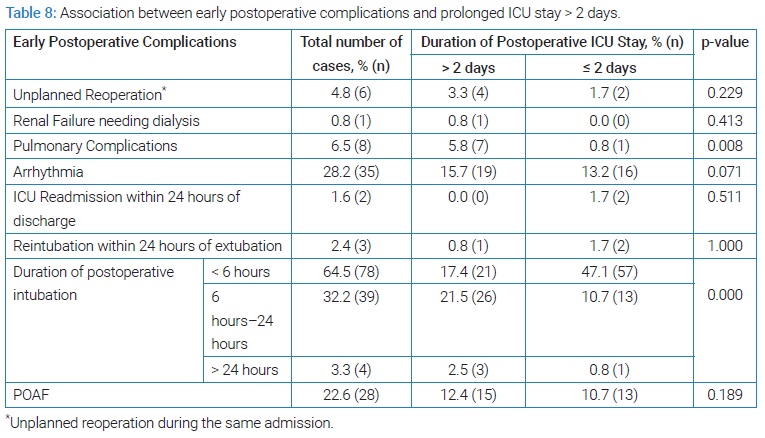
Association between early postoperative complications and prolonged postoperative ICU stay
Pulmonary complications and duration of postoperative intubation were associated with prolonged postoperative ICU stay > 2 days with p-values of 0.008 and 0.000 respectively. Majority of patients who stayed in ICU > 2 days were those who had duration of postoperative intubation between 6 hours–24 hours and more than 24 hours (Table 8).
Discussion
Early postoperative complications
Atrial Fibrillation (AF) is one of the common complications following open-heart surgery. The incidence of AF varies in previous studies, ranging from 10% to 65% [3,4]. In a prospective study by Mariscalco et al. [5] among patients who underwent isolated CABG, the incidence of postoperative AF in their population was 31%. Multiple risk factors such as increasing age, previous episodes of AF, valvular disease and previous cardiac surgery were associated with postoperative atrial fibrillation following cardiac surgery [6–8]. Pulmonary complications are the second most common early postoperative complication after cardiac surgery in our study (6.5%). These complications included pneumonia and prolonged ventilation > 2 days. In a study by Ailawadi et al. [9] the incidence of pneumonia after cardiac surgery was 2.4%. The risk factors for pneumonia in their study were COPD, smoking and older patients. FAA Al-Qubati et al. [10] demonstrated that the incidence of pulmonary complications after open-heart surgery was 15.08% with left phrenic nerve palsy being the most common type (3.35%) followed by Adult Respiratory Distress Syndrome (ARDS) (2.87%). However, the definition of pulmonary complications varies across studies and hence the inconsistency of incidence reported between all studies.
Renal disease and in-hospital mortality
In our study, renal disease was found to be an independent predictor for in-hospital mortality. Multiple previous studies have shown the association between preoperative renal dysfunction and mortality after cardiac surgery. In a study by Thakar et al. [11] among those patients who died, the median preoperative GFR was 57.0 mL/min/1.73m2 while those who survived, the median preoperative GFR was 72.0 mL/min/1.73m2 (p-value < 0.001). A Society of Thoracic Surgeons (STS) national cardiac database study by Cooper WA et al. [12] demonstrated that the risk of mortality in patients with moderate renal disease (GFR 30-59 mL/min/1.73m2) was 55% higher compared to those with normal renal function whereas the risk was 3.8 times higher among those on dialysis. Apart from that, chronic kidney disease itself is a known risk factor for developing Coronary Artery Disease (CAD) and the outcomes of CAD in these patients are poorer compared to those with normal renal function [13]. Some of the possible mechanisms include endothelial dysfunction, metabolic syndrome, haemodynamic instability and arteriosclerosis.
Hypertension and prolonged ICU stay
There were not many previous studies that showed the association between hypertension and prolonged ICU stay. This finding will need further exploration in future studies.
Poor LV function and prolonged ICU stay
In our study, we found that patients with poor left ventricular function had prolonged postoperative ICU stay. Similar findings were seen in a study by Shah R et al. [14] which showed that that patients who stayed more than 4 days in ICU postoperatively had lower ejection fraction compared to those who stayed less than 4 days (ICU < 4 days, 49.42 ± 11.80 vs. ICU > 4 days, 46.09 ± 13.14 p-value, 0.001) although their cut-off duration of prolonged stay was longer. Atoui R et al. [15] in their study also found that patients with ejection fraction < 40 % had a 1.83 times higher risk of prolonged ICU stay > 2 days (RR, 1.83; 95% CI 1.03 to 3.25, p-value of 0.04) following cardiac surgery. A systematic review of 29 papers by Almashrafi et al. [16] recognised low ejection fraction as one of the independent variables for prolonged ICU stay. However, Eltheni R et al. [17] did not find any significant association between poor left ventricular dysfunction and prolonged ICU stay after cardiac surgery. Another retrospective study by Mirinazhad et al. [18] showed that there was no significant difference between the duration of postoperative ICU stay and preoperative left ventricular function [18]. The discrepancy of outcomes between previous studies and our study could be due to the different cut-off values used to distinguish between normal and prolonged postoperative ICU stay. Most patients with poor LV function would probably need longer duration in ICU because they take longer time to wean off from inotropic support and recover from anaesthesia.
Pulmonary complications and prolonged ICU stay
The incidence of pulmonary complications in our study (6.9%) is similar to that reported by Naveed A et al. [19] (6.2%). However, apart from pneumonia, prolonged ventilation > 48 hours and pneumonia, their study also included atelectasis and adult respiratory syndrome as pulmonary complications which our study did not. Hence, the percentage of pulmonary complications in our population might be underrepresented. Unfortunately, there were not many studies that showed any significant association between pulmonary complications and prolonged ICU stay.
Conclusion
Cardiac surgery is a safe procedure in those with low-to-medium risk (EuroSCORE II < 5). Risk stratification of patients is important to better identify patients who are at increased risk following cardiac surgery. The excellent results in the first year at CVSKL demonstrate that open-heart surgery can be safely performed and quality assured in new hospitals with the right team and expertise. Renal disease remains an important independent predictor for in-hospital mortality following open-heart surgery.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Ad N, Holmes SD, Patel J, Pritchard G, Shuman DJ, Halpin L. Comparison of EuroSCORE II, Original EuroSCORE, and The Society of Thoracic Surgeons Risk Score in Cardiac Surgery Patients. Ann Thorac Surg. 2016;102(2):573–579.
- Nilsson J, Algotsson L, Höglund P, Lührs C, Brandt J. Early mortality in coronary bypass surgery: the EuroSCORE versus The Society of Thoracic Surgeons risk algorithm. Ann Thorac Surg. 2004;77(4):1235–1239.
- Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med. 2001;135(12):1061–1073.
- Villareal RP, Hariharan R, Liu BC, Kar B, Lee VV, Elayda M, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol. 2004;43(5):742–748.
- Mariscalco G, Klersy C, Zanobini M, Banach M, Ferrarese S, Borsani P, et al. Atrial fibrillation after isolated coronary surgery affects late survival. Circulation. 2008;118(16):1612–1618.
- Asher CR, Miller DP, Grimm RA, Cosgrove 3rd DM, Chung MK. Analysis of risk factors for development of atrial fibrillation early after cardiac valvular surgery. Am J Cardiol. 1998;82(7):892–895.
- Zaman AG, Archbold RA, Helft G, Paul EA, Curzen NP, Mills PG. Atrial fibrillation after coronary artery bypass surgery: a model for preoperative risk stratification. Circulation. 2000;101(12):1403–1408.
- Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720–1729.
- Ailawadi G, Chang HL, O’Gara PT, O’Sullivan K, Woo YJ, DeRose JJ Jr, et al. Pneumonia after cardiac surgery: Experience of the National Institutes of Health/Canadian Institutes of Health Research Cardiothoracic Surgical Trials Network. J Thorac Cardiovasc Surg. 2017;153(6):1384–1391.e3.
- Al-Qubati FAA, Damag A, Noman T. Incidence and outcome of pulmonary complications after open cardiac surgery, Thowra Hospital, Cardiac center, Sana’a, Yemen. Egyptian J Chest Dis Tuberculos. 2013;62(4):775–780.
- Thakar CV, Worley S, Arrigain S, Yared JP, Paganini EP. Influence of renal dysfunction on mortality after cardiac surgery: modifying effect of preoperative renal function. Kidney Int. 2005;67(3):1112–1119.
- Cooper WA, O’Brien SM, Thourani VH, Guyton RA, Bridges CR, Szczech LA, et al. Impact of renal dysfunction on outcomes of coronary artery bypass surgery: results from the Society of Thoracic Surgeons National Adult Cardiac Database. Circulation. 2006;113(8):1063–1070.
- Cai Q, Mukku VK, Ahmad M. Coronary artery disease in patients with chronic kidney disease: a clinical update. Curr Cardiol Rev. 2013;9(4):331–339.
- Shah R, Patel R, Sharma R, Pandya H, Shah K. Factors Influencing Prolonged Stay in the Intensive Care Unit After Cardiac Surgery. Nat J Med Res. 2015;5(2):140–144.
- Atoui R, Ma F, Langlois Y, Morin JF. Risk factors for prolonged stay in the intensive care unit and on the ward after cardiac surgery. J Card Surg. 2008;23(2):99–106.
- Almashrafi A, Elmontsri M, Aylin P. Systematic review of factors influencing length of stay in ICU after adult cardiac surgery. BMC Health Serv Res. 2016;16:318.
- Eltheni R, Giakoumidakis K, Brokalaki H, Galanis P, Nenekidis I, Fildissis G. Predictors of prolonged stay in the intensive care unit following cardiac surgery. ISRN Nurs. 2012;2012:691561.
- Mirinazhad M, Parsa D, Faridaalaee G, Bilehjani E, Irajian M, Shadvar K, et al. Prevalence and risk factors for prolonged ICU stay after adult Cardiac Surgery. Ann Anesthesiology Crit Care. 2016;1(1):e8635.
- Naveed A, Azam H, Murtaza HG, Ahmad RA, Baig MAR. Incidence and risk factors of Pulmonary Complications after Cardiopulmonary bypass. Pak J Med Sci. 2017;33(4):993–996.
Keywords
Open-heart surgery; CABG; Valve surgery; EuroSCORE II; In-hospital mortality
Cite this article
Azrin MA, Kok Meng JC, Awang Y. First year results of open-heart surgery in a new cardiac centre. Clin Surg J. 2021;2(5):1–8.
Copyright
© 2021 Muhammad Anwar Azrin. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).