Is The Zygoma Implant A Long-Term Successful Method for Reconstruction of The Atrophic Maxilla? – A Prospective Cohort Study
Maths Ericson Bellinetto;
* Lars Rasmusson;
Peter Nilsson;
-
Maths Ericson Bellinetto: Department of Oral and Maxillofacial Surgery, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden.
-
* Lars Rasmusson: Department of Oral and Maxillofacial Surgery, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; Maxillofacial Unit, Linköping University Hospital, Linköping, Sweden.
-
Peter Nilsson: Department of Oral and Maxillofacial Surgery, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; Department of Oral and Maxillofacial Surgery, Ryhov Hospital, Jönköping, Sweden.
-
Feb 18, 2022 |
-
Volume: 3 |
-
Issue: 1 |
-
Views: 2092 |
-
Downloads: 1643 |
Abstract
Background: The Zygoma implant is an alternative to bone grafting to rehabilitate the severely resorbed posterior maxilla. Long-term clinical studies are few, and the primary purpose of this prospective clinical study was to assess the survival rate of zygoma implants used for retention of fixed dental bridges, up to 17 years.
Material and methods: Forty-one consecutive patients with resorbed edentulous maxillae were included in the study. In total, 88 Zygoma implants and 160 conventional implants were installed, and all patients received fixed superstructures.
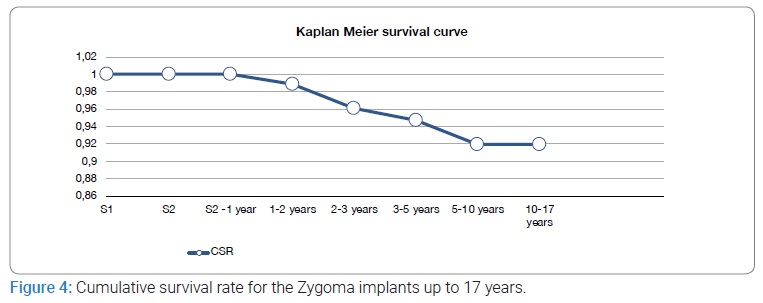
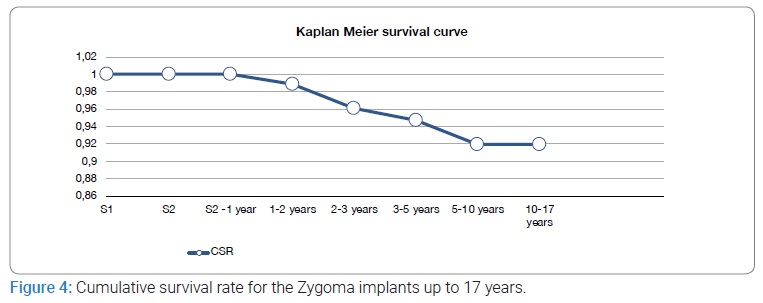
Results: The cumulative survival rate for the Zygoma implants was 92%. Implant losses and subsequent removal were caused by sinus infections. At the 10 years follow-up, 35 patients remained in the study. All except one patient had Implant-Supported Fixed Prostheses (ISFP).
Conclusion: Zygoma implants are reliable and represent a high survival rate in a long-term perspective in the treatment of severely resorbed maxillae. In combination with conventional anterior implants, the zygoma implants give good support for ISFP with few complications. The main drawback with zygoma implants is the risk of the development of chronic sinusitis and osteolysis, where the implant penetrates the alveolar crest into the sinus.
Introduction
The edentulous maxilla frequently exhibits a significant challenge during rehabilitation because of the limited alveolar bone, especially in the posterior due to its close relation to the maxillary sinus. Autogenous and alloplastic bone grafts are often used [1–3]. A common finding is a higher number of lost fixtures and marginal bone loss than fixtures placed in non-transplanted bone [4]. Additionally, autogenous bone grafts resorb over time, and it has been suggested that only approximately 50% of the volume remains after six months, and resorption may continue further [5,6].
According to Brånemark et al. The Zygoma implants allowed high loading forces of the superstructure and could support a 14 unit bridge. The treatment with Zygoma implants was considered less invasive and with a shorter treatment time than bone grafting and conventional implants [7]. However, long-term follow-up prospective studies of severely atrophic maxillae treated with Zygoma implants are sparse. Most reports published on Zygoma implants and prosthetic rehabilitation were in the beginning case reports. Only a few publications were cohort studies [8–12].
The overall aim of this prospective study was to longitudinally follow-up a cohort of edentulous patients with resorbed maxillary crest and bilaterally installed Zygoma implants. The main objective was Zygoma implant survival rate. Secondary objectives were to register any biological or technical complications related to the Zygoma implants and their penetration zones: zygomatic bone, sinus cavity, and crestal bone.
Materials and Methods
Consecutive patients referred to the Maxillofacial Unit, Jönköping, Sweden, for rehabilitation of resorbed edentulous maxillae during 2000–2005 were included in the study. Zygoma implants were chosen instead of augmentation of the sinus floor in cases with posterior resorption. Patients were voluntarily recruited to the study, and all were given the option to go through bone grafting to the sinus floor as an alternative treatment. The sample size was estimated to be 40 to 50 patients during the inclusion period. All surgeries were performed by one surgical team.
Inclusion Criteria: Edentulous atrophic maxillae made treatment with standard osseointegrated implants impossible, and patients with previously failed implants in the posterior maxilla with poor prognosis for retreatment with conventional fixtures only. Included were also cases with resorption of the anterior maxilla where bone augmentation was necessary before installing regular implants.
Exclusion Criteria: Patients who were not medically fit for general anesthesia.
Sinusitis: Patients with evidence of chronic or acute sinusitis were excluded based on CT scans and clinical signs or symptoms. All patients were clinically examined and assessed radiographically with panoramic x-ray and CT scans before surgery.
Clinical Procedures: Forty-one patients were clinically examined and treated during the period 2000–2005. Complementary bone grafting was judged necessary in four patients before installing conventional supporting fixtures in the anterior maxilla. Bone grafting in these patients was performed simultaneously with the placement of the Zygoma implants. The grafts were taken from the iliac crest and allowed to heal for 4 months to 6 months. Complimentary installation of conventional implants was then performed and allowed to osseointegrate.
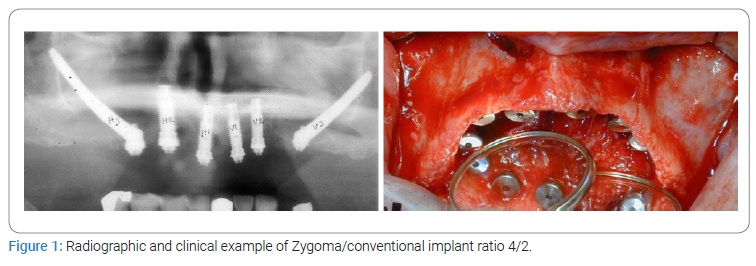
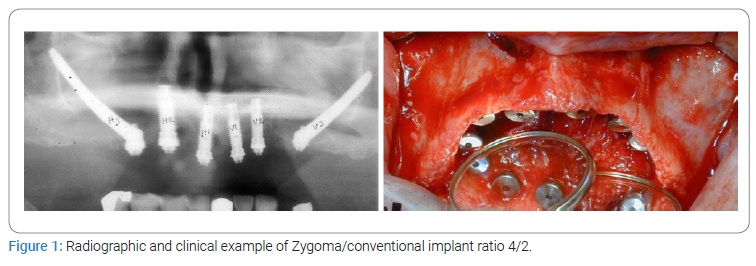
Fixture Installation: The surgical installation of the Zygoma implants was performed according to the guidelines given by Brånemark et al. [7]. During the first stage of surgery, fixtures were installed under general anesthesia and local infiltration anesthesia. The Zygoma and conventional anterior implants were placed in the same session except for the four grafted cases. A crestal incision with releasing incision in the midline and posteriorly in the second molar area was performed. The exposure included the palatal side and was extended in the posterior-superior direction to the lateral surface of the zygomatic bone, between the zygomatic arch and the lateral and medial surface of the frontal process of the zygomatic bone. Special care was taken to release the soft tissue at the posterior and lateral part of the zygomatic buttress. The conventional implants placed anteriorly were inserted according to standard clinical procedures for the Brånemark and ASTRA Tech systems, respectively. Cover screws were placed, and the wound was closed. The postoperative care followed the normal routines (Figure 1).
The patients were instructed not to wear their dentures 2 weeks to 4 weeks after the first stage surgery. After initial mucosal healing, the dentures were optimized and relined with a soft tissue conditioner (Viscogel®, Lifco AB, Stockholm, Sweden) to relieve the supporting tissues and the fixtures. The dentures were regularly controlled and relined during the six-month healing period to avoid hostile forces on the submerged institutions. Second stage surgery was performed under local infiltration anaesthesia and healing abutments were connected to the fixtures.
Evaluation Procedures: Examination and complication protocols were used. Clinical follow-up, including radiographs, were performed after one month (baseline), 1 year, 2 years, 5 years, 10 years, 12 years, and up to 17 years. Intraoral standardized analog radiographs were generally taken with a long-cone paralleling technique, but in some cases, panorama and PA projections had to be used because of anatomic reasons, e.g., flat palatal vaults. A radiographic technical shift was introduced at the five-year control into the digital technique.
Survival: Primary objective was Zygoma implant survival rate, i.e., the fixture was present or not at the follow-up examination irrespective of its condition.
Complications: Biological and technical events such as infections, bone resorption, and complications related to the superstructure were recorded.
Statistical Analysis: Estimation of Cumulative Survival Rate (CSR) for both Zygoma and conventional implants were made using the non-parametric Kaplan-Meier estimator.
Ethical Approval: The regional ethical committee approved this prospective cohort study in Linköping, Sweden.
Dnr: M134-07.
Results
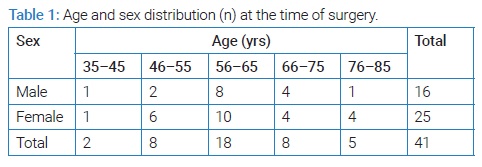
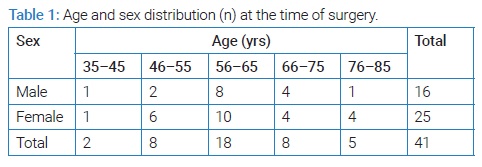
In total, 41 consecutive patients with edentulous resorbed maxillae were included in the study (Table 1).
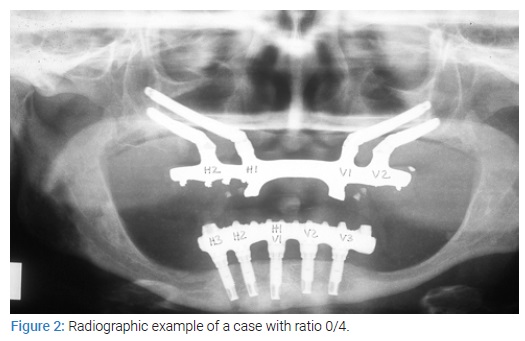
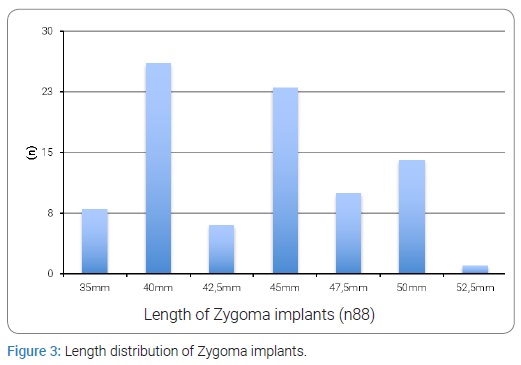
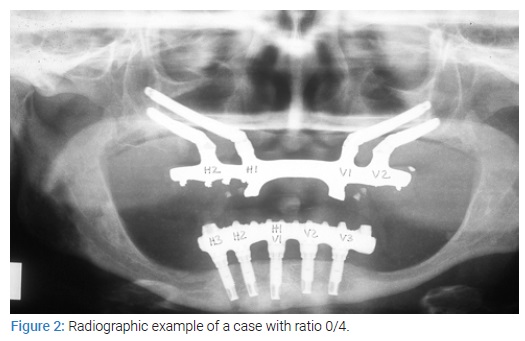
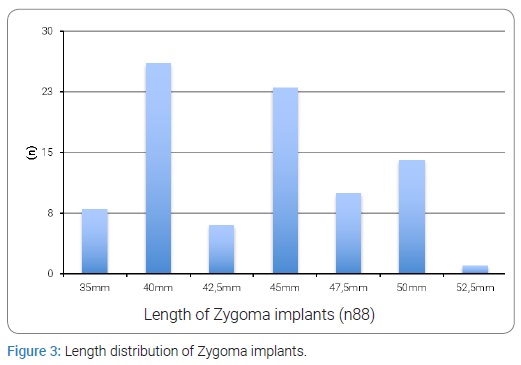
Follow-up was upto 17 years. 88 zygoma- and 160 conventional anterior implants were installed in 41 patients. Out of these, four patients had eight remaining fixtures from previously failed implant therapy. The opposite jaw was dentated in 25 patients, and 13 patients had complete ISFP. Two patients had combinations of their own teeth and partial ISFPs, and one patient had an overdenture. Forty-one ISFPs were fabricated with 40 cases made of gold/acrylic and one case of titanium/porcelain. All of the 88 Zygoma implants had a machined surface (Nobel Biocare AB, Gothenberg Sweden), the length distribution shown in (Figure 2).
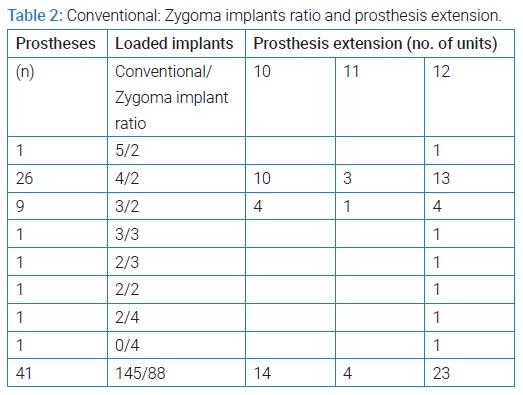
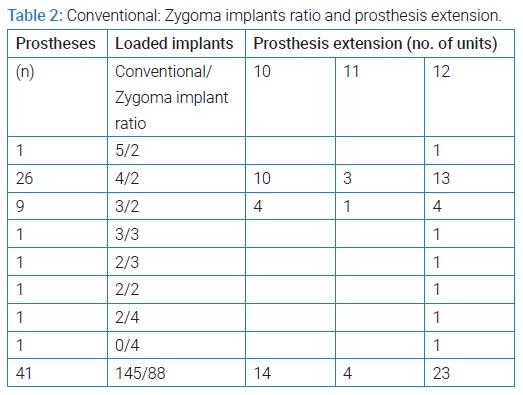
The frontal conventional implants were either Brånemark (Nobel Biocare, Gothenburg Sweden) or Astra Tech implants, (Astra Tech AB, Mölndal Sweden). The distribution and ratio between loaded Zygoma- and conventional implants and the prosthesis extensions shown in (Table 2).
Before loading, 15 (9%) conventional frontal fixtures were lost in 11 patients, including one bone-grafted patient who lost two fixtures. None of the Zygoma implants were lost before loading. During the first year, one patient left the study for personal reasons. No Zygoma implant was lost during the first year. At the Second year follow-up, 39 patients remained in the study. Out of these, 26 patients agreed to unscrew the ISFP, and the fixtures were separately evaluated. All were considered stable and successfully osseointegrated. One patient dropped out for an unrelated reason. One patient with the ratio of 0/4 fixtures lost one anterior Zygoma implant during that period due to severe loss of bone in the alveolar crest. After 4 years, the same patient lost the other anterior Zygoma implant. After a healing period, the patient was treated with a bone graft and conventional implants in the frontal region. At the five and ten-year follow-up, respectively, 35 patients remained in the study. The cause for dropping out was personal reasons or general health problems (Figure 3).
One Zygoma implant, successfully osseointegrated, was excluded at the five-year follow-up because of chronic sinusitis. It was cut inside the sinus due to oral communication around the fixture’s head. Three conventional implants were also lost in the same patient. At the seven-year follow-up, one patient had lost four conventional implants, and the two remaining Zygoma implants were removed due to chronic infection. After these 7 years of ISFP, the patient wanted to go back to the removable prosthesis. In total, 6 Zygoma implants were lost during the follow-up period, giving a cumulative survival rate of 92% up to 17 years.
Sinusitis: In five out of Forty one patients, episodes of sinusitis occurred. The first case with sinusitis was found after 3 years. After that, eleven more episodes of acute sinus infection were recorded during the follow-up period, one of them with severe and repeated episodes of sinusitis. However, this patient kept the original construction and all of her implants (Figure 4).
In total, four of the lost implants were in three of the patients with a sinusitis infection. In the two remaining sinusitis patients, the conditions resolved after treatment.
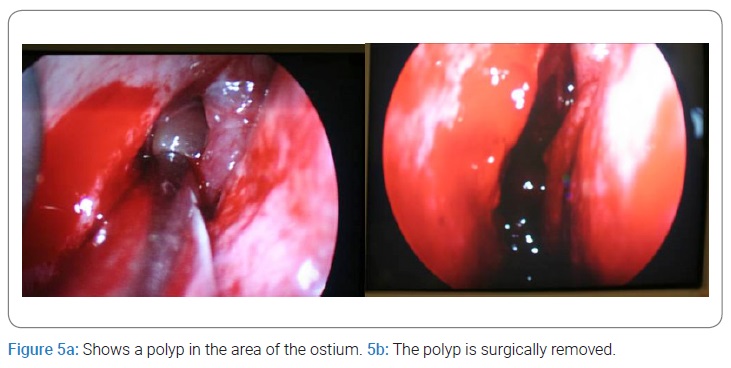
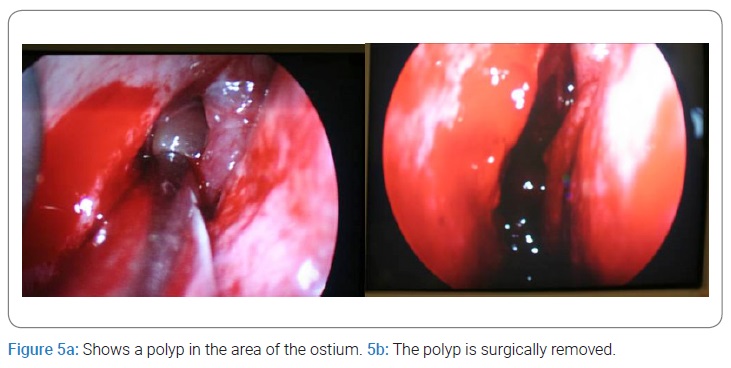
One patient with sinusitis had a polyp in the nasal-sinus connection that needed removal (Figure 5a, Figure 5b).
Radiology: The intraoral radiographs of the Zygoma implants were impossible to interpret regarding bone loss. Radiolucencies were seen at the abutment interface close to the penetrating abutment screw and where the fixture entered into the oral cavity through the alveolar crest/palatal bone. At baseline, 30 (34%) zygoma abutments showed radiolucencies close to the penetrating abutment screw, 35 (40%) showed no signs of bone resorption. In total, 23 (26%) of the Zygoma implants could not be radiographically evaluated. After one year, the corresponding radiolucency figures were 36 (42%), 29 (34%), and 21 (24%), respectively. Prosthetic complications were registered for fractured or worn acrylic teeth in 2 patients during the first year and five patients at the Second year follow-up. One porcelain fracture in the only titanium/porcelain prosthesis also appeared during the first year. One framework was fractured twice during the second year and welded, and another framework showed misfit, was sectioned and welded. Two patients initially got temporary fixed prostheses exchanged for permanent after less than one year.
Discussion
This long-term follow-up study shows that rehabilitation with zygoma implants entails stable and reliable support for cross-arch fixed prosthesis cases with severely resorbed maxillae. The zygoma implant is a solid and predictable anchorage for fixation in the posterior part of the maxilla. The treatment is considered less invasive and exhibits less postoperative morbidity than traditional bone grafting techniques [11]. In our experience, it is a challenge to install more than one zygoma implant on each side of the maxilla. Even technically and surgically possible, it might be too much implant material about the remaining alveolar crest and the zygomatic bone. The close relationship between the implants can also cause soft tissue reactions. It might also be more elasticity in the whole construction with only zygoma implants than in combination with conventional fixtures. However, a fixed bridge supported by four zygoma implants is sometimes the only solution after maxillary resection with subsequent reconstruction (Figure 6a).

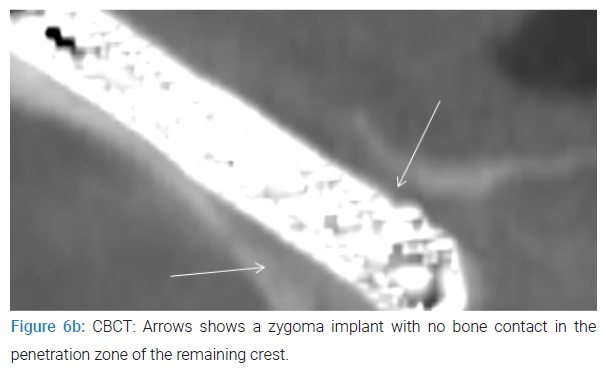
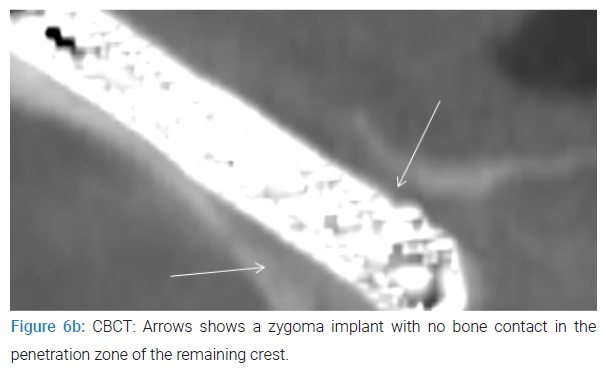
One patient with the ratio of 0/4 implants, who lost one of the anterior zygoma implants during the first year of follow-up, showed severe loss of bone in the alveolar crest, which might be a result of inflammation due to soft tissue movements, forces, and creaking. After 2 years, the same patient lost the other anterior zygoma implant due to loss of osseointegration. After a healing period, this patient was treated with bone grafts and conventional fixtures in the frontal region and with a stable long-term result (Figure 6b).
The number of lost Zygomatic implants was relatively few in the present study. Our results follow a review by Goiato et al. 2014 [13]. Including 25 follow-up studies. The mean survival rate for zygomatic implants was 97.86%, with a follow-up of 36 months. The present study’s survival rate was 96.0 % at the same follow-up period. Rodriguez-Chessa et al. [14]. Showed a survival rate of 79. 1% after a mean of 20 months. In a study by Malevez, 2004 [15]. The survival rate was higher. However, the follow-up varied from 6 to 41 months. Circumstances around the penetration zone into the alveolar crest were the main reason for implant removal. Therefore, it is important to solve the problem with leakage around the fixture at the alveolar crest level. Recently, new implant design and surgical protocol have shown promising results, and the number of sinus infections may be lowered in the future [16]. In this study, five patients presented with sinusitis. It is reasonable to believe that the sinus cavity’s penetration per se causes the infection, but rather the earlier mentioned bacterial leakage in the marginal bone/fixture area. Our results also showed that the infected sinuses are challenging to treat, leading to the removal of the implant fixture.
Conclusions
Zygoma implants represent a high survival in treating the severely resorbed maxillae. In combination with conventional anterior implants, zygoma implants give good posterior support for Implant-Supported Fixed Prostheses (ISFP). with few complications in long-term follow-up. The main drawback with zygoma implants is the risk of developing osteolysis, where the implant penetrates the alveolar crest into the sinus and subsequently causes a chronic infection.
Acknowledgment
Funding of the study was received from FORSS (The Research Council for South-East Sweden). The authors would like to thank Dr Tom Bergendal for valuable scientific advise and excellent prosthetic rehabilitation of the patients in the present study.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Hallman M, Hedin M, Sennerby L, Lundgren S. A prospective 1-year clinical and radiographic study of implants placed after maxillary sinus floor augmentation with bovine hydroxyapatite and autogenous bone. J Oral Maxillofacial Surg. 2002;60(3):277–284.
- Del Fabbro M, Testori T, Francetti L, Weinstein R. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004;24(6):565–577.
- Thor A, Wannfors K, Sennerby L, Rasmusson L. Reconstruction of the severely resorbed maxilla with autogenous bone, platelet-rich plasma, and implants: 1-year results of a controlled prospective 5-year study. Clin Implant Dent Relat Res. 2005;7(4):2009–2020.
- Becktor JP, Isaksson S, Sennerby L. Endosseous implants and bone augmentation in the partially dentate maxilla: an analysis of 17 patients with a follow-up of 29 to 101 months. Int J Oral Maxillofac Implants. 2007; 22(4):603–608.
- Johansson B, Grepe A, Wannfors K, Hirsch JM. A clinical study of changes in the volume of bone grafts in the atrophic maxilla. Dentomaxillofac Radiol. 2001;30(3):157–161.
- Dasmah A, Thor A, Ekestubbe A, Sennerby L, Rasmusson L. Particulate vs. block bone grafts: three-dimensional changes in graft volume after reconstruction of the atrophic maxilla, a 2-year radiographic follow-up. J Craniomaxillofac Surg. 2012;40(8):654–659.
- Brånemark PI, Gröndahl K, Ohrnell LO, Nilsson P, Petruson B, Svensson B, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70–85.
- Hirsch JM, Ohrnell LO, Henry PJ, Andreasson L, Brånemark PI, Chiapasco M, et al. A clinical evaluation of the Zygoma fixture: one year of follow-up at 16 clinics. J Oral Maxillofac Surg. 2004;62(9 Suppl 2):22–29.
- Becktor JP, Isaksson S, Abrahamsson P, Sennerby L. Evaluation of 31 zygomatic implants and 74 regular dental implants used in 16 patients for prosthetic reconstruction of the atrophic maxilla with cross-arch fixed bridges. Clin Implant Dent Relat Res. 2005;7(3):159–165.
- Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implants. 2010;25(6):1213–1221.
- Aparicio C, Manresa C, Francisco K, Ouazzani W, Claros P, Potau JM, et al. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014;16(3):447–459.
- Davo R, Bankauskas S, Laurincikas R, Kocyigit ID, Sanchez de Val JEM. Clinical performance of zygomatic implants- retrospective multicenter study. J Clin Med. 2020;9(2):480.
- Goiato MC, Pellizzer EP, Moreno A, Gennari-Filho H, dos Santos DM, Jr Santiago JF, et al. Implants in the zygomatic bone for maxillary prosthetic rehabilitation: a systematic review. Int J Oral Maxillofac Surg. 2014;43(6):748–757.
- Rodriguez-Chessa J G, Olate S, Duque Netto H, Shibli J, de Moraes M, Mazzonetto R, et al. Treatment of atrophic maxilla with zygomatic implants in 29 consecutives patients. Int J Clin Exp Med. 2014;7(2):426–430.
- Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: a 6-48 months follow-up study. Clin Oral Implants Res. 2004;15(1):18–22.
- Aleksandrowicz P, Kusa-Podkanska M, Tomkiewicz W, Kotula L, Perek J, Wysokinska-Miszczuk J, et al. Platform switch hybrid zygoma implants improve prosthetics and marginal bone protection after extra-sinus placement. Clin Implant Dent Relat Res. 2020;22(2):186–192.
Keywords
Zygoma implants; Survival rate; Sinusitis
Cite this article
Bellinetto M, Rasmusson L, Nilsson P. Is the zygoma implant a long-term successful method for reconstruction of the atrophic maxilla? – A prospective cohort study. Clin Surg J. 2022;3(1):1–6.
Copyright
© 2022 Lars Rasmusson. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).