Abstract
National Institute of Clinical Excellence recommends continuous monitoring of core body temperature using an insertable temperature probe is part of monitoring in major operations (NICE DG6). There have been many reported complications from using insertable temperature probes when this is not properly used and vigilantly monitored. This includes bleeding from posterior nostrils, entrapment in hiatus hernia surgery and aspiration of sheath in re usable types (Thomas Wass 2010). We report a case where the temperature probe migrated intraoperatively into the stomach and was inadvertently stapled across while performing laparoscopic sleeve gastrectomy.
Background
National Institute of Clinical Excellence recommends continuous monitoring of core body temperature using an insertable temperature probe is part of monitoring in major operations [NICE DG6] [1]. There have been many reported complications from using insertable temperature probes when this is not properly used and vigilantly monitored. This includes bleeding from posterior nostrils, entrapment in hiatus hernia surgery and aspiration of sheath in re usable types (Thomas Wass 2010) [2]. We report a case where the temperature probe migrated intraoperatively into the stomach and was inadvertently stapled across while performing laparoscopic sleeve gastrectomy.
Case Presentation
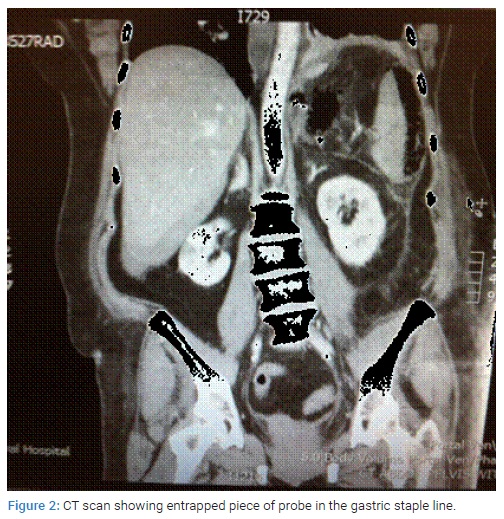
A 54-year morbidly obese lady was worked up for bariatric surgery and an elective Laparoscopic Sleeve Gastrectomy was performed. She had a BMI of 42 and was a diabetic. The procedure was uneventful without any immediate complications. A 9 french disposable general purpose temperature manufactured by GE Healthcare (Figure 1) probe was used to continuously monitor body temperature during the procedure. After the completion of surgical procedure the temperature probe was removed and it was noted that the probe had distal 2 cm missing. This missing end the probe was later retrieved from the resected gastric specimen in the pathology department. She had an uneventful recovery and was discharged home on the day three following the operation. She presented 7 days after the operation with clinical features of post-operative collection. CT scan showed staple line dehiscence with evidence of free fluid through out the abdomen (Figure 2).
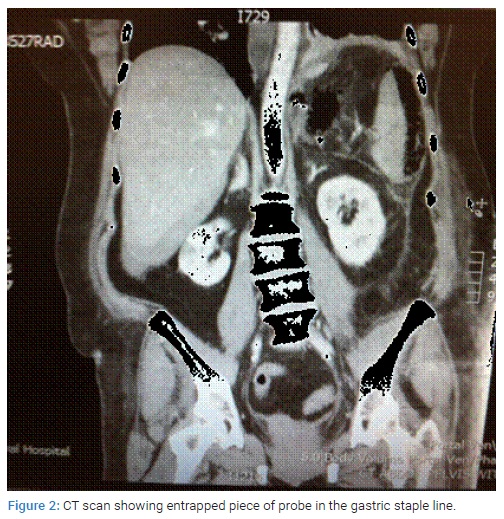
She underwent an emergency laparoscopy which needed intra-operative conversion to a midline laparotomy. Intra operatively, an upper GI endoscopy was performed. This confirmed a piece of the probe was still stuck to the gastric wall along the staple line leading to staple line breakdown (Figure 3).

The probe piece was removed endoscopically and a methylene blue leak test was performed (Figure 4). The visualised staple line leak corresponded to the probe entrapment site on methylene blue testing and this was primarily repaired with PDS sutures. After a thorough washout a single large bore drain was placed near to the leak site at the gastro-esophegeal junctional site. The patient was very unwell in the immediate post operative period with bilateral basal atelectasis and Acute Respiratory Distress Syndrome (ARDS), necessitating ventilatory and ionotropic support. As expected her drain, soon showed gastric content effluent. At present, she is being weaned of her tracheostomy with a double lumen nasojejunal tube for feeding and decompression of gastric juices with an aim of facilitating closure of her perforation.

Literature Review
Wass et al. [2] reported a case of the probe entrapment during a revision of Nissen’sfundo-plication. The situation was identified at the end of surgical procedure as it was unable to pull out the probe. The patient was still anesthetised and the surgical team performed a re-operation to undo the stitches and remove the probe. The probe had evidence of needle entry point suggesting it had been sutured during the fundo-plication. They recommended educating the anaesthetic team regarding the potential complications, using alternative modes such as bladder probe if there is an indwelling catheter. They also recommended better communication between the surgical and anaesthetic team during the critical periods of the procedure. A case of massive epistastix was reported by Sinha et al. [3] after probe insertion following cardiac surgery. The patient had systemic heparin given during the procedure that involved cardio-pulmonary bypass and was reversed using protamine after the procedure. The patient had bleeding post procedure in to the stomach. The source of bleeding was identified using direct laryngoscope to be coming from right posterior nasal orifice. He was managed by nasal packing and continued ventilation. The probe was defective with a cut and the bleeding was attributed to this defect in the probe. Another case of aspiration of the sheath while using sheathed re-usable temperature probe was reported by Kumar [4] during hemicolectomy. The situation was identified at the end of procedure whenthe re usable probe came out without the sheath. The sheath was later extracted using sinus scope by ENT surgeon. The concluded that although the re usable probes are safe to use but the team has to be vigilant about this potential complication. We have also heard, although not published a case of fatal nasopharyngeal bleeding due to a similar temp probe in our tertiary hospital. They have subsequently issued hospital guidelines not to use them through the nose. They are now being used though mouth and rectally for oral surgeries. A case was reported from Israel Yanowski et al. [5] where a temperature probe was stapled across during a sleeve gastrectomy. The anaesthetist noticed and informed of possible migration of the probe during the procedure. With failed attempt to withdraw the probe a further exploration was done and both bits of the probe removed before the completion of the procedure.
Discussion
These temperature probes currently used in our theatre are longer then before. They do not have any markings or any fixation devise. This makes it difficult to know if the probe inadvertently slips down. It is advisable to always fix it at a safe length so that it does not get in to surgically field. We have to look at alternate ways to insert the probe in to mouth or rectum if deemed unsafe through the mouth. Alternate ways of measurement using bladder probes should be looked in to if surgery involves oesophago-gastric junction and below. It is possible that the temp probe was placed correctly to start with but slipped or moved when the bougie was inserted or manipulated during surgery. To start with we have initially sent a departmental alert and national alert through bariatric teams. The departmental protocol now involves fixing the probe at the required length when used. The aim or reporting this avoidable complication is to create awareness of appropriate action that needs to be taken when sleeve gastrectomies is performed. Moreover a clear insight into the possibility of stapling needs to be appreciated by anaesthetists to prevent similar mistakes.
Summary
I summary we are report a case of temperature probe entrapment in staple line during a sleeve gastrectomy leading to post-operative dehiscence requiring emergency laparotomy for removal of the entrapped piece.
Learning Points
The temperature probes can lead to fatal complications if not used properly and vigilantly. The surgical and anaesthetic teams must be constantly aware that this could be a potential source for entrapment in upper gastro-intestinal procedures.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Laparoscopic sleeve gastrectomy; Temperature probe
Cite this article
Guru Raghavendra GK, Balupuri S. Temperature probe entrapment during laparoscopic sleeve gastrectomy: a preventable complication. Clin Surg J. 2021;2(4):1–4.
Copyright
© 2021 Gargeshwari Krishnamurthy Guru Raghavendra. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).