Abstract
A 50-year-old woman was admitted to our Hospital for progressive dyspnoea and reduced exercise tolerance. She had primary diagnosis, in childhood, of TGS, VSD and PS for which she underwent surgical anatomical correction that include LV outflow reconstruction by intracardiac prosthetic baffle and RVOT reconstruction with an extra cardiac conduit according to Rastelli procedure. Echocardiography demonstrated left and right ventricular outflow tract obstruction. We performed optimal therapeutic strategy by multidisciplinary team discussion, novel minimal surgical approach via percutaneous cannulation aimed at minimizing the reentry injury risks, implanted through percutaneous techniques, with fluoroscopy and TEE guidance in a hybrid setting.
Introduction
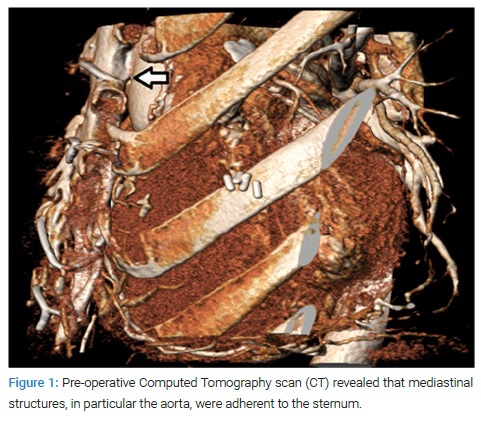
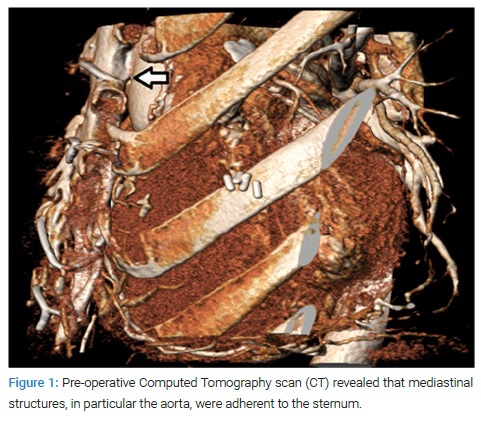
The anatomical correction for TGA, VSD and PS was firstly described by Dr. Giancarlo Rastelli in 1969 [1]. Long-term outcome of this procedure (that include LV outflow reconstruction by intracardiac prosthetic baffle, and RVOT reconstruction with an extracardiac conduit) is influenced by the need of late reoperations due to Left Ventricular Outflow Tract (LVOT) and RVOT obstruction [2,3]. However, in Grown-Up Congenital Heart Disease (GUCH) patients, late surgery is a high-risk procedure and, technically, repeated sternotomy may be associated with adverse injuries to mediastinal structures. Many studies have demonstrated how a preoperative planning including proper cardiovascular imaging may be helpful in identifying patients at risk of re-entry due to strong adherences between mediastinal structures and sternum in redo-surgery [4,5].
Case Presentation
A 50-year-old woman, with primary diagnosis of Transposition of the Great Arteries (TGA), Ventricular Septal Defect (VSD) and Pulmonary Stenosis (PS) was referred to our Grown Up Congenital Heart (GUCH) center for progressive dyspnoea and reduced exercise tolerance. She had a Blalock-Taussig shunt palliation at the age of 3, a Rastelli procedure 2 years afterwards, at 13 years of age the Right Ventricle to Pulmonary Artery (RV-PA) conduit was surgically replaced, and she was re-operated again at the age of 30 for conduit replacement and enlargement of the Rastelli tunnel. At the time of our evaluation, the patient was in good general health, complaining of shortness of breath for minimal effort according to the New York Heart Association classification (NYHA class III/IV). At physical examination, the patient presented raised jugular venous pressure, an audible grade 3/6 ejection systolic murmur at the left third intercostal space and lower leg edema. The Electrocardiogram (ECG) showed atrial flutter (74 bpm) with evidence of right bundle branch block, right atrial overload (23 cm2) and Right Ventricular (RV) hypertrophy (9.6 mm) with preserved right ventricular ejection fraction (TAPSE 18 mm, S’ 8 cm/s, RVFAC 35%) with strain. Echocardiography revealed moderate-to-severe right ventricular to pulmonary artery (RV-PA) conduit obstruction (130 mmHg) and an accelerated left Ventricle-Aorta (LV-Ao) tunnel obstruction (maximum gradient 52 mmHg, mean gradient 32 mmHg), normal ejection fraction (60%), estimated RV pressure of 122 mmHg. Inferior vena cava, as well as hepatic veins were dilated with reduced inspiratory collapse. The cardiac Magnetic Resonance Imaging (MRI) confirmed the echocardiographic findings, further presenting a flattened and reduced caliber RV-PA conduct, strongly thickened walls and VSD patch’ with irregular thickening. A Computed Tomography scan (CT) revealed that mediastinal structures, in particular the aorta, were adherent to the sternum (Figure1).
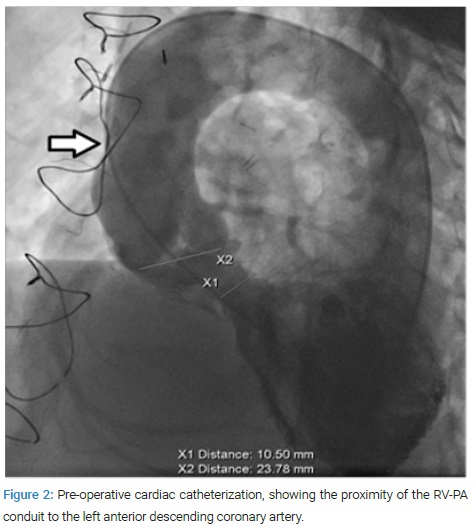
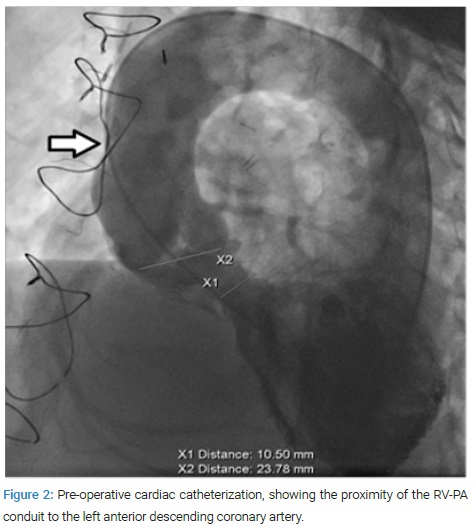
Furthermore, a performed cardiac catheterization supported the previously established findings, showing the proximity of the RV-PA conduit to the left anterior descending coronary artery, that was considered an exclusion criterion for trans-catheter therapy (Figure 2). After careful evaluation of the clinical case, our multidisciplinary staff “Heart Team” decided for high-risk surgical treatment of the residual lesions.
Surgery Description
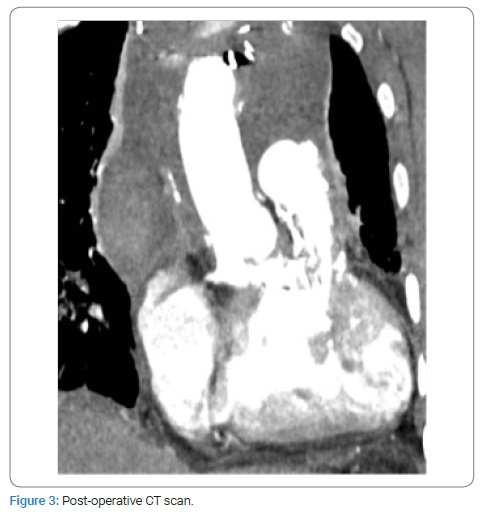
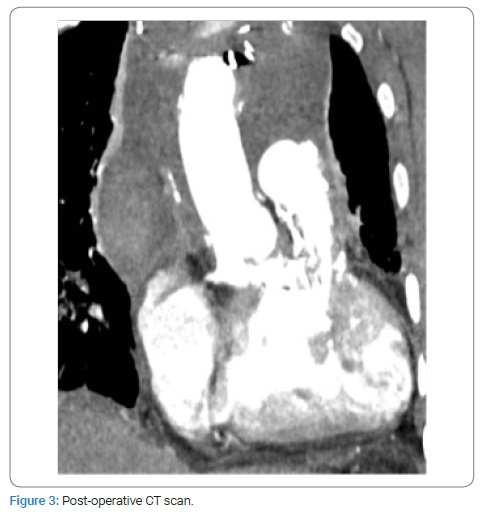
Endo Vent and Propledge (Edwards Lifesciences Corp., Irvine, USA) were placed under fluoroscopic and transesophageal echocardiography guidance. Cardiopulmonary by-pass was established before redo-sternotomy by right femoral vein and axillary artery cannulation. After cardioplegic arrest the RV-PA conduit was opened and a bioprosthesis (Trifecta 23, St. Jude Medical; St. Paul, Minnesota, USA) was implanted in the pulmonary position with continuous monofilament suture. The VSD patch was probed from the right ventricle and it was opened longitudinally and resected, leaving a 1- to 2-mm rim of patch near the conduction system. An appropriately shaped patch was inserted and sewn with continuous monofilament suture to enlarge the Rastelli tunnel. Inferiorly, the rim of the old patch was used to avoid injury to the conduction system. At intraoperative view, the aorta is mildly dilated, with frail wall, the moderate aortic valve regurgitation is confirmed, so ascending aorta replacement with a vascular graft and aortic valve commissuroplasty were performed. Subsequently, the aortic cross-clamp was removed and a RV-PA patch was used to complete the Right Ventricular Outflow Tract (RVOT) reconstruction with the heart beating during rewarming. The post-operative course was regular, except for the need of surgical re-exploration for bleeding on the first post-operative day. A post-operative CT scan documented a good result of surgery (Figure 3). Six months after surgery the patient is doing well with normal functional capacity. From an echocardiographic point of view, a normal biventricular systolic function, normal function of the pulmonary prosthesis and a mean LV-Ao gradient of 18 mmHg are appreciated.
Consent
The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Adult congenital heart patients; Rastelli procedure; Reentry injury risk; Multidimensional perspective; Case report
Cite this article
Grandinetti M, Przybylek B, Calabrese M, Lillo R, Perri G, Graziani F, et al. Multidimensional perspective and hybrid setting for surgical strategy in a complex adult congenital heart disease patient. Clin Surg J. 2021;2(4):1–3.
Copyright
© 2021 Maria Grandinetti. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).