Introduction
Thoracic Outlet Syndrome (TOS) remains a challenging and widely misunderstood disorder that affects the upper extremity [1–3]. TOS is associated with several controversies. These include the definition of the disease, the actual pathophysiology of the disease, the appropriate diagnostic tests, and the appropriate therapeutic interventions. Presently, the only consistent aspects of TOS are the confusion among medical practitioners and the poor results with all therapeutic interventions. The philosopher George Satayana has been credited with saying: ”Those who cannot remember the past are condemned to repeat it” [4]. This observation is especially true when trying to understand the controversies that are associated with TOS. For two millennia, physicians and scientists have made observations about the neurovascular conditions that affect the upper extremity. These observations have been related to a variety of conditions and pathophysiologic processes. Regrettably, with very little attention to this rich history, in the 1950’s an attempt was made to consolidate all conditions that affect the upper extremity under the umbrella of TOS.
In 1956, Peet, a physiotherapist at Mayo Clinic, published the paper Thoracic outlet syndrome: evaluation of a therapeutic exercise program. He used the term TOS and proposed a possible neurocompressive etiology for patients who presented with symptoms affecting the upper extremity [5]. Furthermore, Peet classified TOS based on presenting symptoms as Neurogenic, Venous, and Arterial disease. To a large extent, Peet’s classification of TOS by symptoms rather than the underlying pathophysiologic condition gave rise to the many controversies surrounding TOS today. A better understanding of TOS needs to begin with an understanding of the historic background to the conditions that affect the upper extremity which present with the variety of symptoms that have been attributed to the nerves and the blood vessels. Understanding the history will serve to clarify the many misunderstandings which are responsible for the controversies associated with TOS. Furthermore, a better understanding of the historical background will enable the distinction between the two entities that erroneously have been combined under TOS, Cervical Rib Syndrome (CRS) and the conditions that affect the thoracic outlet. Most importantly, a better understanding of this history will prevent repeating the past and allow for a more accurate diagnostic and therapeutic strategy for TOS.
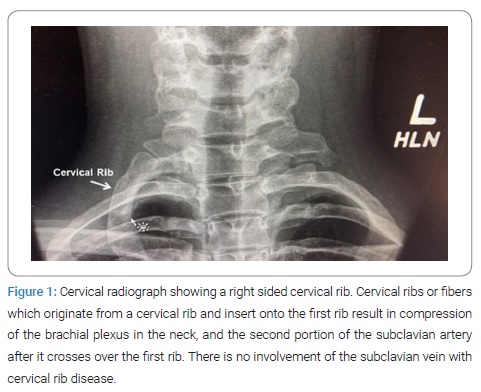
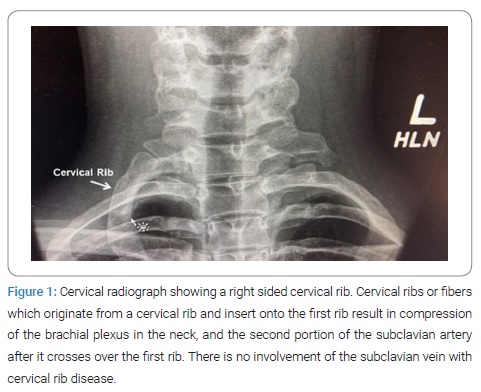
Historical narrative first century: The cervical rib was first described in 150 A.D. by Galen, the Greek anatomist and court physician to Marcus Aurelius. As at that time, human dissection was forbidden and thereafter remained forbidden for several centuries, to a large part, Galen’s anatomic observations were based on the dissection of apes [6] (Figure 1).
Seventeenth century: In 1615, Helkiah Crooke, who served as Court physician to King James I of England and was appointed as the Keeper of Royal Bethlem Hospital, described cervical ribs in Humans [7]. In the book, Mikrokosmographia: A Description of the Body of Man, he described cervical ribs as They are commonly both in men and in women on each side twelve, oftener more than fewer. For Nature would rather there should be an abundance than want. Thereafter, Bauhine found thirteen on each side; the first on the left side was perfect, but the first on the right side was imperfect. Fallopius also twice found one too many; Columbus once described eleven at Padua.
Eighteenth century: In 1743, François Joseph Hunault described and categorized human supernumerary ribs, including cervical ribs.
Nineteenth Century: Cervical Ribs: Subclavian Artery Compression and Aneurysm: Until 1818, clinical and symptomatic manifestations of cervical ribs were unknown. In that year, Sir Astley Cooper, the English surgeon and sergeant surgeon to Kings George IV and William IV, and to Queen Victoria, and founder of the famous medical school at Guy’s Hospital in London, described a young woman with pulselessness and gangrenous spots on her fingers, in conjunction with a palpable hard mass at the base of the neck [8]. Cooper described, I have however seen an exostosis arise from the sixth or seventh cervical vertebra, or perhaps from both. Cooper attributed the patient’s symptoms to a projection of the lower cervical vertebra towards the clavicle, and consequent pressure upon the subclavian artery. Although this was a landmark discovery, unfortunately the future generations of physicians referred to the compression of the subclavian artery by a cervical rib anomaly as TOS as opposed to Cooper’s original and more accurate description of CRS.
In 1831 H. Mayo provided the first description of a subclavian artery aneurysm associated with a cervical rib [9]. In 1853, John Hilton, a British surgeon, described gangrene in a patient with compression of the subclavian artery caused by an exostosis of the first rib [9]. In 1861, Holmes Coote, another English surgeon, performed the first Surgical Procedure for Cervical Rib Syndrome (SPCRS) [10]. The patient was a 26-year-old woman who presented with a hard mass in the left lower neck, which was present since childhood. The tumor had grown, and she experienced paresthesia in the tips of her fingers, with loss of pulses at the wrist, wasting of muscles in the arm, and weakness leading to dropping of items. Coote explored the area while the patient was fully under the influence of chloroform. He noted a bony ‘tumor,’ which he had to divide from the cervical vertebra. He also found it was attached to the first rib anteriorly. He removed as much of the ‘tumor’ as he could, and pulse returned in the left upper extremity. The bony tumor was referred to as an exostotic growth from the transverse process of the seventh cervical vertebra and a development of the costal element, the rib, of the seventh cervical vertebra. Interestingly Coote described the same trepidation experienced by modern surgeons in treating CRS but the region was not a pleasant one for any proceeding demanding the use of the knife. The subclavian artery and vein were in front; the axillary plexus of nerves lay spread out above; below, the apex of the lung, covered by the pleura, rose in dangerous proximity; on the scalenus was the phrenic nerve; while towards the mesial line were the important vessels and nerves passing to the head, together with the vertebral vessels and thoracic duct. You can understand, therefore, why I was cautious in what I did.
In 1869, Gruber published a classification system for cervical ribs. His classification was based on the length of the cervical rib and its attachment to the first rib. This classification remains relevant today [11,12].
- Type: Cervical rib extends to the transverse process of C7.
- Type: Cervical rib extends beyond the transverse process with no connection to the first thoracic rib.
- Type: Cervical rib extends beyond the transverse process with partial fusion to the first rib by fibrous bands or cartilage.
- Type: Cervical rib is completely fused to the first rib by a bony pseudo-articulation.
In 1884, Gould described a 19-year-old laborer who had pain, weakness, and coldness of his right hand. Gould found a cervical rib on examination, and he could create turbulence within the adjacent subclavian artery by pressing on it. Years later, the right arm pulse disappeared, and weakness appeared in the left arm. This was the first description of what was presumed to be an embolic stroke associated with thrombosis of the subclavian artery resulting from Cervical Rib Disease [12].
Twentieth century: In 1927, C.P. Symonds described two patients with left-sided weakness from a presumed stroke, who also had right-sided cervical ribs. For the first time, Symonds hypothesized a mechanism that related the two processes. Symonds suggested that the cervical rib caused damage to the right subclavian artery, resulting in blood clot formation. In turn, the blood clot extended proximally towards the heart until it entered the right common carotid artery. At this point, clot fragments broke off and traveled to the brain, resulting in a stroke [13]. In 1906, H. Lewis Jones described six patients with atrophy of hand muscles, preceded years before by pain and tingling. He found a strong correlation between symptoms and the presence of cervical ribs [14].
Cervical Ribs: Compression of the Brachial Plexus: In 1902, Farquhar Buzzard described seven patients with brachial plexus compression by cervical ribs [15]. In 1903, Edwin F. Bramwell described an 18-year-old plumber with sensory and motor disturbances in his left arm. Bramwell found hand weakness, with atrophy of intrinsic hand muscles. Bramwell described the abnormality as a lesion of the first dorsal root. Bramwell proposed the ‘sharp internal border of the first rib’ had caused nerve trauma. In H. Lewis Jones published the first described case of upper extremity nerve compression symptoms in association with a cervical rib [16]. In 1905, John Benjamin Murphy of Chicago resected a cervical rib in the treatment of the aneurysm of the subclavian artery [17]. In 1907, William Williams Keen, a Philadelphia Neurosurgeon, reviewed 42 known cases of cervical rib resection and described the clinical presentation and surgical treatment for CRS [18]. In 1916, William Halsted of Baltimore collected 716 cases of cervical ribs, which were reported in the literature, and found 27 (3.7%) patients with subclavian artery aneurysms [19].
Cervical ribs: anterior scalene muscle: In 1927, Alfred Washington Adson, who described the Adson’s Test, and Jay Coffey, both on the staff of Mayo Clinic, described the anterior scalene muscle as the cause of neurovascular compression in patients with cervical ribs [20,21]. They advocated Scalectomy or Scalenotomy without removal of the cervical rib as a treatment for CRS. With this procedure, the recurrence rate of symptoms was high, and the procedure was eventually abandoned. Interestingly, these investigators most likely, and erroneously described the fibrous connection from the cervical rib to the anterior scalene tubercle of the first rib as the scalene muscle. In modern surgical practice, the division of this fibrous band is mandatory for the release of the brachial plexus. However, the cervical rib also needs to be removed as it will continue to impinge onto the brachial plexus and the subclavian artery. This is the most likely explanation for the high recurrence rates which were experienced by Adson and Coffey.
In 1931, ed. Telford and John Sebastian Bach Stop ford described compression of the sympathetic fibers of the lower trunk of the brachial plexus by an aberrant cervical rib which resulted in small vessel ischemia of the hands [22]. They differentiated this condition from Raynaud’s syndrome or other conditions which result in small vessel disease in the upper extremity.
Cervical Ribs: erroneous association with Subclavian Vein Thrombosis: Cervical Rib Syndrome (CRS) was recognized as the sequela of the compression or displacement of the subclavian artery by an aberrant cervical rib. In 1875, Sir James Paget of London, and in 1884, Leopold von Schroetter of Vienna independently described thrombosis of the subclavian vein in young patients [23,24]. The syndrome resulting from the thrombosis of the subclavian vein carries their name, Paget-Schroetter Syndrome (PSS). Although these investigators did not associate subclavian vein thrombosis with CRS, unfortunately, in later years these two very different diseases have been erroneously associated under TOS.
Cervical Rib Syndrome without a Cervical Rib: Until 1902, SRS was thought to affect only the subclavian artery. Up to that time, SRS was defined as compression of the second portion of the subclavian artery in the neck by an abnormal cervical rib or associated fibrous bands. That year, for the first time, Farquhar Buzzard described seven patients with neurologic symptoms of the upper extremity whose symptoms were attributed to compression of the brachial plexus by a cervical rib [15]. Thereafter, CRS was defined as: neurovascular symptoms in the upper extremity which resulted from compression of the subclavian artery or the brachial plexus in the presence of a cervical rib [16]. The diagnosis of SRS was facilitated by the advent of X-ray technology at the turn of the twentieth century. Prior to surgical intervention, X-rays provided an objective means of imaging and recognizing cervical ribs for the first time. On the other hand, X-ray technology also confused some more, as many patients had upper extremity neurovascular symptoms like those in patients with SRS but without a cervical rib on X-ray. This gave rise to the curious concept of CRS without a cervical rib. In 1910, Thomas Murphy of Melbourne, Australia, performed the first resection of a normal first rib to treat a patient with upper extremity nerve-related symptoms without a visible cervical rib on X-ray [17].
The patient was a 28-year-old woman with symptoms of brachial plexus compression. X-rays showed no cervical rib, but Murphy was convinced the brachial plexus was compressed. Murphy performed surgery, finding the broad insertion of the anterior scalene was compressing the brachial plexus. He removed the insertion and a small part of the first rib. The patient had some but not complete relief in symptoms. In 1919, John Sebastian Bach Stopford and E. D. Telford of England described Compression of the lower trunk of the brachial plexus by the first rib and reported results from 10 patients following resection of the first rib.
In 1920, Arthur Ayer Law described abnormal cervical soft tissue bands that compressed the neck’s neurovascular structures [25]. In 1937, Howard Christian Naffziger and Francis Clark Grant, were the first to advocate scalenotomy in patients without cervical ribs [26]. Following this description, Alton Ochsner, Mims Gage, and Michael DeBakey published a comprehensive study of patients with symptoms of neurovascular compression in the upper extremity in the absence of a cervical rib, for which they coined the term Scalenus Anticus Syndrome or Naffziger Syndrome [27]. Scalenectomy alone was associated with poor results. In 1939, Eden, and later in 1943 Falconer and Weddell, proposed compression of neurovascular structures between the clavicle and the first rib [28,29]. Falconer and Weddell’s observations were based on symptoms in the upper extremity of young recruits who carried heavy backpacks. They coined the term Costoclavicular Syndrome (CR). The existence of this syndrome remained controversial, although, in 1962, Falconer and Li described a series of 11 patients who underwent first rib resection with good results [30]. Interestingly, in 1945, Irving S. Wright, who described the Wright’s test, described patients with similar symptoms and signs as those with CR. However, Wright’s patients experienced nerve-related symptoms with an elevation of the arms above the head. Interestingly, Wright could not produce pulse obliteration (Adson’s Test) in his patients. Furthermore, Wright described pulse obliteration with hyperabduction of the upper extremity in nearly 90% of asymptomatic normal volunteers and concluded that the Adson’s test did not correlate with compression of the brachial plexus. After extensive anatomic dissections, Wright proposed that ischemia of the nerves due to impaired blood supply as opposed to direct nerve compression may be the mechanism for symptoms elicited by hyperabduction of the upper extremity [31]. Concept of TOS In 1956, Peet and colleagues first used TOS to unify many upper extremity neurovascular compression syndromes [5]. In 1958, Rob and Standeven used Thoracic Outlet Compression Syndrome to describe a series of patients with cervical ribs, arterial thrombosis, and distal gangrene of the upper extremity [32]. Clearly, these patients would have been better and more accurately classified as CRS. This unfortunate attempt to unify a group of disparate anomalies which manifest with upper extremity neurovascular symptoms began an era that has been characterized by confusion about the underlying pathogenesis, confusion about the appropriate diagnostic tests, and poor therapeutic results. In 1962, responding to the poor results associated with splenectomy alone, O.T. Claggett, a Thoracic Surgeon at Mayo Clinic, proposed first rib resection through a high posterior thoracotomy [33]. Results of first rib resection with this approach were confusing as the preoperative upper extremity morbidity could not be differentiated from postoperative surgical morbidity resulting from the thoracotomy incision. On the one hand, patients presented with upper extremity symptoms preoperatively, but on the other hand, the very invasive surgical procedure resulted in additional upper extremity morbidity following surgery.
In 1966, in seeking to obviate the morbidity associated with Clagett’s high posterior thoracotomy approach, David Roos described a trans-axillary approach to first rib resection [34]. Despite widespread acceptance, in the experience of most surgeons, the Roos trans-axillary approach is associated with neurovascular complications, at times erroneous resection of the second rib, and overall poor or incomplete relief of symptoms [35,36].
In response to the inconsistent results of first rib resection, in 1972, Silver and Vemuri attributed some of the failures after first rib resection to the compression of the brachial plexus in the retro-pectoral space. They suggested pectoralis minor tenotomy, either in isolation or in addition to first rib resection [37,38]. This was a rediscovery of a technique advocated two decades earlier by Lord and Stone for Effort Thrombosis and Hyper abduction Syndrome with inconsistent results [39].
In 1979, Sanders introduced supraclavicular splenectomy in patients with recurrent symptoms following first rib resection for post-traumatic upper extremity symptoms. Splenectomy was later used as the primary treatment in upper extremity symptoms following neck trauma patients [40]. Unfortunately, as illustrated by the history of TOS, due to the ongoing confusion and the poor and inconsistent surgical results, surgeons have extrapolated from this experience and have erroneously advocated splenectomy with or without resection of the first rib for patients without neck trauma.
In the near six decades since Peet’s report, confusion about TOS and the poor results with surgical intervention has continued. During this time, a great deal of attention has been focused on the surgical approach to the resection of the first rib and whether other procedures such as splenectomy, neurolysis, and pectoralis minor tenotomy should be included with a first rib resection. However, irrespective of the approach and the specifics of the surgical procedures, the results of surgery have been disappointing [41,42].
History of Terms used to describe Upper Extremity Neurovascular Symptoms: Cervical rib syndrome: The first actual use of the term CRS is by T. Wingate Todd in 1922 CRS was the most well-known and widely used name for the syndrome throughout the late 19th century and into the early 20th century. Although, recently, this term has fallen into disfavor, in reality, CRS is an accurate description which should be reserved for neurovascular symptoms of the upper extremity caused by compression of the cervical ribs or the related anomalous bands on the brachial plexus or the extra-thoracic portion of the subclavian artery in the neck. CRS is rare within the group of disorders that result in upper extremity symptoms. Unfortunately, many who are not familiar with these conditions erroneously think that a cervical rib is responsible for TOS. The correct use of the term CRS plays an important role in the modern understanding of conditions that are responsible for Upper Extremity Neurovascular Symptoms.
Brachial compression neuritis: This term was first used by Stopford in 1919 [43]. Although this is a reasonable attempt at describing compression of the brachial plexus in the neck, it is too general and does clearly convey the cause of such compression. CRS is a more accurate description of what results in brachial compression neuritis.
Scalenus anticus syndrome (Naffziger syndrome) Scalenus antics is another name for the anterior scalene muscle. As noted previously, Adson and Coffey wrote a landmark paper in 1927 describing their approach of detaching the scalenus anticus from its insertion on the first rib in patients with a cervical rib [20,21]. Ochsner, Gage, and DeBakey, in 1935, were the first to describe patients with CRS without a cervical rib who had been treated successfully with the same procedure [27]. They first used the term Scalenus Anticus Syndrome, but credited their work to Howard Naffziger, and suggested the term Naffziger Syndrome as well. Our present understanding of etiology of TOS would lead us to believe that although these authors accurately observed that there was compression of the subclavian vein at the medial aspect of the first rib, they erroneously attributed the compression to a hypertrophied anterior scalene muscle as opposed to a congenital abnormality of the first rib in the region of the insertion of the anterior scalene muscle, the anterior scalene tubercle.
Costoclavicular syndrome/Costoclavicular compression syndrome: Eden first described the mechanism of compression between the clavicle and first rib in 1939 to explain vascular compression [28]. Falconer and Weddell in 1943 described further cases with vascular compression [29,30]. CR was first used by Telford and Mottershead in 1947 [44]. There was the observation that in patients with Upper Extremity Neurovascular Symptoms, the subclavian vein was compressed on the medial aspect of the first rib at is “v” junction with the clavicle. In retrospect, this is a different interpretation of an observation of a phenomenon that was interpreted by other investigators as the Scalenus anticus syndrome (Naffziger syndrome).
Hyperabduction syndrome/ Wright Syndrome: Beyer and Wright first used the term ‘hyperabduction syndrome’ in 1951 [45]. This descriptive term was based on the observations of Todd from 1913 to 1921 and Wright in 1945, who observed exacerbation of the Upper Extremity Neurovascular Symptoms with hyperabduction of the upper extremity above the shoulder [31]. Once again, these instigators made similar observations in terms of compression of structures by a process in the medial aspect of the first rib. In addition, they emphasized that hyperabduction resulted in exacerbation of symptoms by further narrowing the space between the first rib and the clavicle.
Brachiocephalic syndrome/ brachiocephalic vascular syndrome: In 1966, J.D. Devilliers first used ‘brachiocephalic vascular syndrome’ to describe a young woman with a stroke related to arterial TOS and a cervical rib [46].
Nocturnal paresthetic brachialgia? brachialgia statica paresthetica: This term was introduced by Wartenberg in 1944 [47]. It refers to the same phenomenon as the Hyperabduction syndrome/ Wright Syndrome, Paget-Schroetter Syndrome/effort Thrombosis of the Subclavian Vein/Axillary-Subclavian Vein Thrombosis (ASVT): In 1875, Sir James Paget described two patients with spontaneous swelling of one arm and prominence of veins over the ipsilateral chest. Paget thought the condition was caused by vasospasm. In 1884, Leopold von Schroetter independently described patients with the same condition and correctly attributed the clinical condition to the formation of occlusive venous thrombus. In 1949, Hughes performed a review of a large number of cases in the medical literature and proposed the term Paget-Schroetter Syndrome, which is still in use today [48]. von Schroetter suspected that an episode of considerable exertion of the upper extremity precipitated the thrombosis. In 1942, Swartley first used the term ‘effort thrombosis’ [49]. In Peet’s attempt at consolidating all Upper Extremity Neurovascular Symptoms under TOS, Paget Schroetter Syndrome (PSS) became synonymous with Venous TOS.
Cervicobrachial syndrome: Kenneth Aynesworth first used this term in a paper published in 1940, in which he described CRS under a different designation [50]. It was used again by Hansson in 1941, but since then, the name has not come into common use [51]. First thoracic rib syndrome/Superior outlet syndrome/Fractured clavicle-rib syndrome/Cervical rib and band syndrome: According to Werden’s exhaustive literature review, these miscellaneous names are of uncertain origin and have never come into common use [52].
Thoracic Inlet Syndrome: Specifically, Thoracic Inlet is the space defined by the opening into the chest cavity, which allows for the entry of vessels, the trachea, the esophagus, and other midline structures. Although some have tried to use this as a synonym for Thoracic Outlet, clearly by convention, it relates to a different anatomic entity and should not be used in referring to compressive syndromes relating to patients with neurovascular symptoms of the upper extremity.
Pectoralis minor syndrome: In 1967, Erich Lang first referred to the pectoralis minor syndrome [53]. This concept was built on a body of work by Jere Lord and Peter Stone in 1956, who performed the first documented pectoralis minor tenotomy in 5 patients diagnosed with hyperabduction syndrome [39]. Although this condition may be a rare cause of upper extremity neurovascular symptoms, regrettably, in response to the poor surgical results with TOS, some modern surgeons have incorporated pectoralis minor tenotomy to procedures for TOS. Clearly, there is very little objective evidence for this practice.
Cervicodorsal syndrome: First described by Nelson in 1957 in an attempt to simplify and group the various neurovascular syndromes of the upper extremity, this term has not come into common use [54].
Cervicoaxillary syndrome: In 1996, Ranney proposed this term to include subclassifications’ cervical outlet syndrome,’ TOS, CS and pectoralis minor syndrome and to eliminate thoracic inlet syndrome [55]. This is yet a more recent attempt to group a number of etiologies resulting in upper extremity neurovascular symptoms. Such attempts at consolidation of disparate entities with upper extremity neurovascular symptoms will most likely increase the confusion that surrounds TOS.
Thoracic outlet syndrome/thoracic outlet compression syndrome: In 1956, Peet proposed consolidating all conditions with many names and syndromes under TOS. In an attempt to clarify the various conditions that have been classified as TOS, investigators have described three types: Neurogenic, Venous, and Arterial. Most experienced investigators have discovered that classifying multiple closely related conditions under a single umbrella term results in confusion about the important differences among these conditions that are associated with different pathologic etiologies. The creation of the term ‘thoracic outlet syndrome’ was an unfortunate simplification that is not consistent with the present understanding of the etiologic entities that are responsible for upper extremity neurovascular symptoms in patients. Given the confusion in terms of diagnosis and therapy that surrounds the diverse group of disorders placed under the umbrella of Thoracic Outlet Syndrome, future efforts should concentrate on the separation of the different etiologic entities that result in neurovascular symptoms in the upper extremity. Results of surgery can only be improved through a clearer understanding of the specific etiologic entities and the application of surgical procedures which directly address the specific pathologic processes. In turn, the specific underlying pathology needs to be diagnosed preoperatively with a high degree of certainty. TOS Conventional Thinking about TOS: Since Peet’s classification of TOS in 1956, conventionally TOS has been thought to represent a group of diverse disorders that result in compression of the neurovascular bundle exiting the thoracic outlet. The thoracic outlet has been defined as the triangular anatomical area between the clavicle and the first rib and the neck muscles which allows for the passage of the brachial plexus, subclavian artery, and subclavian vein. Compression of this area has been thought to result in a constellation of distinct symptoms, which can include upper extremity pallor, paresthesia, weakness, muscle atrophy, pain, and swelling [56,57].
Until recently, TOS classification has been based on symptoms, rather than the underlying pathology; with the subgroups consisting of Neurogenic (NTOS), Venous (VTOS or PSS), and Arterial (ATOS). Neurogenic TOS (NTOS) can be further divided into true and disputed NTOS, with disputed reportedly representing 95%–99% of all neurogenic cases [58]. The symptoms of true and disputed NTOS are largely the same, though objective findings from motor nerve conduction studies and needle electromyography are notably absent in the disputed NTOS. The true incidence of TOS is difficult to discern. However, depending on the definition and diagnostic modality, the incidence of TOS has been reported to range from 3/1000 to 80/1000. Neurogenic TOS accounts for over 95% of the cases, followed by venous (3%–5%) and arterial (1%–2%) [59]. Historically, TOS presents with symptom onset in the second to the sixth decade of life. The demographics are different for the three types of TOS. It has been reported that NTOS is more prevalent in women with a female to male ratio of 4:1 [60]. True NTOS most commonly affects a younger woman in their teenage years and is usually unilateral. Disputed NTOS is most commonly seen in women ranging from their 20’s to 60’s and is often bilateral [59]. ATOS affects both genders equally and is mostly seen in young adults. ATOS is predominantly unilateral. VTOS which presents as Paget Shroetter Syndrome, is more common in younger able-bodied individuals, most commonly affects the dominant upper extremity and is associated with repetitive upper extremity activity [60,61]. The different demographics of these entities is an important clue to the etiology of these disease processes and has been ignored in Peet’s classification of TOS.
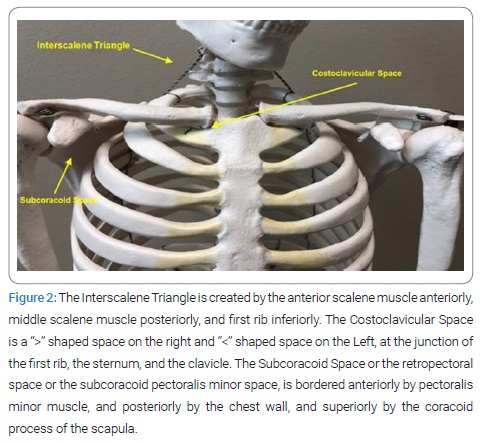
Etiology of TOS: Peet’s classification of TOS was based on the concept of the compression of the neurovascular structures in the neck and upper chest, which gave rise to the symptoms. Accordingly, in searching for a hypothetical anatomic area where compression of the neurovascular structures occurs, three spaces were identified: interscalene triangle, costoclavicular space, and subcoracoid space [61] (Figure 2).
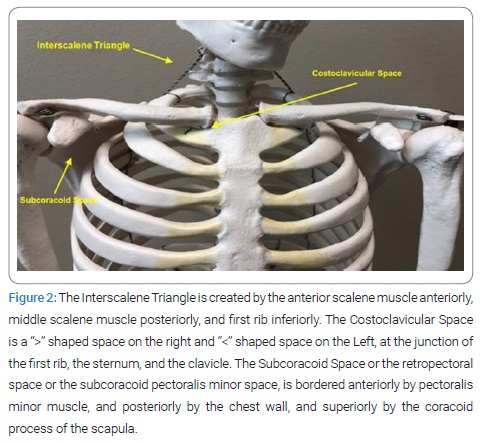
The Interscalene Triangle is created by the anterior scalene muscle anteriorly, middle scalene muscle posteriorly, and first rib inferiorly. These structures create an elongated isosceles triangle. The brachial plexus passes through the apex of this triangle in the neck and has no proximity to the first rib. On the other hand, the subclavian artery passes at the base of the triangle as its course over the first rib. The subclavian vein has no relationship to this triangle. The Costoclavicular Space is a “>” shaped space on the right and “<” shaped space on the Left, at the junction of the first rib, the sternum, and the clavicle. It is bordered by the costo-sternal joint medially, the anterior scalene muscle postero-laterally, and the first rib inferiorly at its base. The subclavian vein passes through this compartment and the subclavian artery crosses the first rib just posterior to this compartment. The subclavian vein and artery are separated by the insertion of the anterior scalene onto the first rib. The Subcoracoid Space or the retropectoral space or the subcoracoid pectoralis minor space, is bordered anteriorly by pectoralis minor muscle, and posteriorly by the chest wall, and superiorly by the coracoid process of the scapula [62,63]. The brachial plexus passes through the subcoracoid space, and the subclavian artery and vein continue through it as the axillary artery and vein. The unifying characteristic of the classification of patients with neurovascular symptoms of the upper extremity into TOS by Peet and propagated in the past six decades has been compression of the neurovascular structures by an anatomic entity in the neck and upper chest.
Mechanism of compression has been: Physical Examination: Included in the physical exam are Individual provocative maneuvers. These include: Trauma: This includes midshaft clavicle fractures, whiplash injuries, or hemorrhage in the neck and upper chest [59,60]. Muscle Hypertrophy and Fibrosis: It has been hypothesized that repetitive activity results in fibrosis and eventual compression of nerves and vessels. VTOS or PSS has been attributed to this mechanism with thrombosis following the repetitive motion of the upper extremity, such as in athletes.
Anatomic anomalies: This includes Cervical Ribs and associated fibrous bands that originate from them and insert onto the first rib, or supernumerary scalene muscles [64]. Benign or malignant tumors of the structures in the neck and upper chest [65,66].
Diagnosis of TOS: Historically confusion about the pathogenesis of TOS has resulted in a number of diagnostic tests. Conventionally diagnosis of TOS has been one of exclusion. Pts. Presenting with upper extremity neurovascular symptoms need to undergo: Physical Examination: Included in the physical exam are Individual provocative maneuvers. These include:
- Adson’s Test- In 1927, Adson and Coffey [20,21]. Described a technique to assess evidence of circulatory symptoms caused by the presence of a cervical rib. Diminution in the volume of the radial pulse is common; the pulse can be decreased or obliterated by having the patient elevate the chin or rotate the head to the affected side while inspiring air. They believed that this evidence of circulatory disturbance warranted consideration for surgical resection of the cervical rib. Over the years the Adson’s test was thought to be the sign of CRD that was erroneously applied to TOS. Adson’s test is associated with minimal inter-examiner reliability, is seen in normal individuals, and is inconclusive for the diagnosis of TOS. The arm is maximally extended and abducted 30° at the shoulder. The patient inhales deeply while extending the neck and turning head towards ipsilateral shoulder. A positive test is signaled by a decrease or absence of ipsilateral radial pulse.
- Wright’s Test: This test was first described by Irving S, Wright in 1945 [31]. With a positive Wright’s Test, the radial pulse weakens or disappears when the arm is abducted and externally rotated. As with Adson’s test, Wright’s test is associated with minimal inter-examiner reliability, is seen in normal individuals, and is inconclusive for the diagnosis of TOS.
- Roos (East) Test- The arms are raised above the shoulder, abducted to 90°, and in externally rotated, with elbows flexed to 90°. The patient slowly opens and closes hand for 3 min. A positive test is signaled by pain, paresthesia, a feeling of heaviness and weakness in the affected extremity.
- Elvey (ULTT) Test- Arms are placed in 3 positions: Position 1: arms abducted to 90° with elbows flexed, Position 2: active dorsiflexion of both wrists, Position 3: head is tilted ear to shoulder, in both directions. A positive test is signaled by symptoms in the ipsilateral side in Positions 1 and 2, and symptoms in the contralateral side in Position 3. Provocative test for TOS are not specific. Overall these maneuvers have led to a high number of false positives and are not helpful in making a definitive diagnosis [67–71].
Diagnostic Tests: Diagnostic tests include Neck Radiographs, Pulse volume recordings, Dopplers of the upper extremity vessels, CT of the chest, MRI of the cervical spine, MR Angiogram of the upper extremity vessels in the thoracic outlet, subclavian vein and artery angiography, Electrodiagnostic testing by EMG, and Nerve conduction studies.
Imaging: In patients with suspected VTOS and ATOS, ultrasound maintains high sensitivity and specificity, is noninvasive and inexpensive, and should be the initial imaging test of choice. CT can differentiate equivocal cases or provide additional anatomic detail required for surgical planning [71]. MR neurogram can provide further detail to identify anatomical relationships or sites of compression. Conventional arteriography and venography can demonstrate extrinsic compression. However, angiography is hampered by the fact that it is perceived as an invasive test with potential complications and therefore is used seldom, and the fact that it does not depict the impinging anatomic structure. As a result, Magnetic Resonance Angiogram (MRA) which overcomes these shortcomings has become the test of choice in patients with all types of TOS [71].
Nerve Conduction and EMG: Invariably, patients suspected of NTOS undergo this testing. This testing is mainly used to rule out cervical radiculopathy and myelopathy, not to rule in NTOS [72,73]. In a small number of patients who have compression of C8 and T1 fibers, nerve conduction studies will be positive. The majority of patients with positive nerve conduction studies involving the C8 and T1 distribution have CRS. In these patients exhibit a characteristic pattern of nerve conduction abnormalities which includes a diminished or absent sensory response in the medial antebrachial cutaneous and ulnar nerves and diminished or absent median and ulnar motor response. It is important to emphasize that nerve conduction and EMG studies are not diagnostic in the vast majority of patients who present with neurovascular symptoms of the upper extremity and are suspected of having NTOS.
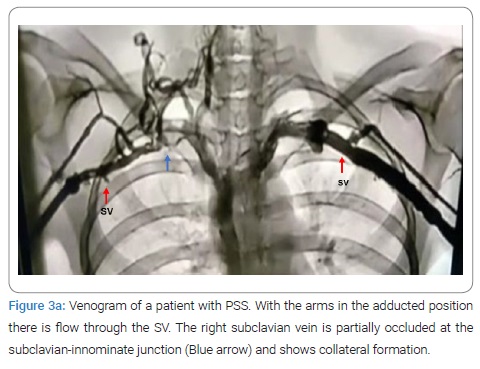
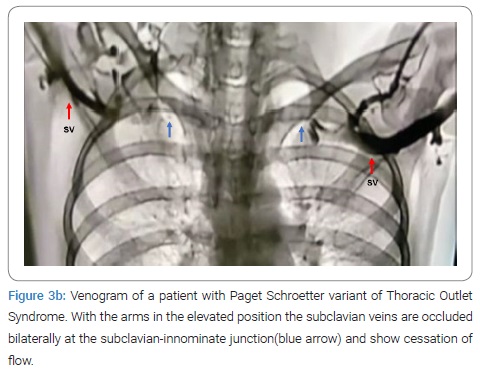
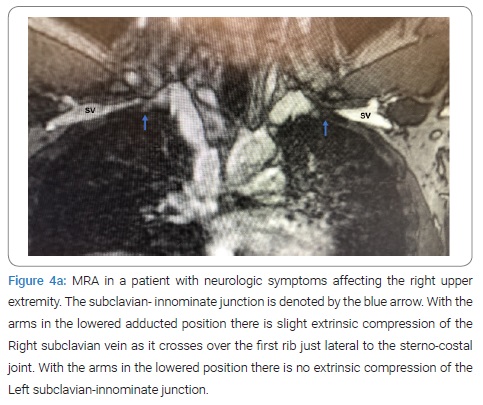
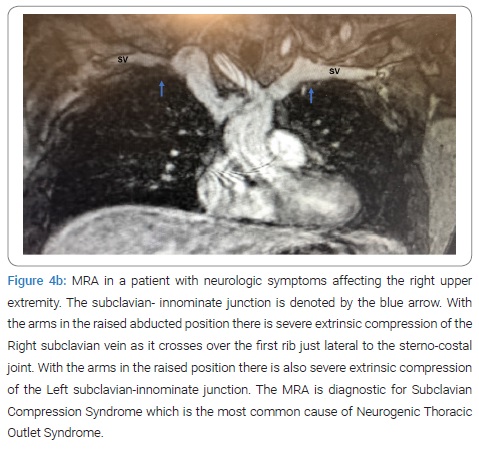
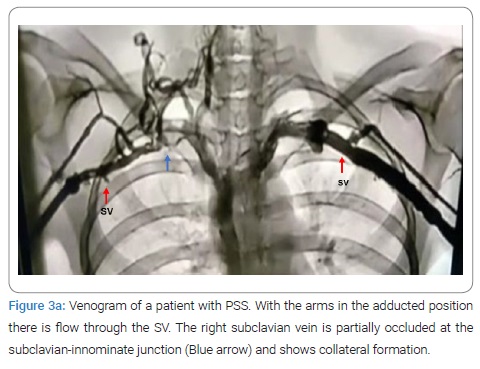
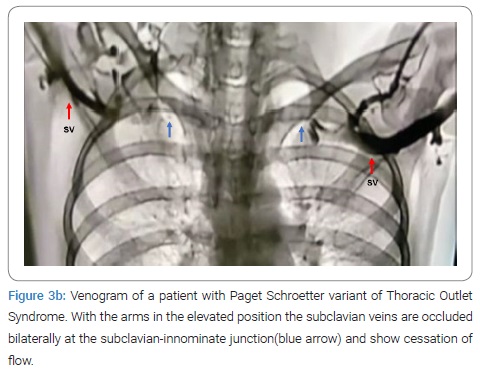
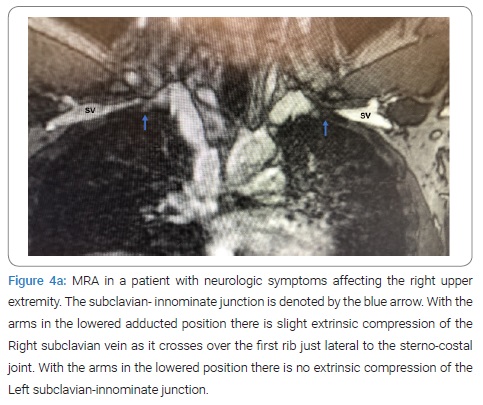
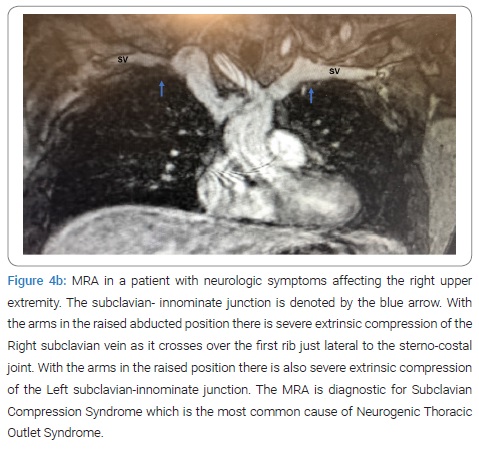
Anterior Scalene Block: Injection of local anesthetic into the anterior scalene muscle has been used to diagnose NTOS. It is postulated that the temporary relief of symptoms following medication injection decreases muscular tension on the neural bundle and may predict response to surgical decompression. This technique remains controversial, however, in one study, 94% of patients with a positive response to the block exhibited a positive outcome following surgical correction as compared to only 50% of patients who underwent decompression following a failed block [67]. As a general rule, except for angiography and dynamic MRA of the thoracic outlet with arm maneuvers, the other tests have been inconclusive and are of historical value (Figure 3, Figure 4). Presently MRA of the thoracic outlet with arm maneuvers is the test of choice in patients suspected of having TOS. This test shows the abnormal bony tubercle on the first rib with extrinsic compression of the subclavian innominate junction, which is exacerbated with an elevation of the arm above the shoulder. The predictive value of the surgical success of this test in patients with Paget Shroetter Presentation is 100%, and in patients with Neurologic Presentation is 100% and 97.3%, respectively [74].
Treatment: Treatment of ATOS and VTOS is not controversial. ATOS is usually the result of compression of the subclavian artery by an abnormality in the cervical region most often associated with CRS. In these patients the optimal therapeutic regimen includes initial thrombolysis and anticoagulation followed by removal of the cervical rib or bands that result in compression.
Management of VTOS or PSS consists of thrombolytic therapy and anticoagulation, followed by resection of the first rib. On the other hand, due to the confusion about the etiology of TOS and the poor surgical results, the treatment of patients with NTOS has been very controversial. As a result, in these patients, conservative management is recommended as the first line of therapy. Although there has been no consensus as to the appropriate conservative regimen, it has included patient education, postural mechanics, weight control, relaxation techniques, activity modification, active stretching, targeted muscle strengthening, TOS-specific rehabilitation, and pharmacologic therapies [75]. Pharmacologic interventions have included NSAIDs and/or opioid analgesics, muscle relaxants, anticonvulsants, antidepressants, local anesthetic injection, steroids, or botulinum toxin type A into the anterior scalene. Invariably conservative management has been associated with suboptimal results and poor patient satisfaction [76,77]. First rib resection with the hypothesized mechanism of decompressing the thoracic outlet has been recommended in patients with NTOS who fail conservative management, even without a specific diagnosis of the etiologic entity.
In the near six decades since Peet’s report, confusion about TOS and the poor results with surgical intervention has continued. During this time, a great deal of attention has been focused on the surgical approach to the resection of the first rib and whether other procedures such as scalenectomy, neurolysis, and pectoralis minor tenotomy should be included with a first rib resection. However, irrespective of the approach and the specifics of the surgical procedures, the results of surgery have been disappointing [41,42].
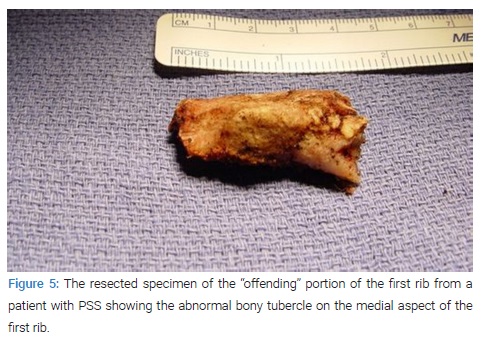
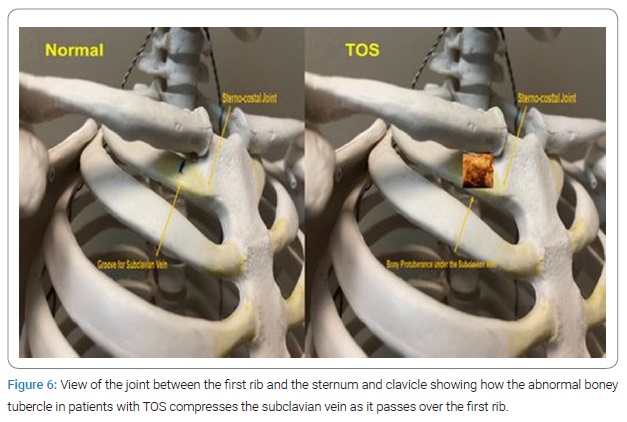
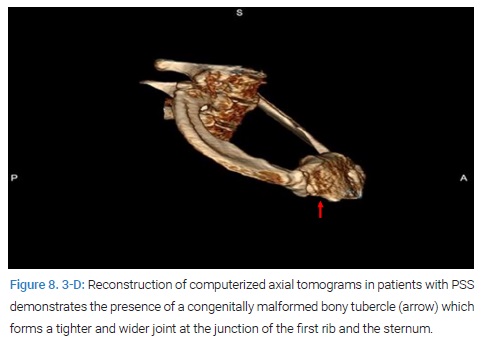
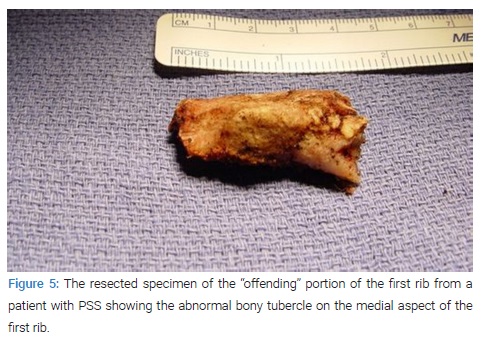
Pathogenesis of Paget Shroetter Syndrome: Recently, examination of the medial aspect of the resected first ribs in patients with Paget-Shroetter Syndrome has demonstrated the presence of a congenitally malformed bony tubercle which forms a tighter and wider joint at the junction of the first rib and the sternum [78]. In a number of patients with a wider tubercle there is even a second pseudarthrosis with the head of the clavicle [79,80] (Figure 5, Figure 6). It has been observed that the wider and less mobile cost-sternal joint locks the medial aspect of the first rib into place and results in extrinsic compression of the boney tubercle onto the subclavian vein at its junction with the innominate vein.
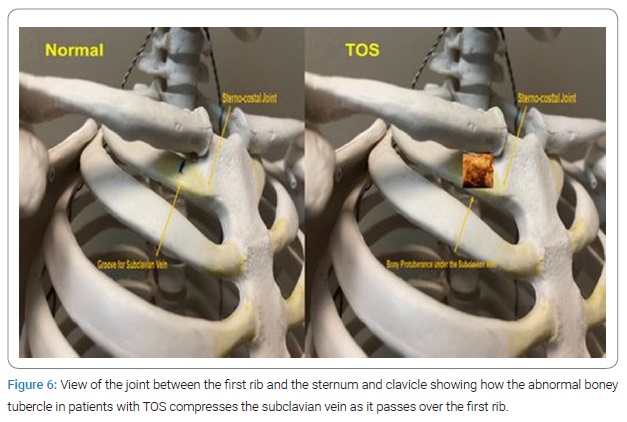
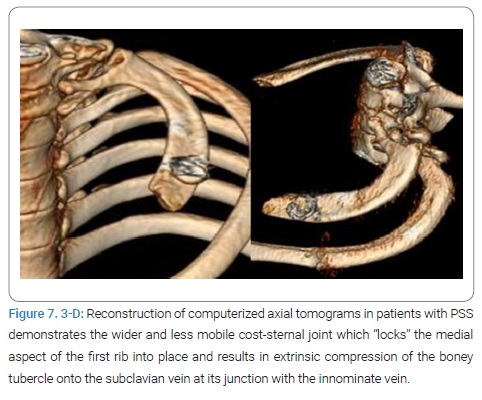
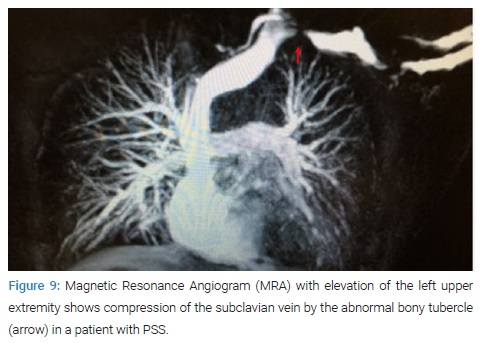
Therefore, the abnormal medial aspect of the first rib compresses the subclavian vein at the thoracic outlet. This abnormal tubercle on the medial aspect of the first rib can be seen on the 3-D reconstruction of computerized axial tomograms in patients with PSS (Figure 7, Figure 8). In addition, the extrinsic compression of the subclavian vein by the tubercle at the medial aspect of the first rib can be demonstrated on dynamic Magnetic Resonance Angiography (MRA) with maneuvers and dynamic Venography (Figure 9).
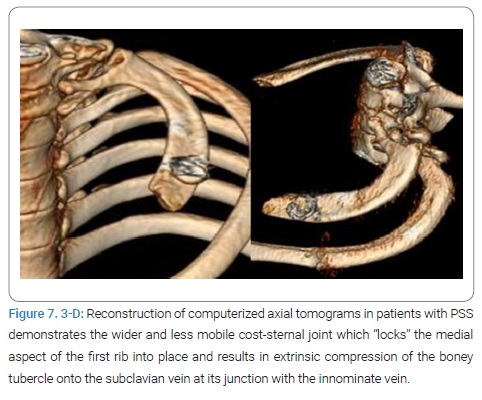
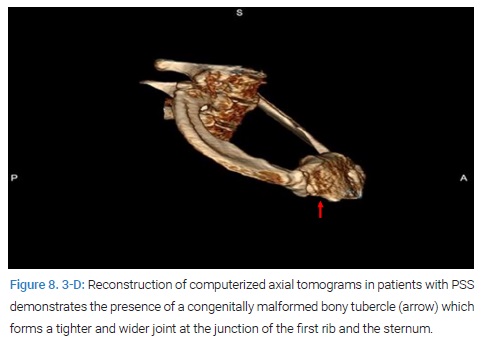
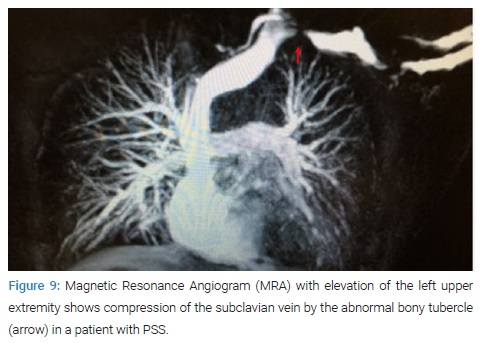
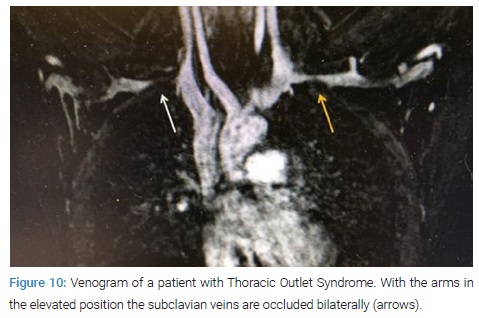
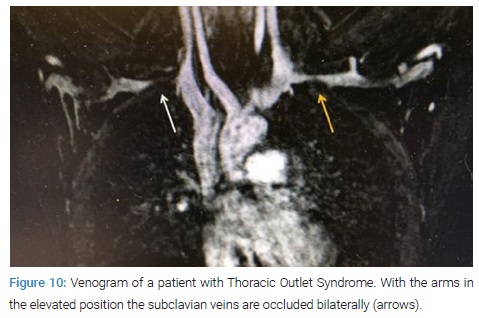
Furthermore, these studies clearly demonstrate that the subclavian vein compression increases with elevation of the arm above the shoulder. It can be surmised that without the benefit of the sophisticated modern imaging, and relying only on intraoperative observations, it is likely that historically surgeons have erroneously referred to this tubercle as the hypertrophied costoclavicular ligament, and the hypertrophied scaleneus anticus tubercle. In patients with Paget Shroetter Syndrome, Gharagozloo et. Al have demonstrated that disarticulation of the costosternal joint and resection of the offending portion of the first rib (portion of the rib medial to the subclavian artery) results in decompression of the subclavian vein [79,80]. Furthermore, preoperative dynamic MRA has been demonstrated to have a predictive value of 100% for surgical success in patients with Paget Shroetter Syndrome. In addition, dynamic MRA in patients with PSS has demonstrated the presence bilateral disease in the head of the first rib (Figure 10). This observation further clarifies reports of Paget Shroetter Syndrome affecting the contralateral extremity and supports the congenital pathogenesis of the disease.
Therefore, it has been suggested that Paget Shroetter Syndrome results from a congenital malformation of the first rib, which compresses the subclavian vein at its junction with the innominate vein in the thoracic outlet, and with prolonged compression stemming from activities that elevate the arm above the shoulder, result in thrombosis of the vein.
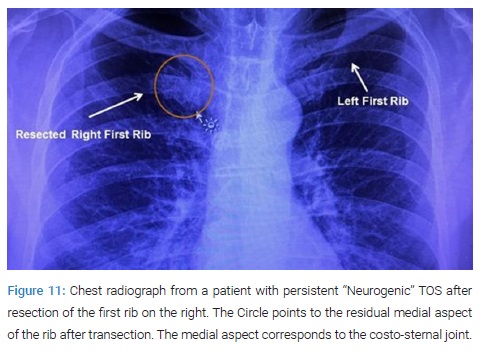
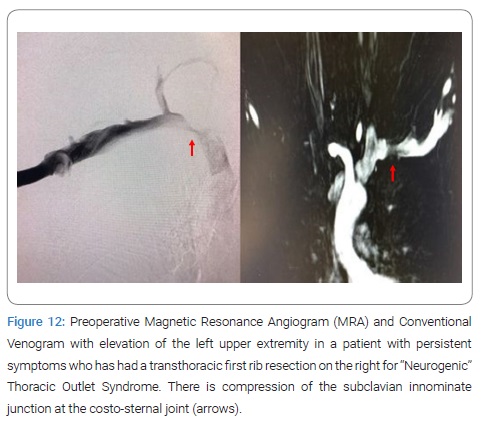
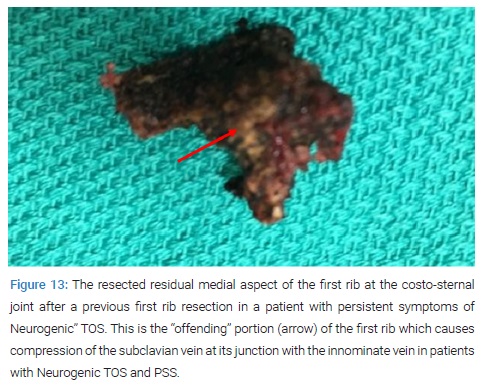
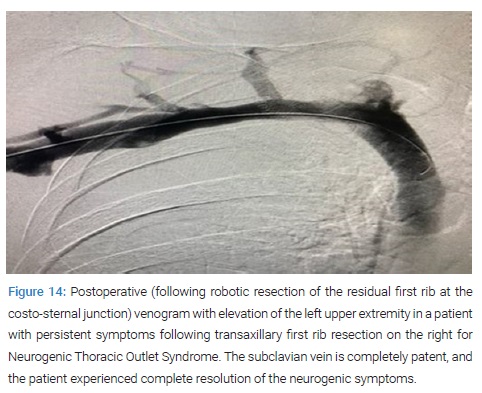
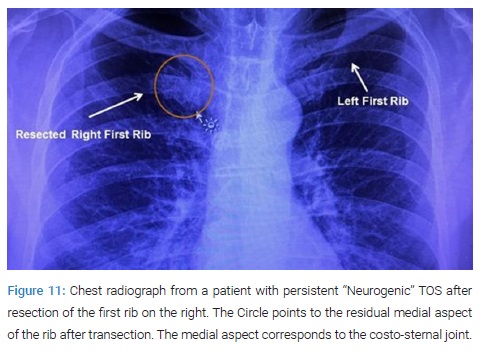
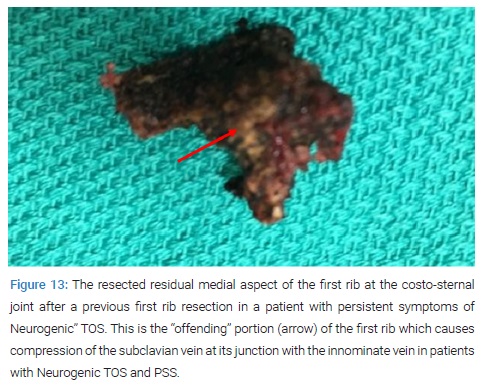
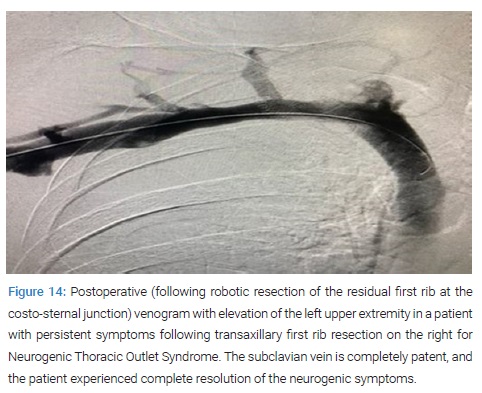
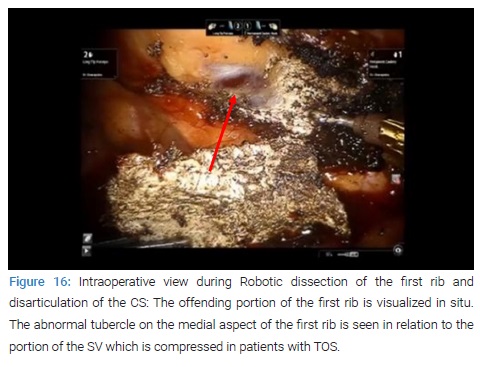
Pathogenesis of Neurogenic TOS: A study of patients with Neurogenic TOS who had persistent upper extremity pain following first rib resection by the transaxillary and supraclavicular approaches, revealed persistent extrinsic compression of the subclavian innominate junction on dynamic MRA. These patients underwent video-assisted exploration of the chest, which showed a persistent costo-sternal joint despite evidence for prior removal of the first rib. Disarticulation of the cost-sternal joint and removal of the remaining portion of the first rib which bore a tubercle similar to that which was seen in patients with Paget- Schroetter Syndrome (PSS), alleviated the extrinsic compression of the subclavian-innominate vein junction on postoperative dynamic MRA and resulted in relief of Neurogenic symptoms in all patients (Figure 11–Figure 14).
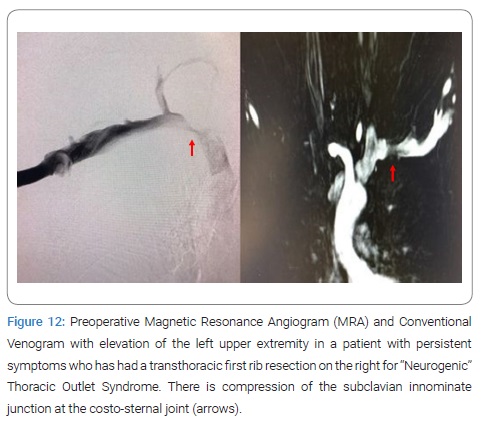
Based on this observation, it was hypothesized that Neurogenic TOS may be the manifestation of nerve pain which results from venous compression and the resultant venous ischemia of the nerves in the upper extremity. This hypothesis is based on the fact that the upper extremity is fed by a single artery and vein as an end organ. In such a setting, studies have demonstrated that the blood-nerve barrier in the nerve root was more easily broken by venous congestion than by arterial ischemia. Venous congestion may be an essential factor precipitating circulatory disturbance in nerve roots and inducing neurogenic intermittent claudication [81]. Therefore, compression of the subclavian vein at its junction with the innominate vein may result in elevation of venous pressure, a decrease in arterial flow, and relative ischemia of the nerves of the upper extremity. Venous ischemia of the upper extremity nerves may manifest as pain, tingling, paresthesia and numbness, and varying degrees of neurogenic intermittent claudication depending of the degree and duration of venous compression. Elevation of the extremity above the shoulder, may result in greater compression of the subclavian vein, further venous congestion, further decrease in arterial flow, greater degree of ischemia of the upper extremity nerves, and exacerbation of symptoms. This phenomenon is demonstrated on dynamic Magnetic Resonance imaging and venography (Figure 3, Figure 4). The pathophysiology of nerve pain in this setting has been likened to symptoms that result from crossing one leg over the knee. Only 5% of patients with the Diagnosis of Neurogenic TOS are found to have a Cervical rib and are best classified as CRS. 95% of patients with the diagnosis of Neurogenic TOS are believed to have neurologic manifestations of upper extremity ischemia and compression of the subclavian vein by an abnormal first rib at the thoracic outlet. Therefore, it was hypothesized that Robotic Transthoracic Resection of the Medial Aspect of the first rib at the costo-sternal junction in patients of Neurogenic TOS diagnosed by MRA will result in relief of symptoms. In a Proof of Concept Study, surgical outcomes in patients diagnosed with Neurogenic TOS who underwent robotic first rib resection were reviewed. Diagnosis was made by History, Physical Exam, MRI of C-Spine, Orthopedic and Neurologic examination, Nerve Conduction Studies, and MRA of the Thoracic Outlet with Maneuvers. Patients with Cervical Ribs or Cervical Bands were excluded.
Patients with compression of the Subclavian Vein by the medial aspect of the first rib underwent robotic resection of the first rib and were the subjects of this study. Subjective Symptoms were assessed by Disabilities of the Arm, Shoulder and Hand Questionnaire Score QuickDASH, 1 week, 1 month and 6 months. The QuickDASH is an abbreviated version of the original DASH outcome measure. In comparison to the original 30 item DASH outcome measure, the QuickDASH only contains 11 items. It is a questionnaire that measures an individual’s ability to complete tasks, absorb forces, and severity of symptoms. The QuickDASH tool uses a Five point Likert scale from which the patient can select an appropriate number corresponding to his/her severity level/ function level [82–84]. The extrinsic compression of the subclavian vein on postoperative MRA and Angiogram with Maneuvers was assessed at 1 month. In this proof of concept study, patients with Neurologic symptoms of the upper extremity who were classified as Neurogenic TOS had complete relief of symptoms with relief of compression of the subclavian vein after robotic resection of the medial aspect of the first rib and disarticulation of the costo-sternal joint.
Removal of the medial aspect of the first rib and decompression of the thoracic outlet has resulted in relief of upper extremity neurovascular symptoms in greater than 97% of patients who presented with neurogenic symptoms in the upper extremity. These observations have led these investigators to propose the ischemic versus the compressive mechanism for Neurogenic TOS. They have likened neurogenic TOS in the upper extremity to the well-known phenomenon of paresthesia, numbness, and pain which results from crossing one leg over the other at the knee. Despite commonly held belief that Crossing Leg syndrome results from compression of the peroneal nerve, it has been shown that in fact it is the result of the compression of the popliteal vein by the contralateral knee.
The present understanding of TOS is that it is the manifestation of a congenital malformation of the first rib. The congenital malformation is in the form of a pronounced tubercle which results in an abnormal costo-clavicular-sternal joint and the compression of the subclavian vein at its junction with the innominate vein. The congenital disease is bilateral with variable symptomatic expression. The compression of the subclavian vein in the thoracic outlet results in a spectrum of disease which ranges from neurologic symptoms resulting from venous ischemia of the upper extremity nerves (Peet’s Neurogenic TOS) to thrombosis of the subclavian vein with prolonged compression (Paget Shroetter or Peet’s Venous TOS). Therefore, patients with neurogenic TOS and venous TOS or PSS represent two manifestation of the same disease process.
Rethinking TOS: Peet’s classification of TOS was based on anatomic rather than symptomatic presentation of the disease. Based on recent studies, in order to decrease confusion and to improve therapeutic results with TOS, the disease should be classified based on the underlying pathologic entity. Acquired and traumatic abnormalities of the clavicle and first rib should be classified separately.
Clearly after the more common and objectively supported diagnoses of conditions that result in neurovascular symptoms of the upper extremity such as cervical spine disease, carpal tunnel disease and nerve entrapment syndromes, have been ruled out, there remains a group of patients who are suspected of having TOS. In these patients rather than the more usual classification such as arterial, venous or neurogenic, the more accurate approach from a diagnostic and therapeutic approach is to classify them as:
- Cervical Rib Disease: In these patients an abnormal cervical rib or the associated bands that insert onto the first rib result in compression and displacement of the nerves or vessels in the neck. These patients can present with neurologic or vascular compromise. Patients with CRS can have complications relating to compression of the subclavian artery and the brachial plexus secondary to a well-formed cervical rib, or to an incompletely formed first rib, fibrous band associated with a rudimentary cervical rib, or a giant transverse process of C. Although in the past, these patients have been classified as TOS, separation of these patients into CRS allows for a more precise diagnostic and therapeutic strategy and perhaps more importantly clears the way to a better understanding of diseases that result from anomalies of the first rib.
- Thoracic Outlet Disease: In these patients an abnormal first rib results in compression of the subclavian vein the subclavian-innominate junction. Compression of the vein results in venous hypertension in the upper extremity and resultant neurologic symptoms. With prolonged compression of the subclavian-innominate junction, the vein clots giving rise to PSS. Therefore, patients who have been previously classified as Neurogenic and Venous TOS represent a variable symptomatic presentation of the same pathologic entity which affects the subclavian vein. The term Arterial TOS should be abandoned as these patients are better classified under Cervical Rib disease or under traumatic causes.
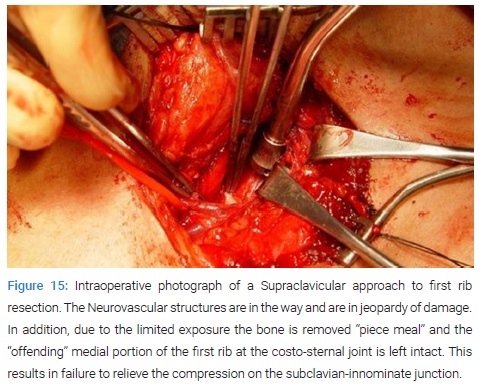
First rib resection: Surgical approaches to resection of the first rib have included transthoracic, transaxillary, supraclavicular, infraclavicular, and thoracoscopy [85–94]. However, these approaches are associated with neurovascular complications, incomplete decompression of the subclavian vein and the medial aspect of the thoracic outlet, and incomplete resection of the most medial portion of the rib. Brachial plexus injury after transaxillary first rib resection has ranged from 0.6%–9%, and 4% after supraclavicular first rib resection [87–89].
These complications are in large part the result of the extrathoracic surgical approach and the difficulty with exposure and access (Figure 15). In addition, the concept has been to remove the body of the first rib and leave the joints at the two ends of the rib intact. This concept has been reinforced by the technical difficulty of disarticulating the costo-sternal joint by a Transthoracic, supraclavicular or VATS approach.
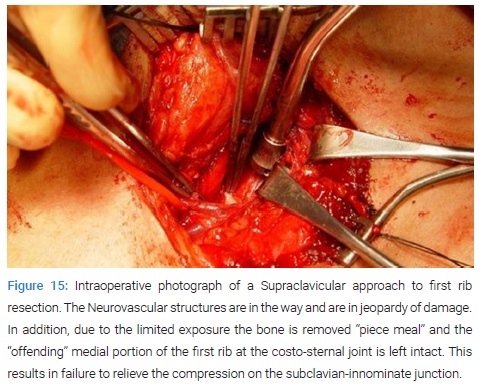
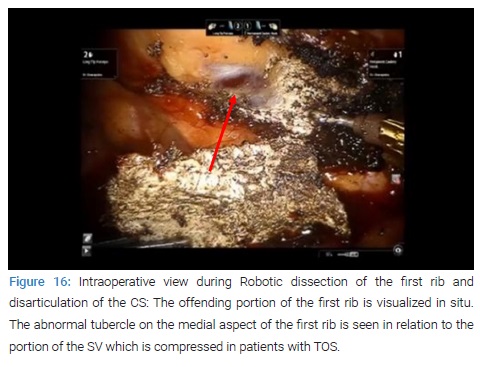
Ironically, based on the present understanding of the offending portion of the first rib which is located at the costosternal joint, transecting the rib at the joint and removal of the rib is ineffective in relieving the extrinsic compression of the subclavian-innominate vein junction. Indeed, this observation may be the explanation for the lack of relief of neurologic symptoms in a significant number of patients with neurogenic TOS, and failure to attain full patency of the subclavian vein in patients with venous TOS. Theoretically, a minimally invasive transthoracic approach aimed at removing the offending compressive portion of the first rib would obviate the neurovascular complications and allow for complete resection of the offending portion of the first rib. The robotic surgical systems have the advantages of 3D high-definition visualization, precise instrument maneuverability in a confined space. Robotic resection of the offending portion of the first rib in patients with TOS has been associated with excellent results. The results have been due to:
- Better understanding of the pathogenesis of TOS, and
- The technical advantages of the robotic platform (Figure 16).
In a recent report Eighty-three patients underwent robotic first rib resection for PSS [74]. There were 49 men and 34 women. Mean age was 24 years ± 8.5 years. Operative time was 127.6 minutes ± 20.8 minutes. Median hospitalization was 4 days. There were no surgical complications, neurovascular injuries, or mortality. At a median follow-up of 24 months, all patients had an open Subclavian Vein (SV) for a patency rate of 100%. Seventy-nine patients underwent robotic first rib resection for neurologic symptoms of the upper extremity (neurogenic TOS). There were 29 men and 50 women. Mean age was 34 years ± 9.5 years. Operative time was 87.6 minutes ± 10.8 minutes. There were no intraoperative complications. Hospital stay ranged from 2 days to 4 days with a median hospitalization of 3 days. There were no neurovascular complications.
There was no mortality. In patients with neurogenic symptoms, QuickDASH Scores (mean ± SEM) decreased from 60.3 ± 2.1 preoperatively to 5 ± 2.3 in the immediate postoperative period, and 3.5 ± 1.1 at 6 months (P < 0.0001). Immediate relief of symptoms was seen in 71/79 (91%) patients. Persistent paresthesia was seen in 9/79 (9%) immediately postop and 3/79 (3.8%) patients at 6 months. Following the appropriate identification of the offending portion of the first rib which results in compression of the SV at its junction with the innominate vein by MRA, robotic resection of the offending portion of the first rib allows is associated with excellent results.