Traumatic Arteriovenous Fistula: A Literature Review
Carvalho Cla;
Silva Ln;
Lima Mbc;
Cavalcante Rcr;
Vasconcelos-Filho Jom;
-
Carvalho Cla: Department of Medical Sciences, University of Pernambuco, Brazil.
-
Silva Ln: Department of Medical Sciences, University of Pernambuco, Brazil.
-
Lima Mbc: Department of Medical Sciences, University of Pernambuco, Brazil.
-
Cavalcante Rcr: Department of Medical Sciences, University of Pernambuco, Brazil.
-
Vasconcelos-Filho Jom: Department of Vascular Surgery, Medical Sciences, University of Pernambuco, Brazil.
-
Dec 28, 2021 |
-
Volume: 2 |
-
Issue: 3 |
-
Views: 7253 |
-
Downloads: 2234 |
Abstract
ArterioVenous Fistulas (AVF) can be described as abnormal communication between the artery and vein. In these situations, blood tends to flow from the highest to the lowest pressure vessel, and it can occur in practically the whole body. Traumatic AVF (TAVF) is present in about 4% of vascular traumas among its etiologies. This work aims to evaluate the main clinical characteristics of TAVF. Forty-five articles published in the last five years were selected as free access, using the headings arteriovenous fistula and wounds and injuries. TAVF was prevalent in men at the mean age of 41.6 years. The primary etiology was a gunshot wound, and the predominant topography was the head. The trauma-diagnosis time interval varied, with most patients being diagnosed after one or more days. The physical examination was the one that suggested AVF the most. The most common findings were notable mass (pulsatile or not), associated with a murmur or thrill, the pain of varying intensity, and edema. The most used test for confirming the diagnosis was conventional angiography. Angio-CT can also be helpful. Considered a rare complication of vascular lesions, TAVF represents a diagnostic and therapeutic problem. The type of injury is often perforating, and the clinic is quite variable and can take from hours to years for diagnosis and definitive treatment. Late complications of TAVF include heart failure, edema, and decreased distal perfusion. Thus, due to its clinically important evolution, attention should be paid to the presence of this complication in patients with a history of trauma.
Abbreviations
AVF: ArterioVenous Fistula; TAVF: Traumatic ArterioVenous Fistula; Angio-CT: Angio-Computerized Tomography; PubMed: U.S. National Library of Medicine; BVS: Biblioteca Virtual de Saúde; SciELO: Scientific Electronic Library Online; CT: Computerized Tomography; MR: Magnetic Resonance; TOF: Time-of-Flight; NBCA-lipiodol: N-Butyl Cyanoacrylate-lipiodol.
Introduction
Arterio Venous fistulas (AVF) can be described as abnormal communication between the artery and vein. In these situations, blood tends to flow from the highest to the lowest pressure vessel, and it can occur in almost every part of the body [1]. This condition can be divided into two main etiologic groups, congenital and acquired, the latter being subdivided into traumatic and iatrogenic. Worldwide AVF of traumatic etiology (TAVF) is not very frequent, usually related to penetrating traumas with different sites, signs, and symptoms [1]. The word trauma is used to describe injuries caused by external forces due to accidents, violence, or self-harm [2]. TAVF represents about 4% of vascular traumas. However, due to the high occurrence of traumas in Brazil, this etiology tends to be more relevant in this country [1,3]. The peripheral vascular resistance, decreased by abnormal blood vessel communication and increased cardiac output, favors heart failure. Thus, the most frequent general presentations are the presence of purplish and engorged veins, similar to varicose veins; decrease in blood pressure; and edema of the lower limbs. However, the manifestations change according to the topography and the etiology of the vascular lesion [4,5,6].
Superficial AVF can develop with erythema, cyanosis and ecchymosis, which can compromise the appearance and machinery murmur and thrills of varying intensity. When it reaches organs such as the brain, it can evolve with headache, convulsions, nausea, and vomiting; in the lungs, cyanosis, digital clubbing, asthenia, and hemoptysis are common; in the gastrointestinal tract, bleeding is the primary manifestation. It is known that the signs and symptoms tend to accentuate over time due to the increased blood flow [2,7,8]. The treatment of TAVF has undergone many changes over time. In the past, the patient was put under observation, and surgical intervention was only performed if necessary. Today, with the advent of the endovascular technique, it was found that the best management consists of interventions performed as early as possible in order to prevent future complications [2].
Therefore, this work aimed at evaluating the overview of the main clinical and epidemiological characteristics of the traumatic arteriovenous fistula. It is also intended to identify and analyze the etiopathogenesis, prognosis, complications, treatment, and rehabilitation of the TAVF.
Materials and Methods
This work can be defined as a literature review. Such projects allow knowledge synthesis by incorporating results from primary studies on the addressed subject, serving as a valuable tool for scientific production in Health Sciences [9].
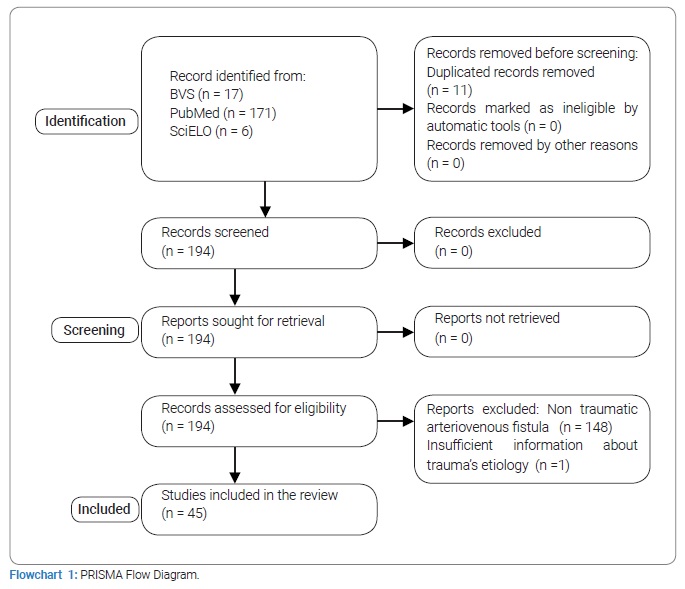
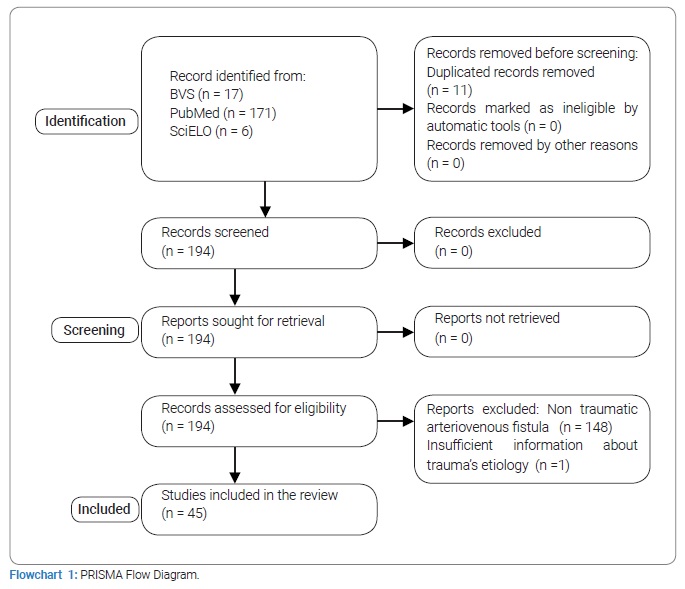
The data was collected using PubMed (U.S National Library of Medicine), BVS (Biblioteca Virtual de Saúde), and SciELO (Scientific Electronic Library Online) databases. The chosen search strategy for research in the databases used “Arteriovenous fistula” and “wounds and injuries” descriptors associated with the Boolean operator and as well as their respective ones in the Portuguese language. Articles about traumatic arteriovenous fistula published in the last five years, in the Portuguese and English languages, were included, in which the complete text was available for free. Articles about fistula with congenital or iatrogenic etiology were excluded from the search. One hundred seventy-one pieces were gathered in the PubMed database, 17 articles in the BVS, and 6 in the SciELO. After reading the abstracts to select the articles that were compatible with the research objective and excluding those that were duplicated, a total of 45 articles were obtained.
Results
In the epidemiology context, articles with full information on age, gender, and country of origin were considered. Socioeconomic aspects were not described in any article. A total of 74 cases were gathered. The masculine gender was predominant (n = 54; 72.97%) in comparison to the female counterpart (n = 20; 27.03%). The age range was 7 years to 87 years, with an average of 41, 62, a variance of 380,95, and a standard deviation of 19,51.
In decreasing order, the study participants came from: Turkey (n = 18), China (n = 13), Taiwan (n = 13), Japan (n = 5), Marrocos (n = 5), Brazil (n = 4), United States (n = 4), India (n = 2). Botswana, Cameroon, South Korea, Spain, Italy, Jordan, Lebanon Mexico, Poland and Switzerland only reported one case each.
Among many case reports described in 45 articles, 84 had information on trauma etiology. In this way, the main TAVF etiology found was gunshot (39.28%), followed by cold weapon and falls the expression and/or contusion with 23.8% each. Vehicle accidents took over 3rd place with 11.9% of the cases, followed by head trauma with only one point.
The TAVF topography, reported in 118 cases, varied significantly, with greater head area incidence (38.9%), mostly related to the carotid-cavernous fistula. The upper limbs occupied the second position with 30.5% of the cases, followed by lower limbs with 11.86%. The abdomen area totalized 7.62% of patients, and 4.23% occurred in the neck. Chest and other regions add up to 3.38% each.
When it comes to blood vessels, the arterial and venous compartments involved in the AVF were specified in 106 and 102 cases, respectively. The most affected arteries were: carotid (46), popliteal (30), femoral (11), subclavian (4), and tibial (3). Other arteries such as mesenteric, pudendal, vertebral, and occipital were less prevalent in 2 cases each. The remaining arterial compartments (10) appeared in only one point each.
The veins affected by AVF varied, with the cavernous sinus (38) as the most prevalent, followed by popliteal (23), femoral (10), and jugular (7). Other venous compartments such as mesenteric, subclavian, and portal veins had less participation, with only 2 cases each. The remaining vessels (12) appeared in only one point each.Regarding the time between the trauma and the development of the arteriovenous fistula, 43 articles that possessed this information available were considered. Most cases (76.7%) took more than one day to develop this vascular complication. The time between trauma and diagnosis varied from confirmation on initial treatment to 25 years later. The average was 860,3 days until diagnosis confirmation, a median of 150 days, with trimodal in 240, 30, and 21 days.
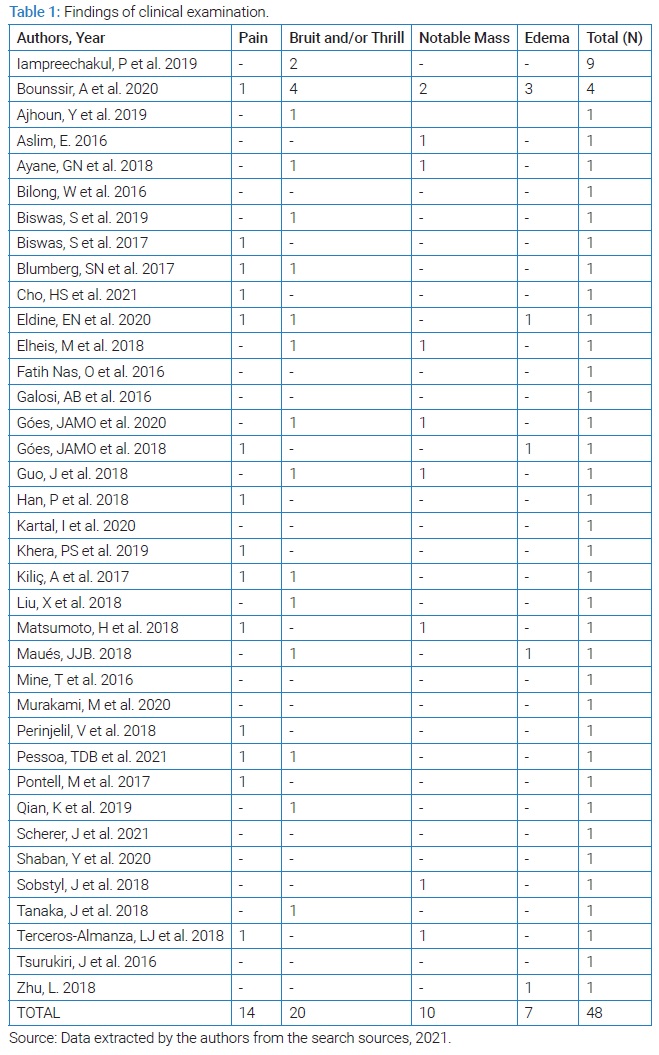
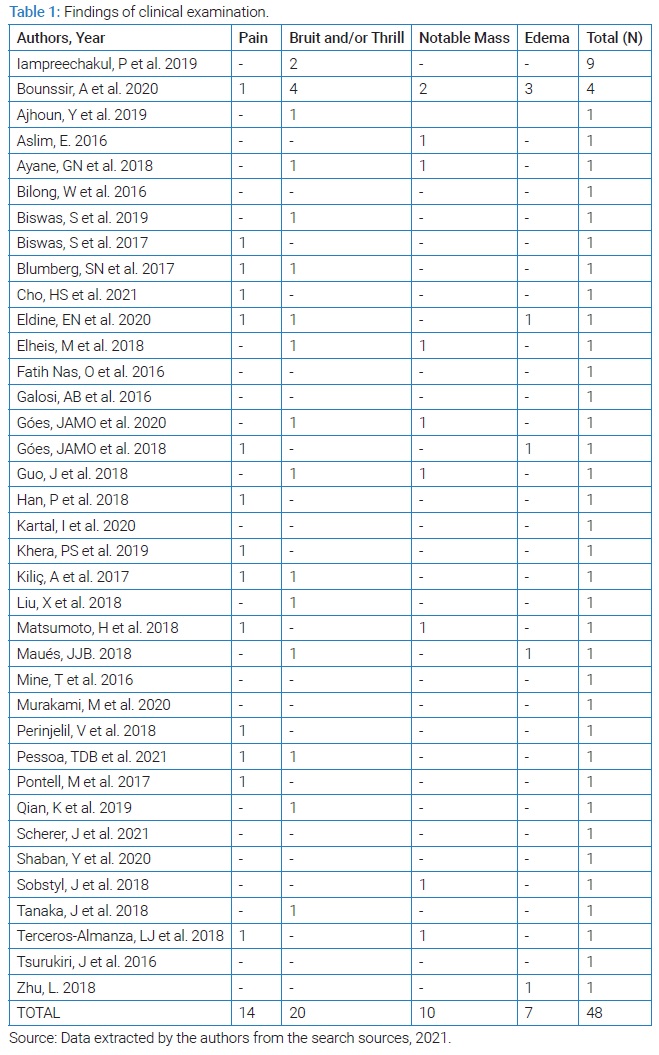
In the selected articles, 48 had entire clinical history described, among which only 5 (10.4%) were discovered in the first moments after trauma and did not develop specific symptoms of the complication. It is essential to observe that 10 (20.8%) had some notable mass on physical exam, pulsatile or not, and this incidence increases to 24 (50%) if we consider other symptoms of local growth/swelling such as proptosis (13 cases) and priapism (1 case).
Despite generally occurring in moderate intensity, the pain was present in 14 (29.1%) reports, and 7 (14.6%) had edema. Other notable signs are bruited or murmurs, present in 11 cases (22.9%), and thrill or tremor, in 7 cases (14.6%). Other less prevalent findings include hyperemia, bleeding, hematoma, hepatomegaly, and ocher dermatitis. The summary of those findings is described in (Table 1).
Physical exam was what suggested AVF the most, being responsible for the rise of the hypothesis in 49 (80.3%) of the 61 cases that defined which exam was used primarily for the investigation. Computed tomography (CT) with or without contrast came in next with 12 points (19.7%), followed by Doppler ultrasound in 8 (13.1%). In 6 cases, the correlation of two exams indicated the possibility of the fistula.
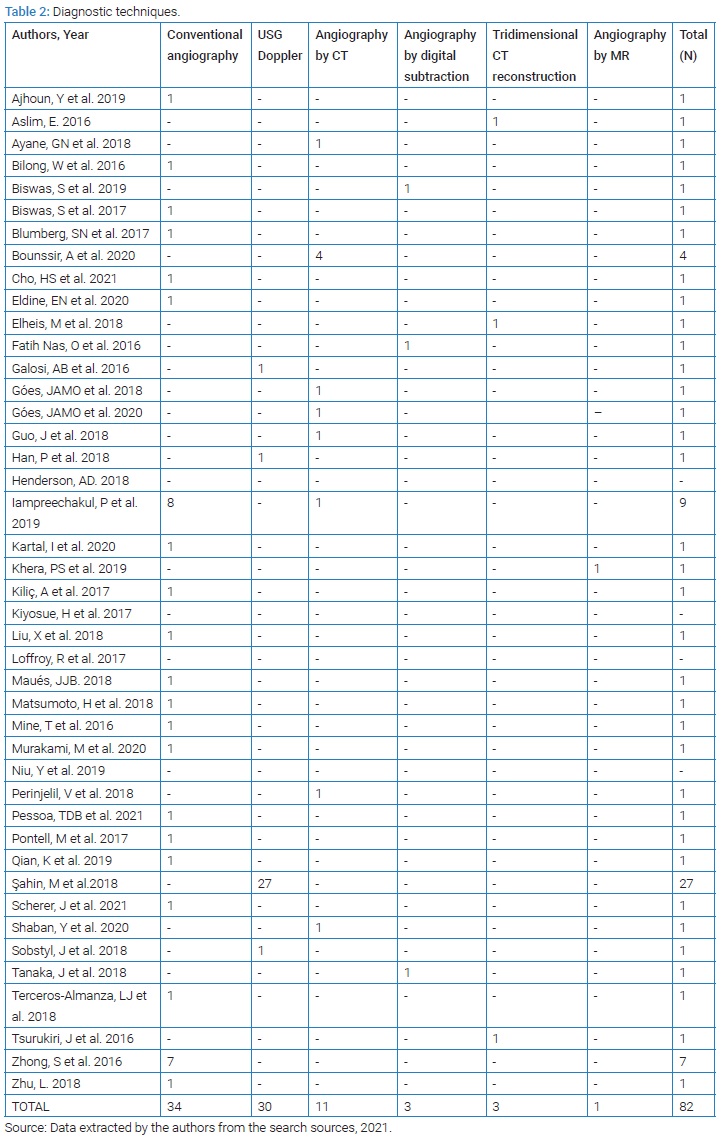
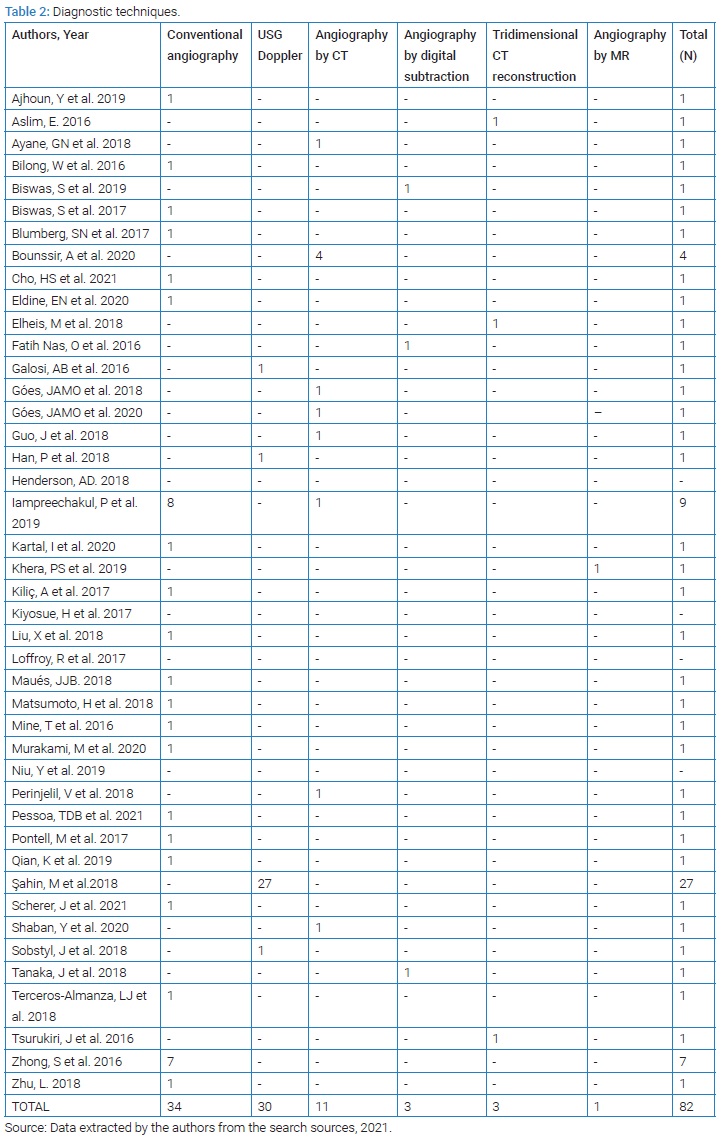
82 cases defined which exam confirmed the fistula. The most used method to establish diagnosis was conventional angiography, reported in 34 patients (41.4%). Doppler ultrasound and angiography by CT were used in 30 (36.6%) and 11 (13.4%), respectively. Angiography by digital subtraction and tridimensional CT vessel reconstruction was presented in 3 cases (3.6%) each. Angiography by MR was sufficient to confirm the diagnosis in one case (0.1%). All of these findings of diagnostics methods can be found in (Table 2).
Eighty cases described the presence/absence of associated injuries, which were present in 46 (57.5%). Regional fracture (30%) and pseudoaneurysm (21.25%) were predominant among these.
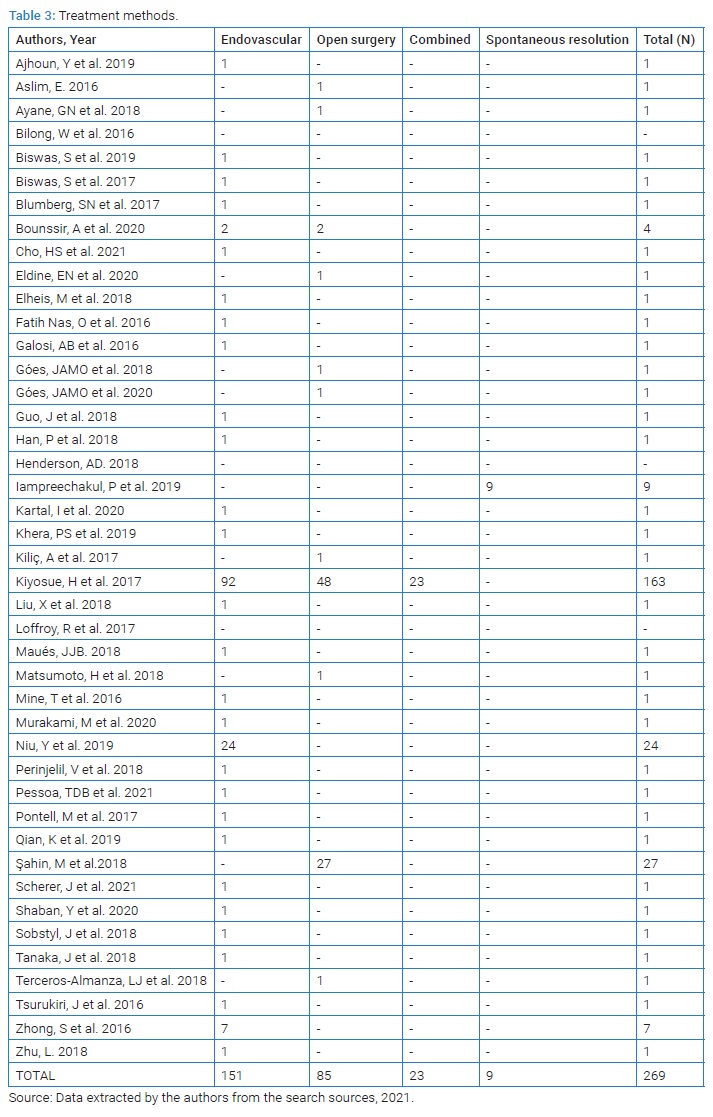
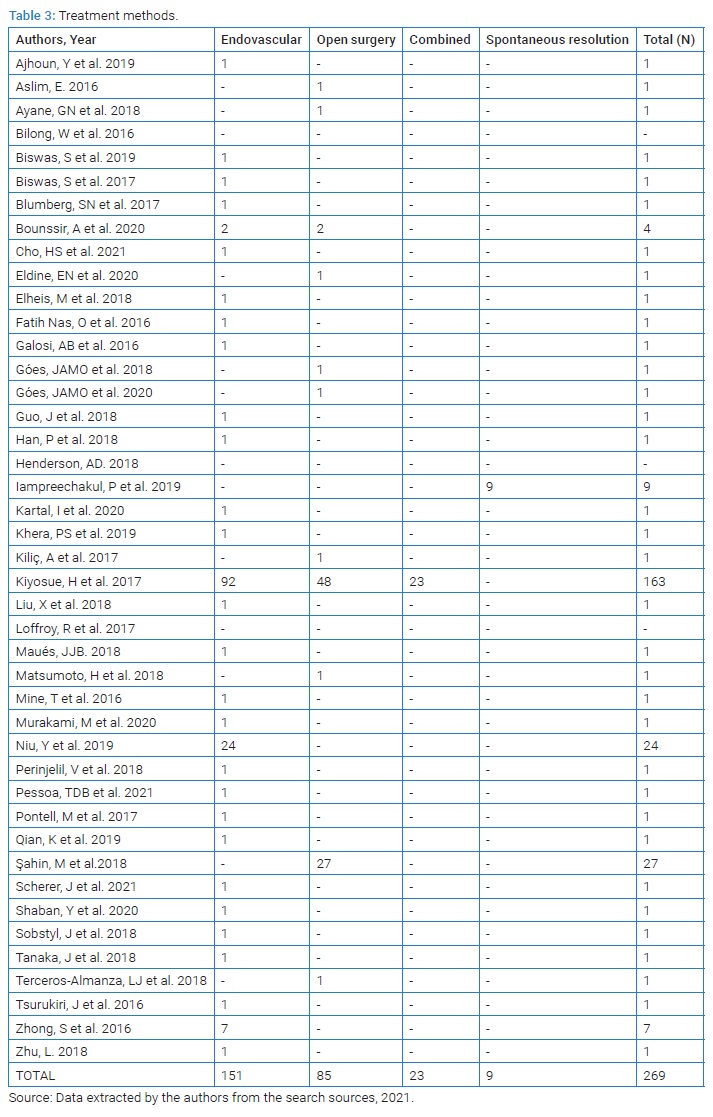
Considering all mentioned patients in the articles (n = 269), the most used method was endovascular surgery, representing a total of 151 cases (56.1%), while open surgery was the treatment choice in 85 cases (31.5%). Twenty-three patients (8.6%) combined with open and endovascular surgery. Although it is essential to notice that one point had merely a clinical follow-up and that 9 had spontaneous resolutions, meaning that 10 (3.7%) didn’t need surgical treatment. In one case, there were no treatment measures specified.
Eighteen cases (6.3%) required a new intervention, mainly related to thrombi occurrence (n = 3; 16.6%) and new TAVF or pseudoaneurysm treatment (n = 9; 50%), considering those that had escaped notice and recurrences. Other reasons for new intervention included treatments of complications and other arterial injuries, with a minority (n = 4; 22.2%) ending up with the need of open surgery as an additional treatment (Table 3) summarizes these results.
Discussion
Firstly described by William Hunter in 1761, arteriovenous fistulas are capable of causing variable vascular damage, with their severity associated with the mechanism and location of the trauma. They are a rare complication of vascular injuries and may represent grand diagnostic and management challenges [10].
In Brazil, external causes are the leading causes of death in the age group from 1 to 39 years, with a mortality rate of 70,5 cases per 100 thousand inhabitants, and males representing 83.1% of all deaths [11]. A study that occurred from 2013 to 2014 in a great hospital center in the state of Rio de Janeiro also highlighted the trauma predominance in male patients, representing 82% of 1268 attended, in which 59.7% were in the age group from 15 years to 39 years [12]. Although the average age and gender prevalence are close to the ones obtained in the literature review, it is not possible to say that the TAVF follows that tendency since the epidemiological data about the injury are scarce both nationally and internationally.
The literature has shown two theories for AVF formation, the theory of laceration and the theory of rupture. The first one occurs when simultaneous cuts of an artery and its corresponding vein generate a communication channel, the fistula. The other would be when the injury resulting from the trauma induces some artery wall rupture, especially in the vasa vasorum; thereafter, endothelial cells proliferate, forming numerous small vessels and leading to an AVF [13].
The injury mechanism is often penetrating, with most cases being caused by cold weapons followed by projectiles or firearms [14]. Firearm and cold weapon injuries were the most prevalent in the current study.
In a review of 210 TAVF, it was observed that more than 50% of them were located in the cervical-mediastinal vessels, 22% in the upper limbs, and 20% in the lower limbs [14,15]. This topographical prevalence presented variation in other studies that show the periphery as more prevalent, including the arteries and veins of the neck, upper and lower limbs [16,17,18] and the cervical-mediastinal region, upper limb, chest, abdomen, and lower limbs [19]. Such characteristics were noted in the sample of this study, in which it prevailed in the head region, followed by lower limbs and upper limbs.
The clinical evolution of AVF is variable and can take from hours to years until diagnosis and definitive treatment are performed [20,21,22]. Still, there is a relatively high possibility (15%) that no apparent sign or symptom will occur. It is interesting to note that, according to the literature, pulsatile masses are present in 20% of the cases, and murmurs reach 60% [23]. The first data is befitting with the findings of this review (20.8%). Otherwise, the prevalence of drones was almost three times lower.
TAVF is, in itself, a complication of a vascular trauma in which, if there is no early identification, it can progress with continuous dilatation of the problematic veins, generating pulsatile venous and lymphatic complications [20,24]. More worryingly, there are later complications such as heart failure, edema, and decreased perfusion due to the steal phenomenon [25].
This is why, when the occurrence in the extremities is analyzed, edema, pain, and murmur can be found, but it is also essential to pay attention to changes in the distal pulse [14,26,27]. In events where a perforation causes the TAVF due to a projectile, in addition to cavitation, it can progress with inflammation and angiogenesis, which delays the resolution of the fistula [25,28]. Thus, one of the principles of the fistula’s treatment, as in the popliteal region, is to avoid prolonging ischemia [29].
AVF that results in mesenteric congestion can cause severe diarrhea [30,31]. However, pain seems to be the most prevalent symptom in the reports involving the abdominal area [32]. When there is the involvement of the aortic artery and vena cava, lower limb edema (> 50%) or critical congestive symptoms are common, therefore being more severe [33]. The portal and pulmonary hypertension development end up being demonstrated with dyspnea, hepatomegaly, and abdominal/thoracic murmurs [34,35]. As for the male reproductive system, initially, non-specific symptoms are present, such as post-traumatic urethral bleeding up to priapism [36,37].
In the head and neck region, murmurs can become audible, turning into complaints of drones or tinnitus. The increase in local volume can be accompanied by pulsatility or become a signal like proptosis [38,39,40]. However, the most problematic fact is the possibility of neurological and visual changes such as strabismus (due to changes in the abducens or oculomotor nerve), headache, visible deterioration, diplopia, and even syncope [28,41,42].
In almost all cases, the clinical history and the physical exam are sufficient to diagnose a traumatic AVF. There were 23 patients in whom the physical exam suggested the condition in this research, but in only one it was enough to diagnose it. The imaging exam is essential to precisely locate the AVF, identify the injured blood vessels, do a hemodynamic analysis and establish a treatment plan. Angiography is considered the most precise diagnostic technique [43]. However, the method can vary greatly according to the possible AVF´s type and location.
CT angiography is seen as the main image exam in cases of vascular injuries involving multiple organs as it has increased its sensibility and specificity from 15.4% to 93% with the advancement of techniques such as CT multidetector [44,45]. Doppler ultrasound is preferred in stable patients with limited vascular injuries [23].
Some studies acknowledge the ultrasound as the primary method of diagnosis for being cheaper, less invasive, and less associated with complications. The disadvantages of the ultrasound are related to its limited use in cases of primary and open injuries and being dependent on the operator´s ability [23]. Other sources claim the angiography as the gold standard to confirm the existence of an AVF for allowing a better localization and visualization of the injury [16]. Furthermore, angiography is considered necessary to develop a surgical plan, be it endovascular or open procedure [13,46]. In this research, the most commonly utilized methods were conventional angiography, followed by CT angiography and digital subtraction angiography. The ultrasound came in fourth place, but it is essential to highlight that it has suggested the AVF in 8 cases. The use of MR angiography is much more common in cases of AVF in the skull. Its usage has been rising due to the significant increase in quality with the advance of the TOF technique. This change caused the sensibility and specificity to jump from 50% to 93% [44].
The interval time between the trauma and the diagnosis range between 10 days and 33 years [47]. In the 48 cases that had the complete clinical history described, we can find an interval extending from 3 days to 25 years, consistent with the literature.
A study in a surgical center indicated that endovascular treatment was the most common approach and that only a minority of patients required a new intervention [48]. This affirmation was confirmed by this research, in which the endovascular methods were the first choices in over half of the cases, and the incidence of new interventions was only 6.3%. The selection of the treatment technique must take into account anatomical characteristics, size, degree and alteration of the arterial flow, and the condition of monitoring of the patients. In situations of anatomical distortion, such as in great AVFs or those associated with pseudoaneurysms, endovascular techniques exhibit superiority compared to the surgical dissection of the compromised structures [49,50].
With a morbimortality that ranges between 5 and 10%, the emergence of the endovascular approach was a revolution [51]. The treatment through this method may include techniques such as embolization using coil and glue (like NBCA-lipiodol), detachable balloon as well as a venous endoprosthesis for the exclusion of the AVF. Different techniques can also be combined for a better procedure outcome [1,52].
It is essential to highlight that those techniques are contraindicated in significant injuries, the absence of the proximal neck of the femur for fixation, and the discrepancy between the proximal and distal diameters of the blood vessels. Other situations may include the impossibility of catheterization of vessels, injuries that need exploratory surgery, hematoma with compressive symptoms, and infected wounds [51].
The most common technical complication that hindered the intravenous approach was the impossibility of advancing the guidewire. Still, hemodynamic instability was also an essential reason for the indication of open surgery [43]. Other possible complications that may justify a change in the method are persistent blood flow and prosthesis migration [1].
Open surgery consists of performing ligatures, grafts, anastomosis, sutures, and patches to complete vascular repair. Such methods can be chosen and even combined according to the patient´s case. Ligation should be avoided because it is associated with worse outcomes of arterial reconstruction [49].
Finally, it is also possible to combine endovascular and open surgery, as recorded in 23 of the cases described in this research. A patient with a simple clinical condition can be treated with a single therapeutic method, but combined may be required in cases of extensive and complicated fistulas [15].
Final Considerations
TAVF is an uncommon condition, and it can have a clinically significant evolution. Thus it is necessary to search for this complication in patients with a traumatic history or victim of traumas since the majority of the cases had a penetrating etiology. To the detriment of more complex exams, the physical exam seems the most appropriate way to raise hypotheses about this condition. Conventional angiography serves as the standard gold method for diagnosing the fistula. Its preferred treatment is the endovascular approach, in which several different techniques can be used, but surgical treatment can still be necessary, especially in cases with hemodynamic instability and pervasive injuries.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Eldine EN, Dehaini H, Hoballah JJ, Haddad FF. Management of dual traumatic arterial-venous fistula from a single shotgun injury: a case report and literature review. BMC Surgery. 2020;20(1):177.
- Valparaiso AP, Vicente DA, Bograd BA, Elster EA, Davis TA. Modeling acute traumatic injury. J Surg Res.2015;194(1):220–232.
- Rasmussen TE, Tai NRM, organizators. Rich´s vascular trauma. 3. ed. Philadelphia: Elsevier; 2016. 354 p.
- Zyck S, Jesus OD, Gould GC. Dural Arteriovenous Fistula. 2021;7(14):20–22.
- Murakami M, Maruyama D, Fujiwara G, Komaru Y, Murakami N, Iiduka R, et al. Early treatment of progressive vertebral arteriovenous fistula caused by cervical penetrating injury. Acute Med Surg. 2019;7(1):e467.
- Kartal İ, Durmaz HA, Çimen SG, Çimen S, Ersoy H. Transcatheter embolization in pediatric blunt renal trauma: Case report and review of the literature. Ulus Travma Acil Cerrahi Derg. 2020;26(3):475–481.
- Al-Jaish AA, Liu AR, Lok CE, Zhang JC, Moist LM. Complications of the Arteriovenous Fistula: A Systematic Review. J Am Soc Nephrol. 2017;28(6):1839–1850.
- Padberg FT, Calligaro KD, Sidawy AN. Complications of arteriovenous hemodialysis access: Recognition and management. J Vasc Surg. 2008;48(5 Suppl):55S–80S.
- De-la-Torre-Ugarte-Guanilo MC, Takahashi RF, Bertolozzi MR. Systematic review: general notions. Rev esc USP. 2011;45(5):1260–1266.
- Robbs JV, Carrim AA, Kadwa AM, Mars M. Traumatic arteriovenous fistula: Experience with 202 patients. Br J Surg.1994;81(9):1296–1299.
- Brazil. Ministry of Health. National Health Plan. 2021;16: 2012–2015.
- Silveira ES, O’Dwyer G. Trauma Center: alternative model of care for external causes in the state of Rio de Janeiro. Saúde debate. 2017;41(112):243–254.
- Matsumoto H, Yamaura I, Yoshida Y. Identity of growing pulsatile mass lesion of the scalp after blunt head injury: Case reports and literature review. Trauma Case Rep. 2018;17:43–47.
- Shaban Y, Elkbuli A, McKenney M, Boneva D. Traumatic femoral arteriovenous fistula following gunshot injury: Case report and review of literature. Ann Med Surg (Lond). 2020;55:223–226.
- Guo J, Zhan R, Ren Y, Meng X, Liu R, Li G, et al. The Hybrid Technical Management of Large and Complicated Traumatic Arteriovenous Fistula of Preauricular Region. J Craniofac Surg. 2018;29(2):432–436.
- Biswas S, Hristov B. Endovascular Management of a Penetrating Zone III Retroperitoneal Gunshot Wound Injury; A Case Report. Bull Emerg Trauma. 2017;5(4):303–306.
- Perinjelil V, Maraqa T, Yenter AC, Ohaeri H, Mercer L, Bansal A, et al. Traumatic arteriovenous fistula formation secondary to crush injury. J Surg Case Rep. 2018:2018(9):rjy240.
- Scherer J, Schäfer FP, Kobe AR, Messmer F, Pape HC, Rauer T, et al. Ordinary injury, big surprise - Traumatic false aneurysm and arteriovenous fistula of the posterior tibial artery after civilian trauma: A case report. Trauma Case Rep. 2021;32:100432.
- Chang HM, Chou YC, Jou IM, Yang JM, Ma CH, Wu PT, et al. Clinical outcomes in distal radial fractures with ipsilateral arteriovenous fistulas. J Orthop Surg Res. 2019;14(1):143.
- Cho HS, Kim Y, Lee J, Yi KS, Choi CH. Use of N-butyl cyanoacrylate in the successful transcatheter arterial embolization of an arteriovenous fistula caused by blunt pelvic fracture: A case report and review of literature. Medicine (Baltimore). 2021;100(1):e24215.
- Bilong W, Ngoune CN. Post traumatic, indirect carotid cavernous fistula: indirect diagnosis in limited context. Pan Afr Med J. 2016;24:72.
- Terceros-Almanza LJ, Domínguez-Aguado H, Pizarro-Rodríguez F. Traumatic arteriovenous fistula of the vertebral artery. Med Intensiva (Engl Ed). 2018;42(6):e15.
- Sobstyl J, Kuczyńska M, Kuklik E, Światłowski Ł, Tsitskari M, Jargiełło T, et al. Diagnosis and treatment of posttraumatic arteriovenous fistula in the lower leg – a case report. J Ultrason. 2018;18(73):166–159.
- Aslim E. Traumatic Arteriovenous Fistulae 25 Years After Gunshot Injury. Eur J Vasc Endovasc Surg. 2016;52(3):316.
- Pessoa TDB, Araujo WJB, Caron FC, Ruggeri VGM, Erzinger FL, Brandão ABF, et al. Endovascular treatment of subclavian artery injury with a complex post-traumatic fistula: Case report. Trauma Case Rep. 2021;32:100400.
- Góes JAMO, Oliveira CP, Maia CC, Xavier BC, Azevedo SKBC. Surgical correction of pseudoaneurysms and complex arteriovenous fistula between popliteal vessels. J Vasco Bras. 2018;17(3):229–233.
- Ayane GN, Walsh G, Prozesky D, Kadimo K. Simultaneous false aneurysm and arterio-venous fistula in the presence of a single wound. Trauma Case Rep. 2018;16:8–11.
- Iampreechakul P, Tirakotai W, Tanpun A, Wattanasen Y, Lertbusayanukul P, Siriwimonmas S, et al. Spontaneous resolution of direct carotid-cavernous fistulas: case series and literature review. Interv Neuroradiol. 2019;25(1):71–89.
- Zhong S, Zhang X, Chen Z, Dong P, Sun Y, Zhu W, et al. Endovascular Repair of Blunt Popliteal Arterial Injuries. Korean J Radiol. 2016;17(5):789–796.
- Tsurukiri J, Sano H, Akira H, Kaneko N. Early post-traumatic splenic arteriovenous fistula in the pancreatic arcade: Diagnosis by volume-rendered 3D reconstruction images. Ulus Travma Acil Cerrahi Derg. 2016;22(5):495–497.
- Han P, Yang L, Huang XW, Zhu XQ, Chen L, Wang N, et al. A traumatic hepatic artery pseudoaneurysm and arterioportal fistula, with severe diarrhea as the first symptom: A case report and review of the literature. Medicine (Baltimore). 2018;97(7):e9893.
- Kılıç A, Yarlıoğlueş M, Ergün E, Ünal Y, Murat SN. Percutaneous treatment of a superior mesenteric artery pseudoaneurysm and arteriovenous fistula with coil embolization: a case report. Turk Kardiyol Dern Ars. 2017;45(6):556–559.
- Blumberg SN, Mussa FF, Maldonado TS. Percutaneous fenestrated endovascular aortic graft treatment of aortocaval fistula with aortic pseudoaneurysms secondary to penetrating trauma. J Vasc Surg. 2017;66(3):906–909.
- Pontell M, Scantling D, Babcock J, Trebelev A, Nunez A. Lateral Thoracic Artery Pseudoaneurysm as a Result of Penetrating Chest Trauma. J Radiol Case Rep. 2017;11(1):14–19.
- Qian K, Yang N, Lin C, Wan H, Fu F, Liu Z, et al. Portopulmonary Hypertension: A Complex Case Derived from Multiple Penetrating Trauma-Induced Mesenteric Arteriovenous Fistulae. Ann Vasc Surg. 2019;58:378.e11-378.e15.
- Galosi AB, Capretti C, Leone L, Tiroli M, Cantoro D, Polito M, et al. Pseudoaneurysm with arteriovenous fistula of the prostate after pelvic trauma: Ultrasound imaging. Arch Ital Urol Androl. 2016;88(4):317–319.
- Khera PS, Garg PK, Pandey H, Chaurasia K. Post-traumatic high-flow priapism: uncommon presentation with endovascular management. BMJ Case Rep. 2019;12(10):e229299.
- Ajhoun Y, Khoyali AE, Aissa I, Laaribi N, Mouzari Y, Reda K, et al. Direct carotid-cavernous fistula: an atypical presentation. Pan Afr Med J. 2019;34:204.
- Biswas S, Kathrani NV, Jitender S, Gupta AK. XCalibur aneurysm occlusion device for the treatment of direct carotid cavernous fistula: expansion of armamentarium. BMJ Case Rep. 2019;12(2):e014475.
- Liu X, Fan L, Ying C, Cheng Y, Wang M. Traumatic extracranial internal carotid-jugular fistula leading to serious injury: a case report in forensic assessment. Forensic Sci Res. 2018;5(2):170–173.
- Zhu L, Liu B, Zhong L. Post-traumatic right carotid-cavernous fistula resulting in symptoms in the contralateral eye: a case report and literature review. BMC Ophthamol. 2018;18(1):183.
- Jozef Č. Carotid-cavernous fistula from the perspective of an ophthalmologist A Review. Cesk Slov Oftalmol. 2020;1(1):1–8.
- Şahin M, Yücel C, Kanber EM, Mert FTİ, Bıçakhan B. Management of traumatic arteriovenous fistulas: A tertiary academic center experience. Ulus Travma Acil Cerrahi Derg. 2018;24(3):234–238.
- Tanaka J, Fujita A, Ishii T, Kohmura E. Importance of source images of time-of-flight magnetic resonance angiography in the diagnosis of low-flow dural arteriovenous fistulae after traumatic brain injury. BMJ Case Rep. 2018;2018:bcr2017223512.
- Elheis M, Aljarrah Q, Heis H, Haque A. Endovascular Management of an Acquired Carotid-Jugular Fistula in a Child. Am J Case Rep. 2018;19:839–843.
- Kiyosue H, Matsumaru Y, Niimi Y, Takai K, Ishiguro T, Hiramatsu M, et al. Angiographic and Clinical Characteristics of Thoracolumbar Spinal Epidural and Dural Arteriovenous Fistulas. Stroke. 2017;42(12):3215–3222.
- Bounssir A, Taghi H, Sedki N, Bakkali T, Lekehal B. Technical management of traumatic arteriovenous fistula: Tips and tricks. International Journal of Surgery Case Reports. 2020;76(1):468–473.
- Niu Y, Chen T, Tang J, Jiang ZY, Zhu G, Chen Z, et al. Detachable balloon embolization as the preferred treatment option for traumatic carotid-cavernous sinus fistula?. Interv Neuroradiol. 2020;26(1):90–98.
- Góes JAMO, Jeha NSAH, Dias DV, Ferreira JMT. Surgical repair of a traumatic carotid-jugular arteriovenous fistula. J Vasc Bras. 2020;19:e20200008.
- Nas OF, Buyukkaya R, Kacar E, Erdogan C, Hakyemez B. Use of SolitaireTM retrievable stent-assisted coiling technique for endovascular treatment of post-traumatic direct carotid cavernous fistula. Diagn Interv Imaging. 2016;97(11):1193–1195.
- Maués JJB, Hauter HL. Endovascular treatment of traumatic fistula of subclavian vessels: case report. J Vasc Bras. 2018;17(3):248–251.
- Mine T, Murata S, Yasui D, Yokota H, Tajima H, Kumita S, et al. Glue embolization of a blunt traumatic hepatic arteriovenous fistula under inflow and outflow control. J Nippon Med Sch. 2016;83(1):27–30.
Keywords
Arteriovenous fistula; Wounds; Injuries
Cite this article
Carvalho Cla, Silva Ln, Lima Mbc, Cavalcante Rcr, Vasconcelos-Filho Jom. Traumatic arteriovenous fistula: a literature review. Clin Surg J. 2021;2(3):1–10.
Copyright
© 2021 Vasconcelos-Filho Jom. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).