Optimization and Management of Personal Protective Equipment (PPE) in A COVID-19 Positive Field Hospital
Elyse A. Lynch;
Matthew M. Hutter;
Brendan McCaffrey;
Patrick Curley;
Joyce Donadio;
Laura Lakin;
Cliff Brown;
Jeannette Ives Erickson RN;
Ron Hirschberg;
Giles Boland;
* Richard J. Ehrlichman;
-
Elyse A. Lynch: Department of Surgery, Home Base, A Massachusetts General Hospital and Red Sox Foundation Program, United States; Department of Surgery, Brigham and Women’s Hospital, United States.
-
Matthew M. Hutter: Department of General Plastic Surgery, Massachusetts General Hospital, United States.
-
Brendan McCaffrey: Department of Surgery, Home Base, A Massachusetts General Hospital and Red Sox Foundation Program, United States.
-
Patrick Curley: Department of Surgery, Brigham and Women’s Hospital, United States.
-
Joyce Donadio: Department of Surgery, Home Base, A Massachusetts General Hospital and Red Sox Foundation Program, United States.
-
Laura Lakin: Department of Surgery, Home Base, A Massachusetts General Hospital and Red Sox Foundation Program, United States.
-
Cliff Brown: Department of Surgery, Home Base, A Massachusetts General Hospital and Red Sox Foundation Program, United States.
-
Jeannette Ives Erickson RN: Department of General Plastic Surgery, Massachusetts General Hospital, United States.
-
Ron Hirschberg: Department of Surgery, Home Base, A Massachusetts General Hospital and Red Sox Foundation Program, United States; Department of Surgery, Spaulding Rehabilitation Network, United States.
-
Giles Boland: Department of Surgery, Brigham and Women’s Hospital, United States.
-
* Richard J. Ehrlichman: Department of General Plastic Surgery, Massachusetts General Hospital, United States.
-
Dec 03, 2021 |
-
Volume: 2 |
-
Issue: 3 |
-
Views: 2410 |
-
Downloads: 1513 |
Abstract
Importance: The global COVID-19 pandemic has severely stressed the system supplying Personal Protective Equipment (PPE) to healthcare professionals. Healthcare professionals have become fearful of not meeting standards established to protect patients and team members. Critical shortages, especially in N95 masks, have resulted in leaders struggling with local, state, and federal agencies and vendors to secure adequate supplies.
Objective: This paper documents the adaptation of one subacute Alternative Care Facility to restore and preserve system integrity in maintaining PPE supply.
Design: This descriptive study utilizes quantitative PPE supply statistics to inform the efficacy of a novel system for distributing, tracking, and replenishing PPE over an approximately 2 month period between April 2020 and June 2020.
Setting: This study data was collected at Boston Hope, a subacute treatment facility and Field Hospital established by Massachusetts, Boston, and several Boston teaching hospitals.
Interventions: These consisted of establishing PPE requirements, assembling a conservation task force, creating centralized donning and doffing stations, monitoring usage of PPE, implementing gown alternatives, and decontamination and reuse of N95 masks.
Main Outcome and Measure: Our primary outcome was the widespread use of surgical gowns and N95 respiratory masks over the study period.
Results: The Field Hospital remained operational for 54 days and successfully discharged 723 patients. During this time, system integrity was maintained, and the conservation interventions resulted in an uninterrupted supply of PPE. Our efforts resulted in > 59% cumulative reduction in the use of surgical gowns and N95 respiratory masks.
Conclusions and Relevance: This system is easily transferable to other facilities and appropriate for other potential future pandemics.
Introduction
Donning complete Personal Protective Equipment (PPE) is required among healthcare workers to reduce the likelihood of transmission of infectious diseases. These include SARS-CoV-2, the causative agent of the coronavirus disease, which spreads mainly through respiratory droplets produced when an infected person coughs or sneezes [1]. Since the coronavirus outbreak, health care systems around the world have been faced with unprecedented challenges, including managing the skyrocketing demand for PPE and resulting shortage of N95 respirator masks, gowns, and gloves [2]. This has necessitated the need for improvisation, commonly with loss of integrity and improper use of PPE, resulting in an increased risk of infection. Thus, the need for established protocol and continued education efforts surrounding proper management and optimization of PPE is pertinent in the face of this pandemic and possible future ones [3].
The Commonwealth of Massachusetts and the City of Boston, in collaboration with Mass General Brigham (Brigham and Women’s Hospital, Massachusetts General Hospital and Spaulding Rehabilitation Center, formerly Partners Healthcare), were tasked with the establishment of a 1000 bed subacute care facility; Boston Hope (BH) Field Hospital, in anticipation of the surge of COVID-19 positive patients. Given the projected surge, the facility would help ease the burden on local hospitals so that they may provide acute, subacute, and intensive care to those patients in need. This collaborative resource served the Eastern Massachusetts population. Patients admitted it required acute, sub-acute, and isolation convalescing. Boston Hope consisted of two components: A Post-Acute Medical Facility (“Field Hospital”) for 500 COVID-19 positive patients), and a Low-Acute Housing Facility of 500 beds for COVID-19 positive unhoused people of Greater Boston. Given the nationwide shortages of PPE and its crucial role in ensuring the safety of our frontline workers, developing a system of monitoring and preservation of equipment became imperative. During the initial phase of operations at BH, a severe shortage of PPE was experienced, at which point a team was tasked with formulating strategies for the preservation of PPE. Specifically, our supply chain and safety team leaders worked to sustain or restore system integrity during confusion or periodic setbacks. This report describes the system developed and actions taken and analyzes the resulting impact on PPE conservation in a COVID-19 positive Field Hospital.
Materials and Methods
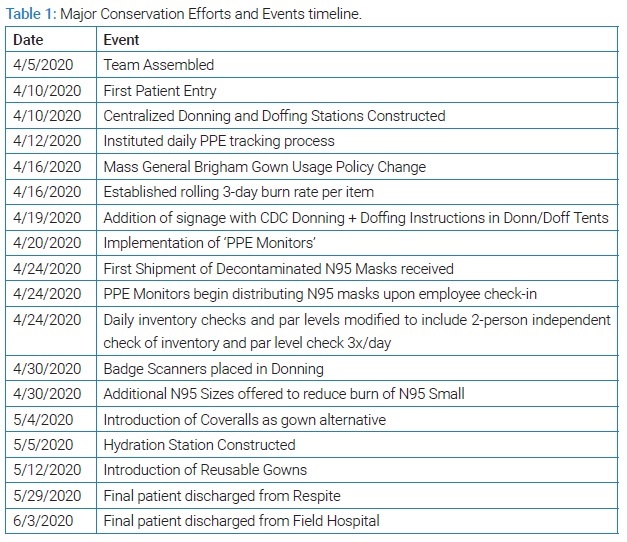
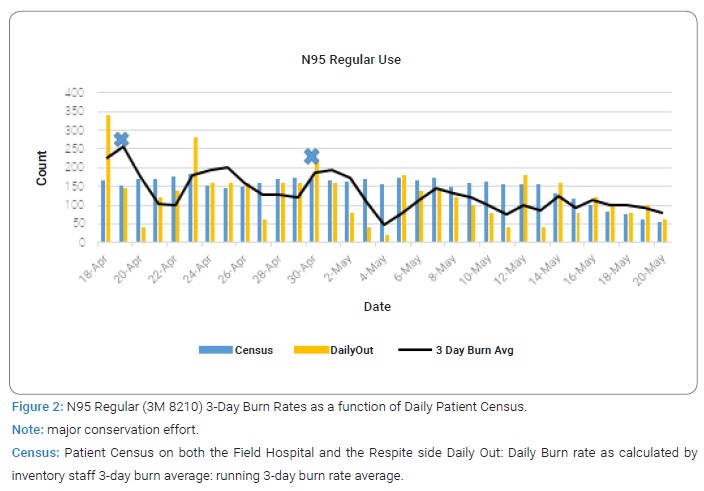
PPE components: The following PPE is included for the purposes of this report: N95 respirator masks and Gowns/coveralls (Table 1).
Event Background and Description Team Assembled: Consistent with prior research [4]. A PPE Conservation task force was assembled, including leadership amongst various departments and between all sites (Boston Hope leaders, the state, Mass General Brigham, Boston Medical Center, BI/Lahey, and the Military Task Force). During the initial opening phase, numerous actions were put into place to ensure the active monitoring of PPE Supply and ensure timely responses to projected shortages. These included, but were not limited to: standing discussion of PPE issues at 9 AM and 5 PM daily meetings; the willingness of the state, hospitals, and local donors to pitch in resources where they could; and rapid assessment by infection control specialists of these products to ensure they met Partners’ standards; subsequent immediate cycle quality/process improvement as to new product processes, training, and rollout.
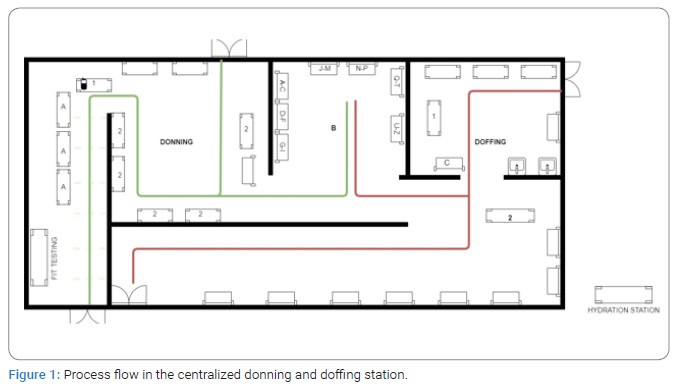
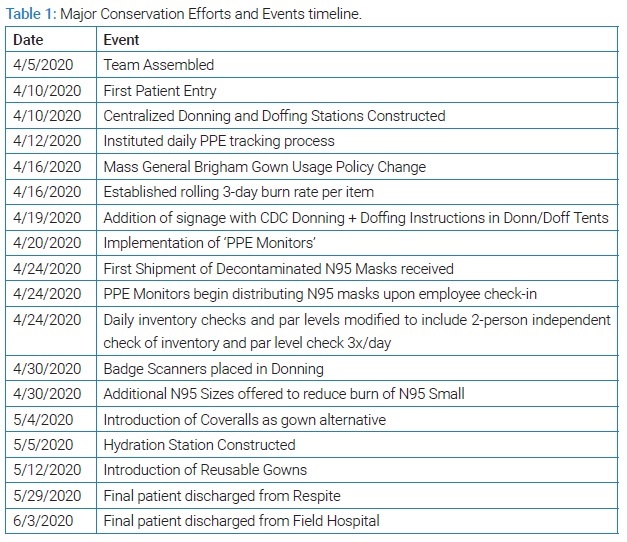
Centralized Donning and Doffing Station: The layout of our field hospital regarding the entrance and exit of staff and the fact that we treated only COVID-positive patients meant we could have one centralized donning and doffing station. While PPE was available on our patient floor for tears or spoilage, or non-COVID infections precautions, all other PPE was available at one location. (Please see the associated diagram). This centralized donning and doffing station ensured the following key functions were performed:
- a) PPE monitors to provide real-time education and assistance at both the donning and doffing locations.
- b) Refitting N-95s in real-time as the new product became available.
- c) Stocking product and assuring appropriate usage with no deficiencies.
- d) Monitoring reuse and reprocessing efforts.
See (Figure 1) for an overview of the process flow in the donning and doffing station.
Donning Workflow (green line)
- a) PPE Monitor checks employee in, checks the size of N95 Mask employee was fit tested to and distributes new or reprocessed Mask (if present; Area A).
- b) Employee dons PPE with assistance from PPE Monitor. Face Shield is retrieved from the bag in Area B (organized alphabetically).
Doffing Workflow (red line)
- a) PPE Monitors oversee doffing of PPE.
- b) PPE Monitor distributes surgical Mask.
- c) Employee returns Face Shield (and N95 Mask if going on break) to Area B; places N95 in the collection box (if the end of shift; Area C).
Note: Hydration Station: area allocated for employees to safely hydrate.
Fit Testing: Area PPE Monitors fit test employees on an as-needed basis.
Partners Gown Policy Change: Before this policy implementation, staff was required to change gowns after contact with every patient. Due to the high gown burn rate associated with this process and following current CDC guidelines, staff was instead instructed to doff gowns only when visibly soiled or when leaving the patient care area. This was possible since all our patients in the facility were COVID positive.
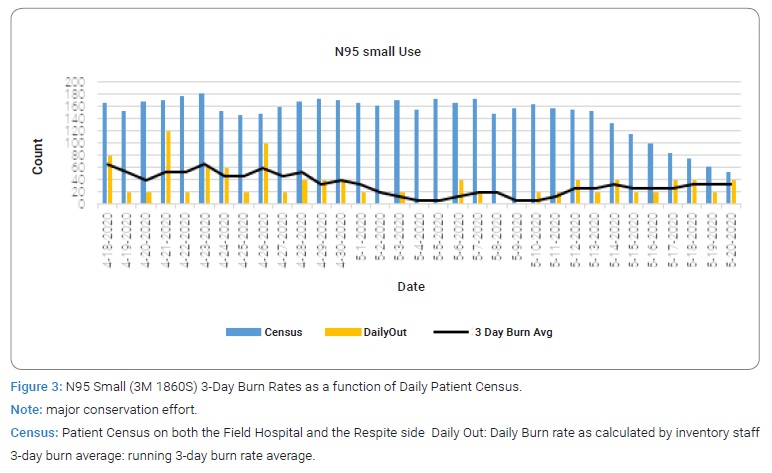
3-Day Average Daily Usage of PPE: To project on-hand supply more accurately, a 24 hour reporting period (7 AM–7 AM the next day) was established. A 3-day rolling average use was created to balance out fluctuations driven by floor traffic and patient care. The three-day rate did not completely smooth weekend fluctuations.
Implementation of PPE Monitors: The doffing of PPE is the highest risk time for self-contamination [5]. Which was essential for employing PPE Monitors. Their role was to monitor the donning and doffing tents 24/7 to ensure appropriate procedures were followed by all staff entering and exiting the clinical area. PPE Monitors would distribute PPE to staff as needed and assist them in following best practice hygiene and safety guidelines. With the presence of the PPE Monitors in the donning and doffing areas, a system for same-day N95 reuse was established. Staff exiting the patient care area on break (i.e., during the same shift) were instructed to place their N95 Masks in a shelved paper bag, organized alphabetically. Staff then reused the same N95 Mask upon reentry.
Introduction of Gown Alternatives
Other gowns / Coveralls: Due to the shortage of disposable gowns available to healthcare professionals in Massachusetts, Boston Hope could supplement gown inventory with coveralls. When the disposable gown inventory was depleted entirely on May 4th, staff used coveralls exclusively.
PPE Monitors Distribute N95 Masks upon Employee check-in: To limit the probability that an employee would lose or use an incorrect mask and reduce any staff hoarding of PPE items, PPE Monitors at the Donning Station began to distribute N95 Respirator Masks upon employee check-in. PPE Monitors distributed.
- a) Returned, labeled decontaminated mask (if present).
- b) Unlabeled decontaminated mask (sent from collected failed fit tests).
- c) New Mask according to documented size/model. If the employee did not have documentation as to what size they were fit tested to, the PPE Monitor proceeded to fit test the employee and distribute the Mask they passed with. Fit Testing started with masks that were most abundant in supply and then, should the fit not be adequate, proceeded to masks that were scarcer in descending order.
Decontamination of N95 Masks: N95 masks can be decontaminated using concentrated, vapor phase hydrogen peroxide. The respirators are exposed at the validated concentration level to decontaminate biological contaminants, including the SARS-CoV-2. Battelle CCDSTM can decontaminate the same respirator multiple times without degrading N95 respirator performance.
After every shift, staff members were instructed to place soiled, compatible N95 masks in a collection box which was placed in the doffing tent. Staff labeled the masks with their first and last name and the site unit code. Used masks from failed fit-tests were also collected and added to the shipment.
The masks were then sent in bulk weekly to the Battelle Critical Care Decontamination System plant in Somerville, MA. Decontaminated N95s were returned in bulk weekly and sorted according to make/model and last name, and documentation was taken regarding which employees’ masks were returned. The masks were distributed to respective staff members at the beginning of their shift. Daily inventory checks and inventory QA policies were implemented.
When operations were first underway, daily inventory checks were done by one person. As a best practice, the daily inventory of all PPE categories was conducted by two people to improve accuracy and reduce human error. Daily inventory was taken of all masks, eye shields, and gloves, which were published daily in numerical and graph form for command and leadership, and the burn rate was calculated.
Badge Scanners placed in Donning Area: Badge Scanners were placed at the dining area entrance. Employees were instructed to badge in every time they entered the area, ensuring regular tracking of staff traffic through the site. This, in turn, allowed for better estimation of how often staff was leaving the patient care area and allowed ascertainment of team violating the policies.
No Make-Up Recommendation: Due to a high rate of N95 Respirators disposed of at the CCDS plant (> 50%), a no make-up recommendation was implemented to reduce visible spoilage of N95 masks. These efforts consisted of multiple communications circulated to all staff regarding the request, provision of face wipes in the team changing areas and dining area, signage at the front entrances, staff changing area, and dining area, efforts by ‘PPE Monitors’ to remind staff of the recommendation, and communication during the ‘Introduction to Donning and Doffing Training’ at new staff Orientation. These efforts resulted in our final shipment reducing to a 22% disposal rate, a reduction of 28% failure.
Additional N95 Masks were offered to reduce the burn of N95 3M Small: The N95 Small was consistently in scant supply due to the high frequency of fit success and employee comfort level. This shortage was felt statewide, and thus, maintaining a steady supply from our donators proved challenging. To address these concerns, a request was submitted for N95 alternative masks (both ‘Small’ and ‘Regular’ fit). Employees who were originally fitted to the 3M 1860S were refit-tested to identify an alternative mask that held them. 53% of the employee’s refit-tested (n = 55) successfully passed with an alternative model. Results were documented, and subsequently, those individuals have distributed the newer models, *or whichever model was more considerable in supply, further reducing the 3M 1860S burn rate.
Hydration Station Constructed: A hydration station was placed outside of the doffing tents so staff could safely hydrate without leaving the patient care area and doffing full PPE. Staff degloved, performed hand hygiene and donned new gloves. They then removed eye protection and respiratory masks and placed on a clean paper towel before doffing gloves, performing hand hygiene and hydrating using disposable plastic cups filled from a water jug.
Reusable Gowns Implemented: Reusable cloth gowns were introduced as a gown option on May 12th. These were innovative solutions to solve issues created by the disposable gown shortage and challenges with coverall use/doffing in the patient area. As Boston Hope had an efficient laundry service on-site, this was an option available to our staff where it hasn’t been at other sites. Laundry bins were placed in the doffing tents and throughout the patient care area. Gowns were laundered on-site daily. PPE Monitors were instructed to actively remind staff to place used gowns in the laundry bins to reduce the likelihood that the gowns would be disposed of. Additionally, ‘REUSABLE’ was written in permanent marker across all reusable gowns.
Results
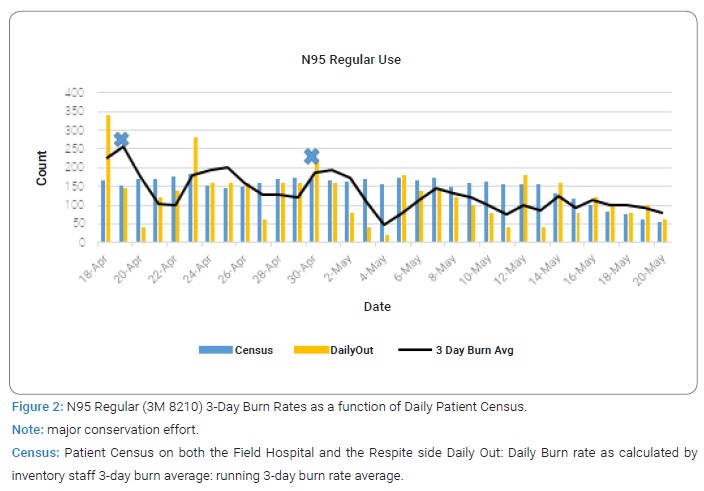
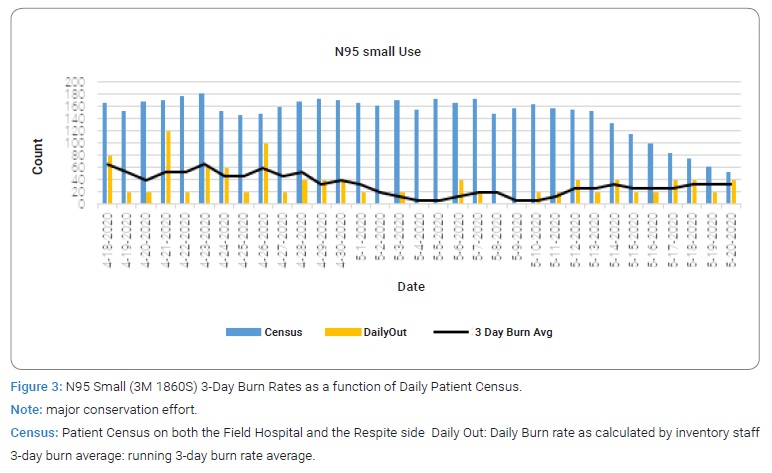
The preservation and management efforts detailed above resulted in an uninterrupted supply of PPE while the hospital was operational. The below graphs illustrate the daily census, daily out and three day burn average from the date that three-day burn averages were calculated (4/18) to when a patient census of zero on the respite side of the hospital was achieved (5/20). Please note when considering the graphs:
- a) Considerable usage fluctuation is observed throughout due to patient headcount, staffing levels, and significant events, considered an event with attendance >1 SD than the daily orientation (i.e., large staff orientation, military fit-testing effort).
- b) Toward the end of the hospital’s operations, there was overstaffing due to a higher than expected discharge rate over the last week (5/16–5/20), which led to a higher daily item burn rate to the patient census.
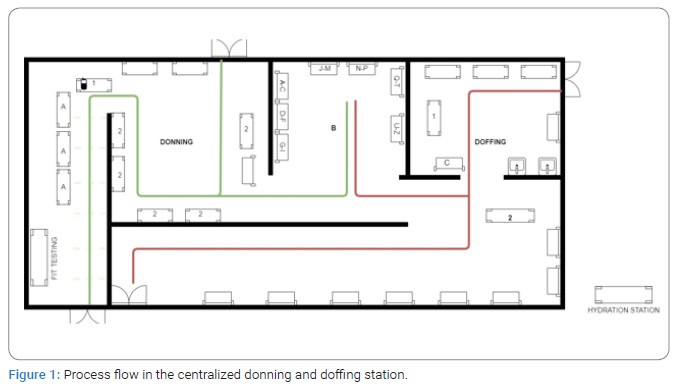
N95 Regular Respiratory Masks 3M 8210 R; see (Figure 2). These were initially an area of concern during the opening phase of operations.
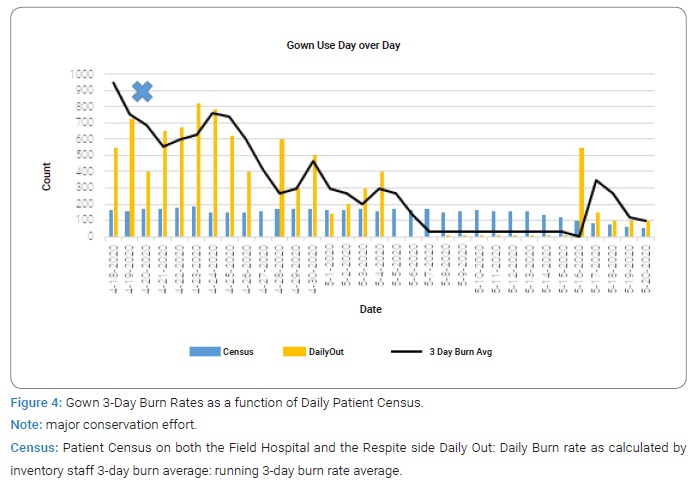
The first option employees were fit-tested to contribute to the initially high burn rate greatly. As employment leveled out and onboarding slowed, regular N95 daily burn steadied. The conservation efforts detailed above (no make-up recommendation, PPE Monitor distribution) significantly contributed to the N95 Regular Mask burn leveling off. These efforts resulted in a 255.7 3-day average burn rate on 4/19 to 187 on 4/30, ultimately a 94 average 3-day burn rate, and a cumulative reduction of 63.24%. N95 Small 3M 1860S; see (Figure 3). Supply consistently approached critical levels and was addressed through the same events as the N95 regular (3M 8210), among others. A steady burn rate was ultimately achieved through these efforts and constant communication with staff on the floor and PPE Monitors. These efforts resulted in a 66.7 3-day average burn rate on 4/19, to 40.0 on 5/1, to ultimately a 26.7 average 3-day burn rate, a cumulative reduction of 59.97%. Gowns see (Figure 4). Initially, there was a high burn rate of gowns due to the MGB-wide gown policy of doffing and donning between patients.
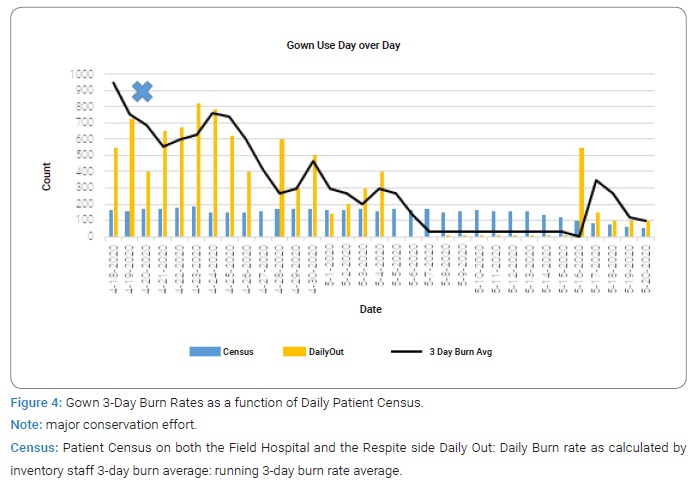
This initial spike eventually flattened through several conservation efforts. The MGB policy change regarding gowns (only removing the gown once soiled) that dropped the burn rate immediately, from a 952 burn rate on 4/18 to 742 burn rate on 4/25, and ultimately 300 3-day average burn rate on 5/1, a cumulative 87.78% reduction. Nonetheless, due to a shortage of disposable gowns in our supply chains, coveralls as a gown alternative were introduced (5/4) as reusable dresses that could be washed and denominated (5/12).
Discussion
The nationwide shortage of Personal Protective Equipment (PPE) during the current COVID-19 pandemic has created multiple issues of procurement and supply chain integrity, potentially affecting patient care and provider safety. It brought into stark reality the collective need for established protocols updated with regard to continually evolving information surrounding proper use and conservation of PPE, particularly in a Field Hospital setting. The rapid construction of the Field Hospital (< 10 days) and the lack of guidelines from similar settings resulted in an initial lack of organization until the taskforce was established. Seemingly mundane feats conducted in established hospitals (equipment to monitor staff traffic, consistent staffing and hiring flow, basic facility amenities (e.g. hydration station). Were initially not available to facilitate proper management and conservation of resources. Additionally, while it was clear from the beginning that N95 respirators would be needed, the resources needed to provide fit testing was not anticipated. Fit testing equipment was not available until approximately 24 hours before opening, and staff needed to be trained on the fit testing procedure, resulting in much confusion as staff worked to catch up to fit testing needs. This understandably resulted in a spike of PPE usage during the initial phases of operation.
However, the PPE Conservation taskforce at Boston Hope Field Hospital quickly learned to respond positively to challenging situations by active problem solving, adhering to the established standards and values, and regularly responding to crisis situations. The construction of a Field Hospital specifically for COVID positive patients allowed for design and operational changes that would not have been possible in traditional hospitals. In most hospitals, the layout, staffing and location of COVID positive patients relies on donning and doffing throughout the hospital at multiple stations (e.g. OR, ER, ICU) and staff specifically assigned with monitoring this process are rare. Our single centralized donning and doffing station and the utilization of PPE monitors was a key element in maintaining functions surrounding quality, safety, and conservation of PPE. Additionally, the consistent emphasis placed on real-time data, alongside the cooperation from leadership at all levels in twice daily briefs, ensured day to day and larger system PPE issues were addressed quickly and efficiently. The assembled taskforce was ultimately able to work preemptively and proactively to solve potential future shortages and flatten PPE usage to a steady level. The BH Field Hospital proved to be a crucial component of the overall strategy of easing the burden on local hospitals during the surge of COVID-19 cases in Massachusetts. The efforts detailed in this report successfully resulted in an uninterrupted PPE supply throughout the 54-day period that the Field Hospital was operational. The Field Hospital ultimately resulted in the cumulative discharge of 723 COVID-negative patients, and consistently maintained the highest standard of safety and care for staff and patients alike.
Article Summary
Strengths and Limitations
- a) To the authors knowledge, this is the first study that describes PPE management and conservation efforts in a COVID-19 Field Hospital in the United States.
- b) This manuscript documents in detail the efforts led by the quality and safety team to preserve PPE supply and system integrity when faced with periodic setbacks and confusion.
- c) These efforts can be easily replicated in other Field Hospital settings.
- d) While we cannot draw sweeping conclusions from isolated interventions or efforts, this paper tracks everyday PPE usage of N95 masks and gowns throughout the time the Field Hospital was operational, which indicates the cumulative effects of the quality improvement initiatives.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- WHO (2020). Shortage of personal protective equipment endangering health workers worldwide.
- Rowan NJ, Laffey JG. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic - Case study from the Republic of Ireland. Sci of the Total Environ. 2020;725:138532.
- Boskoski I, Gallo C, Wallace MB, Costamagna G. COVID-19 pandemic and personal protective equipment shortage: Protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointest Endosc. 2020;92(3):519–523.
- Forrester JD, Nassar AK, Maggio PM, Hawn MT. Precautions for operating room team members during the COVID-19 pandemic. J Am Coll Surg. 2020;230(6):1098–1101.
- Verbeek JH, Rajamak B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020;4(4):CD011621.
Keywords
Quality; Safety; COVID-19; PPE management; Process improvement
Cite this article
Lynch EA, Hutter MM, McCaffrey B, Curley P, Donadio J, Lakin L, et al. Optimization and management of personal protective equipment (PPE) in a COVID-19 positive field hospital . Clin Surg J. 2021;2(3):1–7.
Copyright
© 2021 Richard J. Ehrlichman. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).