The Use of Ambulatory Emergency Care Unit as Supply-Side Drivers for Non-Emergency Surgical Patients during COVID-19 Pandemic Lockdown: An Audit Report from a Tertiary Care Center
* Kausik Ray;
Aaina Mittal;
Christi Swaminathan;
Mandeep Kaur;
Krishna K Singh;
Muhammed S Sajid;
-
* Kausik Ray: Department of Gastrointestinal Surgery, Digestive Disease Center, Brighton & Sussex University Hospitals NHS Trust, UK.
-
Aaina Mittal: Department of Gastrointestinal Surgery, Digestive Disease Center, Brighton & Sussex University Hospitals NHS Trust, UK.
-
Christi Swaminathan: Department of Gastrointestinal Surgery, Digestive Disease Center, Brighton & Sussex University Hospitals NHS Trust, UK.
-
Mandeep Kaur: Department of Gastrointestinal Surgery, Digestive Disease Center, Brighton & Sussex University Hospitals NHS Trust, UK.
-
Krishna K Singh: Department of Gastrointestinal Surgery, Digestive Disease Center, Brighton & Sussex University Hospitals NHS Trust, UK.
-
Muhammed S Sajid: Department of Gastrointestinal Surgery, Digestive Disease Center, Brighton & Sussex University Hospitals NHS Trust, UK.
-
Oct 15, 2020 |
-
Volume: 1 |
-
Issue: 5 |
-
Views: 2617 |
-
Downloads: 2354 |
Abstract
Background: Surgical Ambulatory Emergency Care (AEC) provides better patient flow, improves patient experience, and reduces hospital admissions. This study aims to assess the functionality pattern of an AEC for acute surgical patients in a tertiary care hospital.
Methods: Using the National Health Service Improvement (NHSI) guidelines, the review outcomes of 50 consecutive patients attending AEC were gathered and compared with the results of previously collected data to complete an audit cycle which coincidentally happened during the COVID-19 pandemic lockdown.
Results: More male (54% vs. 38%) and relatively younger patients (age > 71 years 8% vs. 16%) underwent acute surgical review in AEC during the lockdown. The review rate by senior surgeons had increased from 38% to 100%. The discharge rate (72% vs. 60%) with a complete discharge summary (94% vs. 82%) increased significantly. As more patients were referred for acute surgical review, the process-driven component of ‘Provider’s effort’ remained the most effective tool despite showing a drop from 60% to 52%. The pathway-driven component improved due to more follow-up reviews. Increased workload prolonged the mean patient stay time. Category 4 (waste-capacity) patients were reviewed more (22% vs. 18%) in the second limb.
Conclusion: Improvement of various components of AEC services following the application of NHSI recommendations was observed. However, a higher number of follow-up patients at AEC were treated due to lack of face-to-face clinic facilities during lockdown which resulted in an upsurge in the waste category.
Introduction
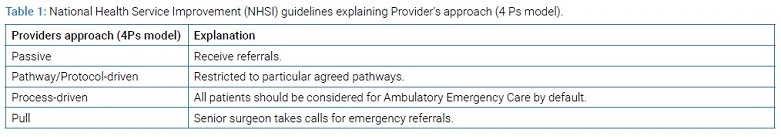
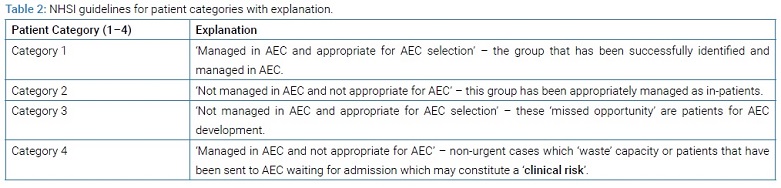
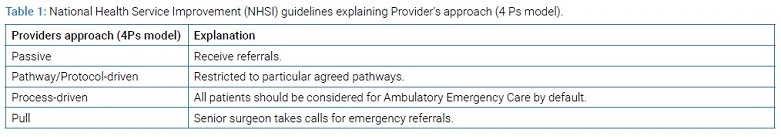
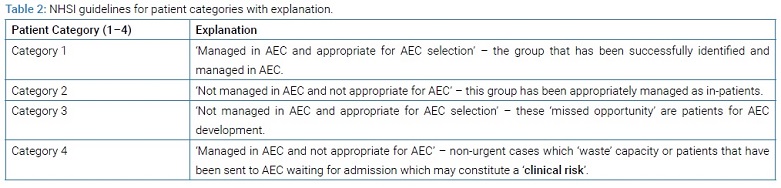
The concept of Ambulatory Emergency Care (AEC) was first introduced in 2007 by the National Health Service Institute for Innovation and Improvement (NHSI). It is updated subsequently, at a regular interval for serving the interest of patients, health-care providers, and hospitals throughout the NHS [1]. The major objective of establishing AEC services is to manage a notable number of emergency patients on the same day without the need for hospital admission. In AEC the acute surgical patients are managed appropriately with sound clinical assessment and rapid access to investigative measures is provided in a timely manner. In this way, it gives the opportunity to manage patient flow better, improve the patient’s experience, and reduce acute hospital admissions [1–4]. Approximately 20% of overall emergency patients have been reported as suitable for ambulatory care treatment [3]. The development of acute ambulatory surgical services can reduce surgical admissions for sub-acute surgical conditions such as abscess, biliary colic, cholecystitis, and non-specific abdominal pain by up to 30% and thereby reducing the cost significantly by avoiding frequent hospital visits [5]. NHSI has published several guidelines to improve AEC services aiming to improve patient care and management pathway in acute settings. The health-care provider’s effort or drive was classified into 4Ps (Table 1) and the patients attending AEC were categorized into 4 groups (Table 2) [2].
Brighton & Sussex University Hospitals NHS Trust is a tertiary care referral center for major regional trauma network, for the management of upper and lower gastrointestinal cancer and it is equipped with all modern-day multi-specialty care facilities. This Trust provides health care facilities to almost half a million population on the South Coast of England. There is a well-established AEC unit that provides ambulatory acute care services to several medical and surgical disciplines. The primary purpose of this study was to assess the performance of AEC in terms of providing care to acute surgical patients and comparing it with the published guidelines of NHSI by completing an audit cycle. In addition, the influence of the COVID-19 pandemic lockdown on the provision of AEC services to acute surgical patients was also evaluated because the second part of the study was conducted during the lockdown.
Methods
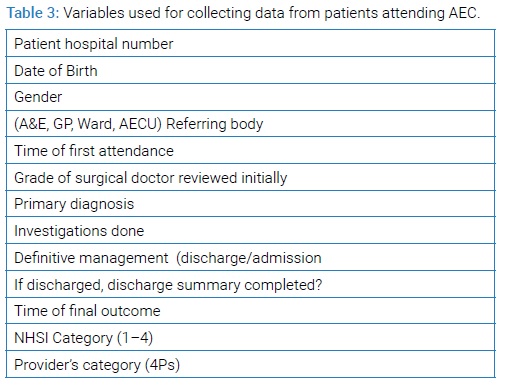
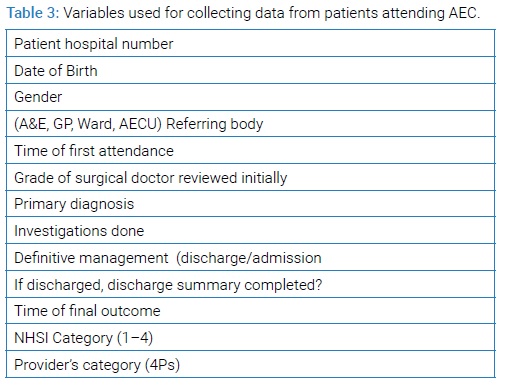
NHSI guidelines for AEC workflow improvement were used as a standard to conduct this audit project [2]. The idea was discussed in Clinical Governance (CG) meeting and approval was obtained for this Quality Improvement Project (QIP). It was approved by the local audit & research department. Data was collected and saved on the Microsoft Excel spreadsheet. The variables used for the data collection on the spreadsheet were agreed among the audit team which is shown in (Table 3).
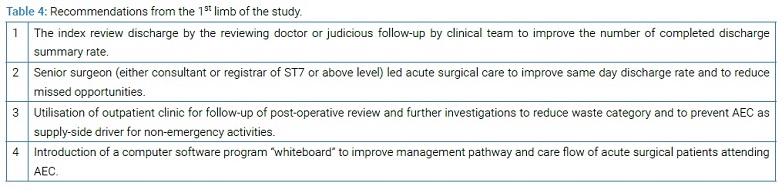
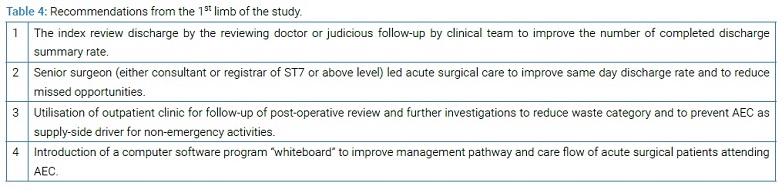
The first audit was commenced on the 21st of October, 2019 and data was collected on 50 consecutive surgical patients who attended AEC. The 4Ps classification of “provider’s effort” and patient categories were classified by the senior author who has 20 years experience in surgery and conducting research studies. Data wasanalysed and the findings of the first limb of this audit project were discussed in the departmental CG meeting and recommendations (Table 4) were implemented by spreading the message through posters and e-mails among all concerned individuals to improve the outcomes of the AEC unit for acute surgical patients. The second limb of the study (re-audit) was commenced (which coincided with the COVID-19 pandemic lockdown) on the 21st of April, 2020 and the data of 50 consecutive acute surgical patients was collected for comparison purposes.
Results
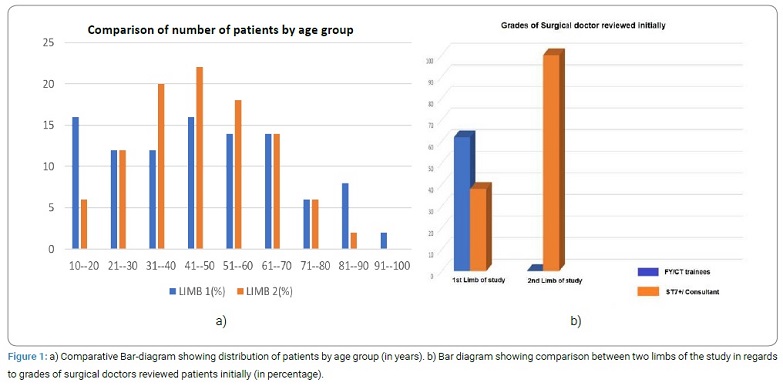
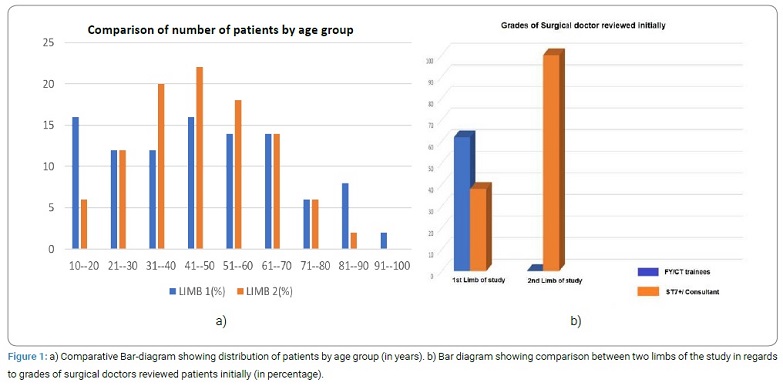
The mean age of the study group in the first limb was 46.8 (18–97) years and 45.6 (17–89) years in the re-audit. The age distribution pattern and variation between both limbs are given in (Figure 1a) showing the relatively less attendance of elderly population to AEC. There was female preponderance (62%) in the first limb of the study, however, in the second limb, the male preponderance (54%) was observed. The source of referral significantly varied between both limbs of the audit. The number of referrals from the general practitioner reduced to 12 (24%) patients from 20 (40%) in the previous limb. Ward referrals for reviews and follow-up increased from 5 (10%) patients to 13 (26%) during the second phase of the study. The referral rate from the accident and emergency department remained almost similar (18 patients vs. 19 patients). Obliging the recommendation from 1st limb and lockdown related rota modification (More senior doctors for emergency service and junior trainees for ward-based service), initial review rate by the consultant/senior trainee (ST7 or above) increased significantly from 38% to 100% (Figure 1b).
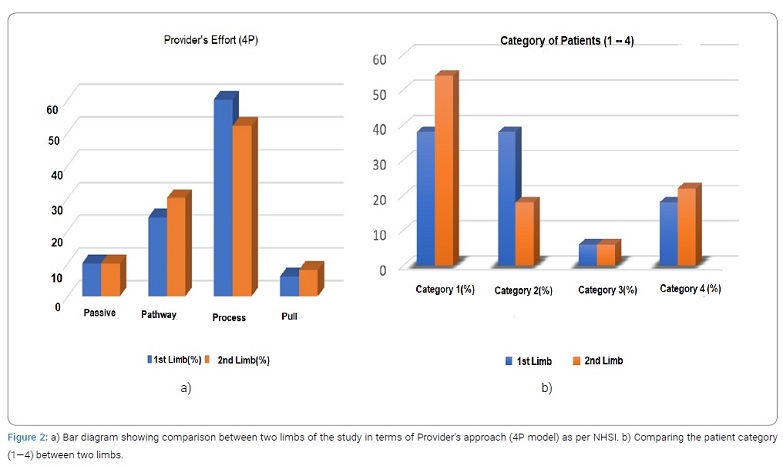
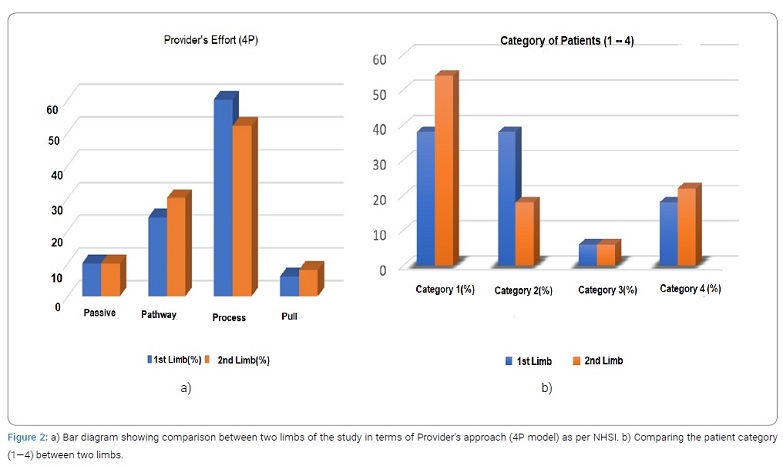
By using the 4Ps model of “provider’s effort”, the process-driven component remained the most effective tool despite showing a drop from 60% to 52% (Figure 2a). Pathway-driven component improved due to more follow-up appointments requiring review in AEC as the face-to-face clinic facility was completely closed. Workload also increased significantly as more patients were referred for surgical review at AEC unit. Due to the increase in the workload, mean patient stay-time prolonged from 3.42 hours to 4.22 hours. In-patient admission following AEC review was reduced to 14 (28%) from 20 (40%) and the number of completed discharge summaries increased to 47 (94%) from 41 (82%) which might be explained by the fear-factor related to COVID crisis among patients, more review by senior doctors and, more number of follow-up patients. The distribution of “provider’s effort” (the 4Ps) was passive in 10% of patients (similar as seen in the first audit), pathway-driven in 30% (24% in the first), process-driven in 52% (60% last time) and pull category were 8% (6% in the first limb; Figure 2a). The distribution according to patient categories was 54% of patients (38% in the first limb) in category I, 18% (38% in the first limb) in category II, unchanged in category III patients (6% each) and 22% of patients were classified into the category IV (18% in first limb) (Figure 2b). As a result of lockdown, more routine post-operative patients were reviewed at AEC causing an increase in category 4 patients (waste-capacity).
Discussion
The findings of current QIP demonstrate the improvement of various components of AEC services following the application of NHSI recommendations and an increased number of routine follow-up patients were seen in AEC due to lack of face-to-face clinic facility during lockdown which resulted in an upsurge in the ‘waste capacity’ patients. In contrary, Decision makers’ inexperience, Poor understanding of AEC services, pressure from A&E and inappropriate use of AEC for elective cases were identified as contributing factors in the first limb. The COVID-19 pandemic in the United Kingdom, as well as worldwide, resulted in the lockdown in addition to the shielding, and isolation of high-risk population. It also led to the cancellation of all elective surgical procedures [9–11]. The recommendation from the Royal College of Surgeons of England stated that surgical services should triage non-emergency surgery, change clinical networks and rotas, and adapt to the virtual outpatient clinics [10]. The unprecedented crisis posed a challenge for there view of complex chronic and, post-operative patients due to abrupt cut-off of out-patient clinic service as well as redistribution of the workforce. Our audit clearly reflected that picture. The review rate of overall (both acute and follow-up) surgical patient in AEC substantially increased causing an upsurge in the pull and process-driven components of “provider’s effort” in addition to an increase in the ‘waste capacity’ (who were not appropriate for AEC) category of patients. Association of Surgeons of Great Britain and Ireland advised increased presence of consultants on the surgical triage area on a regular basis to speed throughput, avoid crowds at the waiting area, and facilitate prompt decision making to reduce unnecessary admissions during COVID-19 pandemic [11]. Similar studies in the past suggested that review by a senior surgeon would improve the decision making, same-day discharge rate, and patient satisfaction [7,8]. Communication between the referring body and a senior surgeon also improves the proper selection of patients for AEC services [6]. The recommendation from the 1st limb of this quality improvement project was to increase the consultant/senior doctor (ST7 and above) review rate for better outcomes. The remarkable improvement in the senior review was observed (from 38% to 100%) in second limb of the study that resulted in fewer hospital admissions. The introduction of ‘Whiteboard’ also improved better notification of patient’s journey resulting in more numbers of complete discharge summary. In the 1st limb of the audit, patients with missed opportunity (6%) and ‘waste-capacity’ category (18%) accounted for almost one-fourth of AEC referrals which was translated as “supply-side driver for non-emergency activities” [2]. Unfortunately, the re-audit showed an increase in the waste-capacity category and the same amount of missed opportunity despite improved effort due to the lockdown. For developing or improving services, there are three types of measures that need to be considered: outcome, process, and balancing measures [4]. During this crisis, balancing measures and process showed significant adjustment for safe and steady outcomes. There are several limitations of this study. This is just an observational study and timings to conduct the study were diverse between both limbs. Therefore, the comparison between both limbs of the quality improvement project may be considered biased. The sample size is very small which may be considered inadequate to justify the conclusions. Despite these limitation authors successfully demonstrated the improvements in service delivery by following the guidelines of NHSI.
Future Implications
Larger numbers of studies are required to strengthen the existing evidence for the improvement of AEC services. A dedicated surgical AEC services as compared to the performance of general AEC looking after medical and all surgical specialties may result in entirely different outcomes. The increased “waste capacity” patients seen in AEC during COVID-19 lockdown may well be a good alternative for complex surgical patients needing frequent outpatient reviews without compromising the care of acute surgical patients in AEC.
References
- https://improvement.nhs.uk/resources/same-day-emergency-care-ambulatory/
- https://improvement.nhs.uk/documents/583/maximising-aec-services-RIG.pdf
- Royal College of Surgeons of England. Commissioning Guide: Emergency General Surgery (acute abdominal pain). 2014.
- http://www.ambulatoryemergencycare.org.uk/file_download.aspx?id=16712
- Nuffield Trust. Quality Watch report: Focus on preventable conditions. 2013.
- Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- Hubbard T, Thomas R. Improving the surgical hot clinic. BMJ Qual Improv Rep. 2014;3(1):u206573.w2639.
- Kazem MA, Hopley C, Corless DJ. Reducing emergency admissions and length of stay by introducing emergency surgical ambulatory service. Ann Med Surg (Lond). 2019;43:17–24.
- Rajan N, Joshi GP. Covid-19: role of ambulatory surgery facilities in this global pandemic. Anesth Analg. 2020;131(1):31–36.
- https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/
- https://www.asgbi.org.uk/news/2020/mar/30/updated-intercollegiate-general-surgery-guidance-on-covid-19
Keywords
Ambulatory care; Acute surgical patients; COVID-19 pandemic
Cite this article
Ray K, Mittal A, Swaminathan C, Kaur M, Singh KK, Sajid MS. The use of ambulatory emergency care unit as supply-side drivers for non-emergency surgical patients during covid-19 pandemic lockdown: an audit report from a tertiary care center. Clin Surg J. 2020;1(5):1–5.
Copyright
© 2020 Kausik Ray. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).