Early surgical repair of congenital completely buried penis in children – report of 103 cases
* Mumtaz Hussain Shad;
Naila Yaqub;
Hani Mohammad Al-Khalaf;
-
* Mumtaz Hussain Shad: Section of Pediatric Surgery, Department of Surgery, Northern Area Armed Forces Hospital, Hafr Al Batin, Saudi Arabia.
-
Naila Yaqub: Department of Pediatrics, Northern Area Armed Forces Hospital, Hafr Al Batin, Saudi Arabia.
-
Hani Mohammad Al-Khalaf: Section of Plastic Surgery, Department of Surgery, Northern Area Armed Forces Hospital, Hafr Al Batin, Saudi Arabia.
-
Oct 28, 2020 |
-
Volume: 1 |
-
Issue: 5 |
-
Views: 12368 |
-
Downloads: 4008 |
Abstract
Objectives: The aim of this study is to present the single surgeon’s experience in the early surgical repair of Congenital Completely Buried Penis (CCBP) in a series of 103 boys.
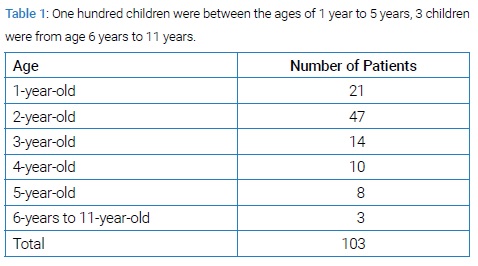
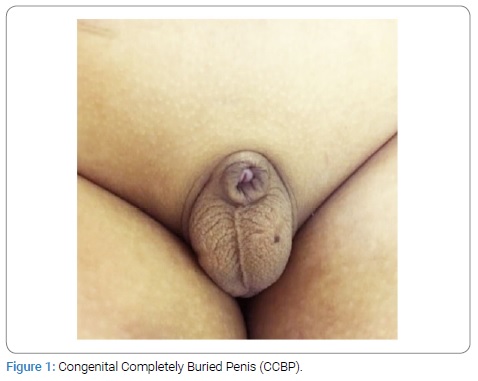
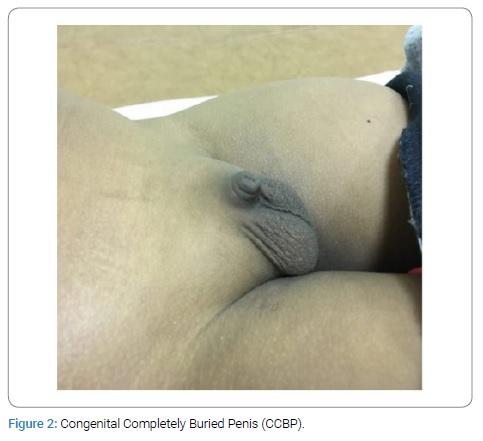
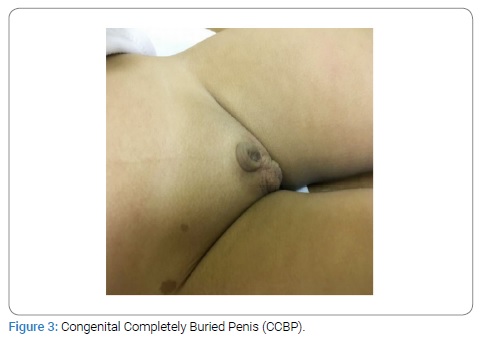
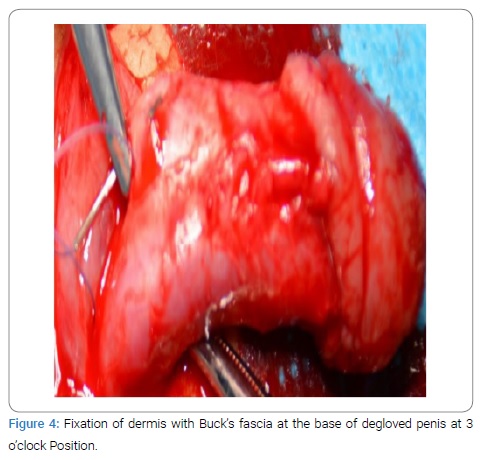
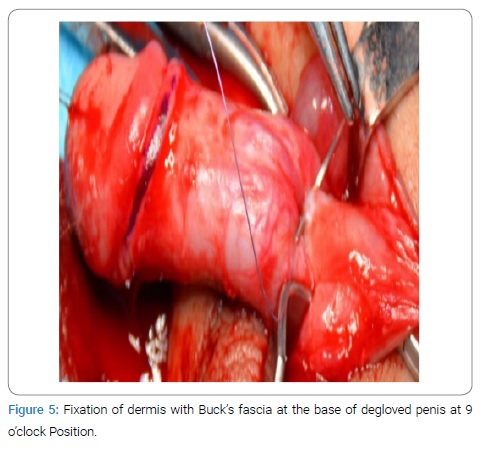
Methods: This is a retrospective study of management of patients of CCBP at the median age of 28 months between May, 2012 and March, 2019. All the children were followed up for 6 months. One hundred children were between the age of 1 to 5 years and 3 children were from the age of 6 to 11 years. All the patients underwent examination to exclude associated anomalies. All children with Congenital Partially Buried Penis (CPBP) and all obese children with Body Mass Index (BMI) more than 85th percentile were excluded from surgical repair. The repair was done using simple technique of penile degloving, release of abnormal Dartos bands and fixation of skin dermis with Buck’s fascia at 3- and 9-o’clock positions. At completion of surgery, technique of compression dressing with transparent TegadermTM was used for 72 hours in all patients
Results: All of 103 patients had excellent cosmetic and functional outcome without any complications. Two patients had developed mild hematoma which resolved spontaneously. All parents were pleased with immediate results.
Conclusion: Early surgical correction of CCBP by technique of penile degloving, release of abnormal Dartos bands and fixation of skin dermis with Buck’s fascia at 3- and 9-o’clock positions is simple, safe and effective. Compression dressing with transparent TegadermTM prevents complications of hematoma formation and wound infection.
Abbreviations
CCBP: Congenital Completely Buried Penis; CPBP: Congenital Partially Buried Penis; BMI: Body Mass Index
Introduction
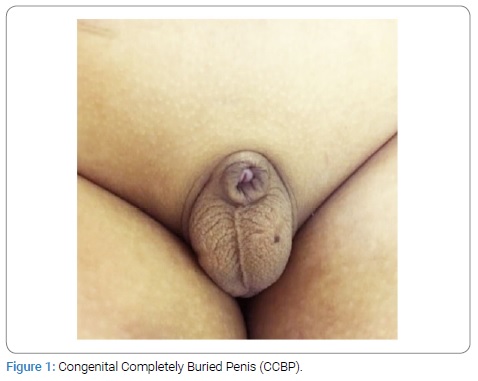
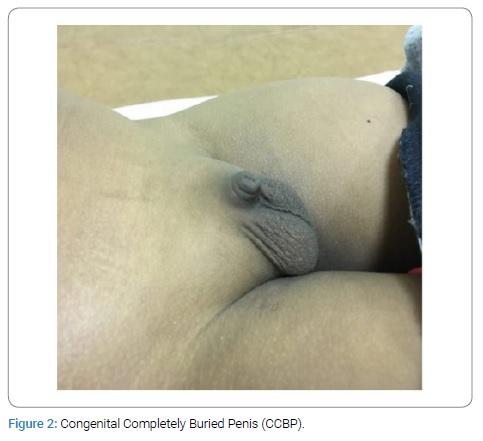
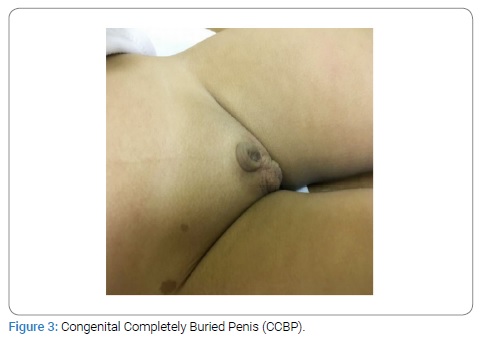
Buried penis in children is a congenital anomaly characterized by a normal sized penis which is retracted within pre pubic tissue [1–3]. This condition is often due to mal-development of penile shaft skin. The penis lacks appropriate sheath of skin with abnormal lateral Dartos bands causing retraction below the skin [3]. It is often a cause of great concern to the parents. This condition was first described by Kayes in 1919 [1,4]. There are two types of Congenital Buried Penis, Congenital Completely Buried (CCBP) and Congenital Partially Buried Penis (CPBP). It is widely regarded as a condition which is difficult to manage. In partial type the proximal half of the penile shaft is buried in pre-pubic tissue. In the complete type, the phallus is completely invisible [5,6]. Buried penis was first classified by Crawford into partial and complete types in 1977 [3–5]. The CPBP usually resolves spontaneously and needs late circumcision usually at the age of two years for better cosmetic results [6]. The CCBP in children is an important clinical entity as it does not resolve spontaneously with age. CCBP needs early surgical correction in children [7–9]. The patients with obesity having Body Mass Index (BMI) more than 85th percentile or those patients having syndromic features need dietary advice and endocrine evaluation [7]. The CCBP may lead to many problems including obstruction of urinary stream, poor hygiene, soft tissue infection, phimosis, poor cosmoses, difficult accessibility and parental anxiety [10–12]. The etiology of CCBP is not clear. Most widely accepted hypothesis for CCBP is that the abnormal lateral Dartos bands retract the penile shaft [13–16]. The commonly performed surgical correction is based on the principle of complete degloving of penile skin along Buck’s fascia to release the lateral Dartos bands which cause tethering of penis [17–20]. There is no unanimous consensus about “gold standard” surgical correction of CCBP. Different surgical techniques have been described to correct the condition [21]. We present our experience with commonly used surgical technique for correction of CCBP based on anatomical findings, with satisfactory cosmetic and functional outcome. Our mean operative duration was 50 (40–60) minutes. We used technique of compression dressing with transparent TegadermTM and kept it for 72 hours to avoid hematoma formation and prevention of infection due to exposure of wound to urine and stool. The patients were discharged home after removing the dressing on 3rd postoperative day and were advised daily sitz baths for 5 days at home. The follow-up appointment in outpatient clinic was given after one week and then after six months.
Objective
The aim of this study is to present single surgeon’s experience in the early surgical repair of Congenital Completely Buried Penis (CCBP) in a series of 103 boys.
Material and Methods
This is a retrospective study of management of 103 consecutive patients with median age of 28 months who underwent repair between May, 2012 and March, 2019 in a single institution by single pediatric surgeon. Indication for surgery was Congenital Completely Buried Penis (CCBP) and parents’ concern. All the patients were referred from circumcision clinic and primary health centers. The children were otherwise healthy, non-obese with BMI ranging from 5th percentile to below 85th percentile. The patients did not have any syndromic features. All patients underwent complete local examination to exclude any associated anomalies such as hypospadias, chordee and severe torsion. All the obese boys with BMI more than 85th percentile were excluded from surgical correction. Congenital Partially Buried Penis (CPBP) and patients with syndromic features were also excluded from surgical treatment. The relevant investigations were within normal range. One hundred children were between the ages of 1 year to 5 years, 3 children were from age 6 years to 11 years as mentioned in (Table 1).
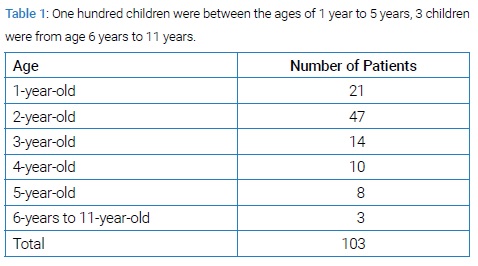
All the children were given appointments for elective admission, through the out-patient clinic, one day prior to surgery (Figures 1–3). The repair was done under general anesthesia.
Surgical technique
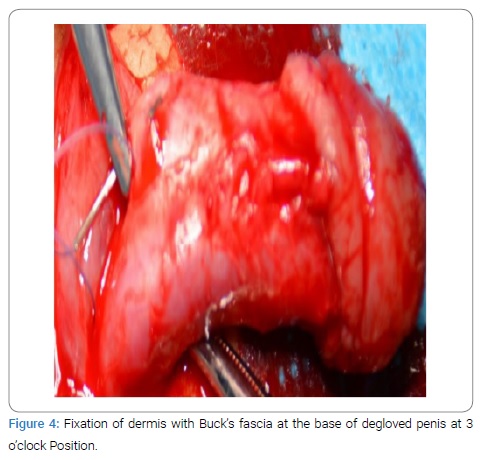
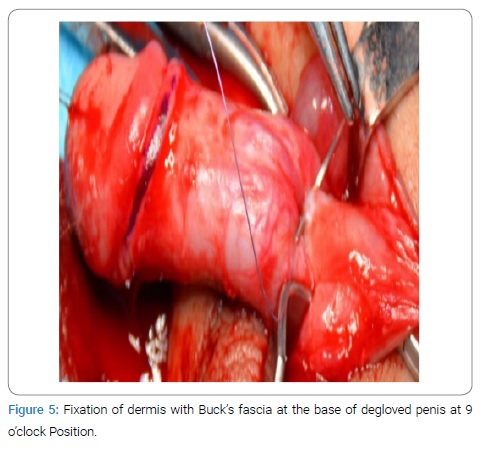
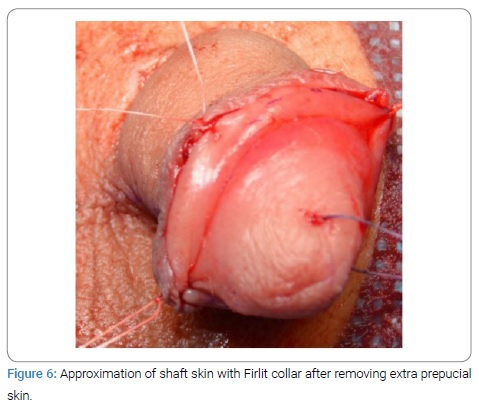
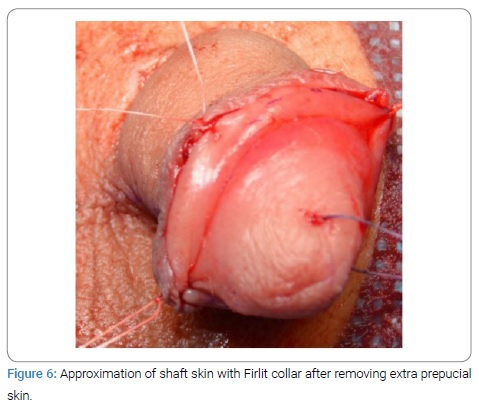
In this series we used commonly practiced surgical technique for correction of CCBP in all boys. A stay suture with 4/0 vicryl is placed through the glans to give control and traction of the penis. Skin marking is done at the base of the penis at 3- and 9-o’clock positions and at the site of circumferential incision leaving 2 mm of Firlit collar distally. Circumferential incision is given at the previously marked site. Complete degloving of penile shaft skin is done in the subdartos plane to preserve dorsal neurovascular bundle. The abnormal lateral Dartos bands are sharply released. The penis is degloved to its base dorsally and to peno-scrotal junction ventrally. The author invariably performs the technique of two points fixation by fixing dermis of penile shaft skin at its base with Buck’s fascia at 3- and 9-o’clock positions by vertical mattress sutures with 4/0 vicryl. The extra outer prepucial skin is marked and removed for approximation with distal Firlit collar of inner prepuce using 5/0 vicryl (Figures 4–6).
We used the technique of compression dressing with transparent TegadermTM in all patients at completion of surgery for 72 hours to avoid wound infection and hematoma formation (Figure 7).

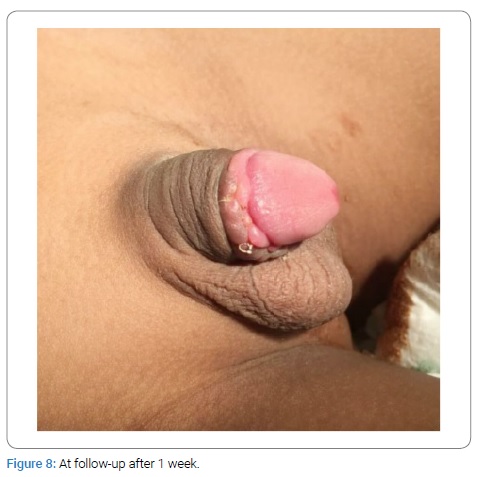
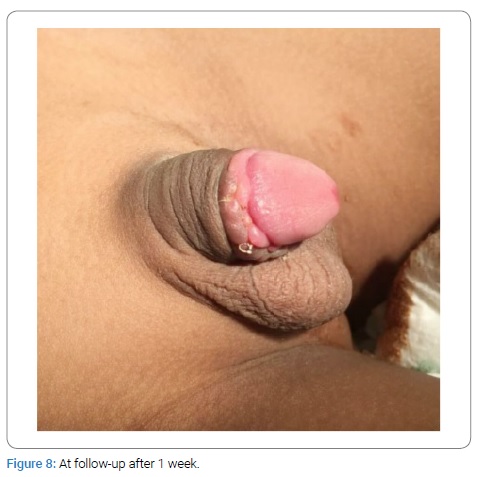
In all patients complete penile shaft coverage with skin was accomplished. We avoided circumferential incision at the base of penis which leads to postoperative lymphedema. We avoided vertical incision in median raphae of shaft skin. We avoided tacking of penis base with pre-pubic / surrounding tissue. In our patients stretched penile length ranged from 2.3 cm to 4.2 cm (mean 3.1 cm). The glans length from the tip dorsally to the corona ranged from 0.9 cm to 1.6 cm (mean 1.2 cm). All patients received perioperative IV antibiotics and analgesia for 72 hours. The patients were discharged home on 3rd postoperative day with advice for sitz baths twice daily for 5 days. All patients were given appointments in pediatric surgical outpatient clinic after one week (Figure 8). The children remained under mean follow-up for 6 months.
Results
The age of patients at operation varied from 1 year to 11 years. Median age was 28 months. All the patients had excellent outcome with uniformly improved visualization of penile shaft immediately after surgery. There were no per-operative or post-operative complications. Two patients had developed mild hematoma due to displacement of transparent TegadermTM transparent dressing which resolved spontaneously within few days. No revision of repair was needed in any patient. All parents were pleased with the outcome immediately after surgery and at review on follow-up.
Discussion
Congenital Completely Buried Penis (CCBP) is a condition characterized by a normal sized penis hidden below the surface of the skin due to the lack of fixation of penile shaft skin. It is retracted by abnormal Dartos bands [1–3]. This condition can lead to obstruction of urinary stream, poor hygiene, soft tissue infection and phimosis [12,13,21]. The treatment should aim to restore an aesthetic and functional penis. Literature shows wide variety of approaches to correct this condition [3,22,23]. Some authors do not recommend fixation sutures between dermis of penile shaft skin with Buck’s fascia and depend upon natural fixation of skin with penis by healing [4,24]. However fixation of penile shaft skin with Buck’s fascia is widely practiced [1,2,21,25]. Borsellino emphasizes that the key to correction is the release of abnormal Dartos bands and fixation of penile skin to Buck’s fascia [18–20,26–28]. In a study published in the Journal of Pediatric Surgery 1995, the technique for repair of buried penis is based on the recognition that the root of the penis is displaced below its normal position resulting into enveloping of penile shaft in the surrounding fat and Dartos tissue. The procedure described for correction was dissection at the root of the penis carried out deep down to the corporal bodies. All fibrotic tissue that binds the penile shaft is excised. The lengthened penile shaft is anchored at its base by suturing the surrounding tissue with tunica. This technique has been applied in 22 patients with age ranging from 5 months to 11 years. Apart from two patients with technical problems all other patients had satisfactory correction with good functional results [4,21,23,25,27–29]. In another technique applied in a series of 50 cases published in the Journal of Pediatric surgery in 2001 the authors avoided circumferential incision at the base of the penis, thus decreasing post-operative edema [6,17,20,22,28–30]. The authors used the technique of vertical mattress sutures at the base of the penile shaft skin to the underlying corpora [6,17,20,31]. In another study published in Pediatric Surgery International in 2009 reported 100 cases. The technique used was based on a vertical incision in the median raphe, complete degloving of penis and tacking its base to the prepubic fascia. Shaft skin is attached to the base of the penis with vertical mattress sutures [6,12,23,31]. The number of fixation sutures varies among the clinicians [6,9,24]. In our series degloving of penile shaft skin was achieved through distal circumferential incision. Thus dissection is done from distal to proximal base. The lateral Dartos bands were released sharply. This enables clear and safe visualization of dissection plane protecting neuro-vascular structures. We used simple two point fixation by vertical mattress sutures between the dermis of penile shaft skin at the base with Buck’s fascia at 3- and 9-o’clock positions to prevent retraction of penis. We used technique of compression dressing at completion of surgery with transparent TegadermTM for 72 hours in all our patients to avoid wound infection and hematoma formation.
Conclusion
Congenital Completely Buried Penis (CCBP) is an important surgical entity in children and needs proper management for good cosmetic and functional outcome. Although there are different operative procedures described in the literature, in this series we found that early surgical correction of CCBP by simple technique of degloving penile shaft skin and release of abnormal lateral Dartos bands followed by two point fixation at 3- and 9-o’clock positions of the dermis of penile shaft skin at its base with Buck’s fascia is simple, safe and effective. At completion of surgery, use of technique of compression dressing with transparent TegadermTM for 72 hours is useful to avoid wound infection and hematoma formation. No additional procedures are required to ensure successful cosmetic and functional outcome. This technique is already being wildly practiced with excellent results. Patients with CPBP need only delayed circumcision. The obese or syndromic patients need dietary management and further evaluation.
Statement of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Statement of Ethics
This is a retrospective study of early surgical repair of Congenital Completely Buried Penis (CCBP) in children – Report of 103 cases. It is approved by Institutional Review Board, Al Imam Mumammad Ibn Saud Islamic University, Riyadh, Kingdom of Saudi Arabia. Project Number 51-2019, Dated: May 26, 2019. The consents for all 8 figures are secured from the parents for the purpose of publication.
References
- Hesham Kassem, Wael Alshahat, Mohamed Khalifa. Early surgical correction of buried penis. Ann Pediatr Surg. 2018;14:83–86.
- Hadidi AT. Buried penis: classification surgical approach. J Pediatr Surg. 2014;49(2):374–379.
- Xing Liu, Da-wei He, Yi Hua, De-ying Zhang, Guang-hui Wei. Congenital completely buried penis in boys: anatomical basis and surgical technique. BJU Int. 2013;112(2):271–275.
- Smeulders N, Wilcox DT, Cuckow PM. The buried penis-an anatomical approach. BJU Int. 2000;86(4):523–526.
- Crawford BS, Buried penis. Br J Plast Surg. 1977;30(1):96–99.
- Liu X, He DW, Hua Y, Zhang DY, Wei GH. Congenital completely buried penis in boys: Anatomical basis and surgical technique. BJU Int. 2013;112(2):271–275.
- Alter GJ, Horton CE, Horton Jr CE. Buried penis as a contraindication for circumcision. J Am Coll Surg. 1994;178(5):487–490.
- Ferro F, Spangnoli A, Spyridakis I, Atzori P, Martini L, Borsellino A. Surgical approach to the congenital megaprepuce. J Plast Reconstr Aesthet Surg. 2006;59(12):1453–1457.
- Rivas S, Romero R, Parente A, Fangjul M, Angulo JM. [Simplification of the surgical treatment of a hidden penis]. Actas Urol Esp. 2011;35(5):310–314.
- Alexander A, Lorenzo AJ, Salle JLP, Rode H. The Ventral V-plasty: a simple procedure for the reconstruction of a congenital megaprepuce. J Pediatr Surg. 2010;45(8):1741–1747.
- Oh CY, Lee HY, Hong CH, Han SW. Long-term outcome and parent’s satisfaction after the correction of concealed penis. Korean J Pediatr Urol. 2009;1:58–63.
- Perger L, Hanley RS, Feins NR. Penoplasty for buried penis in infants and children: report of 100 cases. Pediatr Surg Int. 2009;25(2):175–180.
- Chu CC, Chen YH, Diau GY, Loh IW, Chen KC. Preputial flaps to correct buried penis. Pediatr Surg Int. 2007;23(11):1119–1121.
- Jung EH, Son JH, Jang SH, Lee JW. Simple anchoring of the penopubic skin to the prepubic deep fascia in surgical correction of buried penis. Korean J Urol. 2011;52(11):787–791.
- Frenkl TL, Agarwal S, Caldamone AA. Results of a simplified technique for buried penis repair. J Urol. 2004;171(2 Pt 1):826–828.
- Chuang JH, Chen LY, Shieh CS, Lee SY. Surgical correction of buried penis: a review of 60 cases. J Pediatr Surg. 2001;36(3):426–429.
- Brisson P, Patel H, Chan M, Feins N. Penoplasty for buried penis in children: report of 50 cases. J Pediatr Surg. 2001;36(3):421–425.
- Radhakrishnan J, Razzaq A, Manickam K. Concealed penis. Pediatr Surg Int. 2002;18(8):668–672.
- Philip I, Nicholas JL. Congenital giant preputial sac: case report. J Pediatr Urol. 1999;34(3):507–508.
- Cromie WJ, Ritchey ML, Smith RC, Zagaja GP. Anatomical alignment for the correction of buried penis. J Urol. 1998;160(4):1482–1484.
- Joseph VT. A new approach to the surgical correction of buried penis. J Pediatr Surg 1995;30(5):727–729.
- Asimakopoulos AD, Iorio B, Vespasiani G, Cervelli V, Spera E. Autologous split-thickness skin graft for penile coverage in the treatment of buried (trapped) penis after radical circumcision. BJU Int. 2012;110(4):602–606.
- Jung EH, Son JH, Jang SH, Lee JW. Simple anchoring of the penopubic skin to the prepubic deep fascia in surgical correction of buried penis. Korean J Urol. 2011;52(11):787–791.
- Zhao YQ, Zhang J, Yu MS, Long DC. Functional restoration of penis with partial defect by scrotal skin flap. J Urol. 2009;182(5):2358–2361.
- Li CY, Agrawal V, Minhas S, Ralph DJ. The penile suspensory ligament: abnormalities and repair. BJU Int. 2007;99(1):117–120.
- Chuang JH. Penoplasty for buried penis. J Pediatr Surg. 1995;30(9):1256–1257.
- Boemers TM, De Jong TP. The surgical correction of buried penis: a new technique. J Urol. 1995;154(2 Pt 1):550–552.
- Redman JF. Buried penis: congenital syndrome of a short penile shaft and a paucity of penile shaft skin. J Urol. 2005;173(5):1714–1717.
- Lee T, Suh HJ, Han JU. Correcting congenital concealed penis: New pediatric surgical technique. Urology. 2005;65(4):789–792.
- Chuang JH, Chen LY, Shieh CS, Lee SY. Surgical correction of buried penis: a review of 60 cases. J Pediatr Surg. 2001;36(3):426–429.
- Borsellino A, Spagnoli A, Vallasciani S, Martini L, Ferro F. Surgical approach to concealed penis: technical refinements and outcome. Urology. 2007;69(6):1195–1198.
Keywords
Congenital completely buried penis (CCBP); Congenital partially buried penis (CPBP); Penile degloving; Release of dartos bands; Buck’s fascia; Dermis; Two point fixation
Cite this article
Khan MH, Yaqub N, Al-Khalaf HM. Early surgical repair of congenital completely buried penis in children – report of 103 cases. Clin Surg J. 2020;1(5):1–6.
Copyright
© 2020 Mumtaz H Khan. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).