Symptomatic Portal Biliopathy – Surgery for failed Endoscopic Management
* Sastha Ahanatha Pillai;
Karthikeyan Srinivasan;
Padmanabhan S;
-
* Sastha Ahanatha Pillai: Department of Surgical Gastroenterology, Madurai Medical College, India.
-
Karthikeyan Srinivasan: Department of Surgical Gastroenterology, Madurai Medical College, India.
-
Padmanabhan S: Department of Surgical Gastroenterology, Madurai Medical College, India.
-
May 18, 2020 |
-
Volume: 1 |
-
Issue: 3 |
-
Views: 3277 |
-
Downloads: 1960 |
Abstract
Background: Patients with chronic portal venous obstruction can develop portal cavernoma and obstruction in the biliary system, which is termed as portal biliopathy. Symptomatic portal biliopathy requires intervention. It is a complex problem and therapeutic strategy has not been optimized.
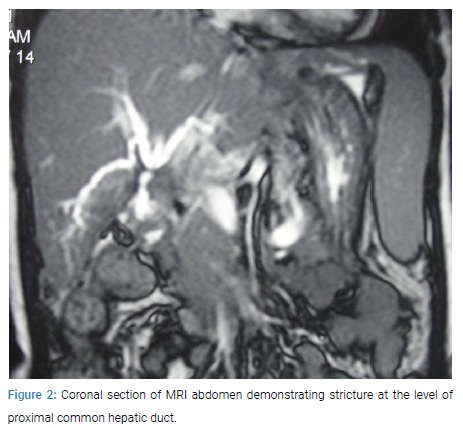
Materials and methods: Retrospectively, details of 23 patients who were admitted between June 2015 and November 2018 with symptomatic portal biliopathy were analysed. Endoscopic stenting was the preferred initial management. Seven patients in whom endoscopic management failed were subjected to surgical intervention. The treatment strategy and outcomes in these seven patients were studied.
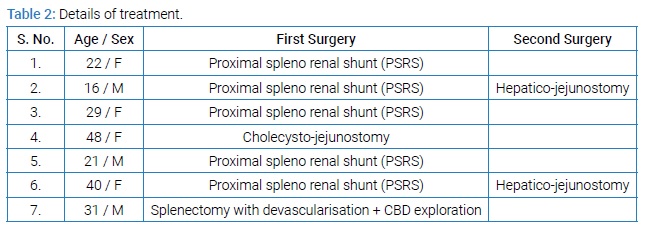
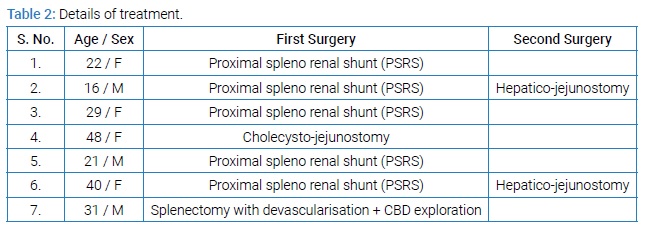
Results: In 5 patients proximal spleno-renal shunt was done as the primary procedure. Three of the patients improved after the shunt procedure. The other 2 patients needed hepaticojejunostomy to treat persistent biliary strictures. Two patients in whom a porto-systemic shunt was not feasible, alternative procedures were done. One patient underwent splenectomy with devascularisation and CBD exploration and the other underwent cholecystojejunostomy.
Conclusion: Portosystemic shunt may be effective in relieving symptoms in patients with portal biliopathy, achieving good long term outcome. Some patients may need bilioenteric bypass as the second procedure to tackle persistent biliary stricture. Treatment needs to be modified according to specific problems of each patient.
Background
Portal biliopathy is a condition which describes the abnormalities in the intrahepatic and extrahepatic biliary tree, gallbladder and the cystic duct in patients with portal hypertension [1]. Portal biliopathy is usually associated with Extrahepatic Portal Venous Obstruction (EHPVO) although it has been described infrequently in patients with Non Cirrhotic Portal Fibrosis (NCPF) [2]. Imaging studies have demonstrated changes of portal biliopathy in 80%–100% of patients with EHPVO, but only about 5%–30% become symptomatic [3–6]. Other biliary diseases like choledocholithiasis, primary sclerosing cholangitis, biliary parasitosis, AIDS cholangiopathy, oriental cholangiohepatitis and cholangiocarcinoma, which can resemble portal biliopathy need to be excluded before making a diagnosis [7]. The natural history and progress of portal biliopathy is not known. Some studies suggest that about 2%–4% of patients with persistent biliary obstruction or inadequate drainage or surgery may go on to develop secondary biliary cirrhosis [5]. Portal biliopathy is relatively rare. The development of symptomatic portal biliopathy is a difficult problem to treat. There is no standard treatment recommendation available for portal biliopathy in literature. There are very little reports on long term outcome analysis following treatment for portal biliopathy. The aim of this study is to present our surgical strategy followed in treating patients with symptomatic portal biliopathy in whom endoscopic therapy failed.
Material and methods
The approval number of the institutional review board of the institution is 37/SGE/2018. Between June 2015 and November 2018, 23 patients were admitted to the Government Rajaji Hospital & Madurai Medical College, Madurai, Tamilnadu, India with symptomatic portal biliopathy. Endoscopic intervention was the preferred initial management. In seven patients with symptomatic portal biliopathy endoscopic management failed and these patients needed surgical intervention. Liver function test was done in all patients to assess the severity of liver dysfunction. Upper gastrointestinal endoscopy was done to identify the presence and grade of oesophageal or fundal varices and to rule out malignant distal biliary obstruction. Portal venous doppler study was done to identify the extent of portal venous obstruction or portal cavernoma. Magnetic Resonance Cholagiopancreatography (MRCP) were done to evaluate the site and severity of biliary obstruction. Contrast enhanced CT scan of the abdomen was occasionally needed. Patients with symptomatic portal biliopathy were preferably managed by endoscopic stenting of the biliary system. Endoscopic stenting was done using a single plastic stent whenever feasible. Multiple stents were deployed if symptoms persisted or if patients developed features of cholangitis after the first stenting. Any significant or bleeding varices were managed simultaneously by endoscopic variceal ligation. Patients were put on UDCA 300 mg twice daily after stenting. Any patient who had recurrent symptoms six months after stenting or when endoscopic stenting was not possible was considered for surgery. Initially a portosystemic shunt procedure, proximal splenorenal shunt (PSRS) was done. In some patients, the symptoms of biliary obstruction improved with the shunt alone. No further intervention was needed in these patients. In the rest, a bilioenteric bypass was done in the second sitting. In patients who did not have shuntable vein, alternative procedures were done, either in the form of cholecystojejunostomy or devascularisation with splenectomy.
Results
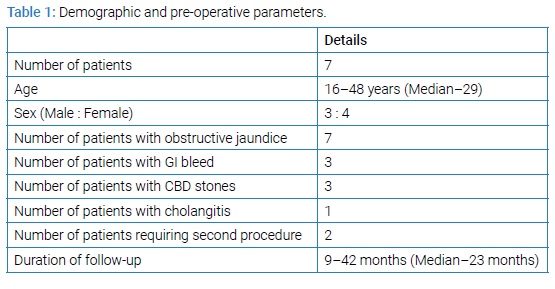
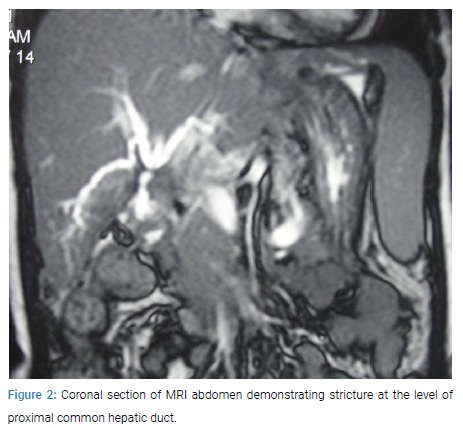
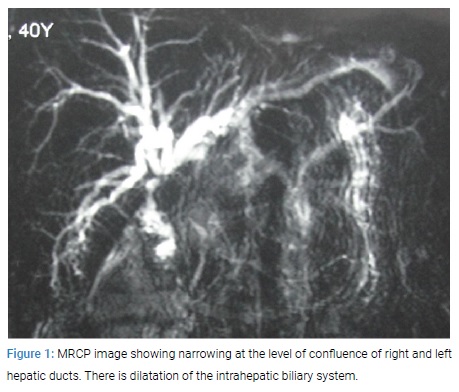
During the study period 23 patients were admitted with symptomatic portal biliopathy. All these patients were planned for endoscopic stenting as the primary treatment. Endoscopic stenting was successful in 16 of these patients. Endoscopic therapy failed in three patients. These three patients had persistent symptoms even after multiple stenting and a median waiting period of 6 ½ months. Endoscopic stenting and was not feasible in four patients. In three patients the common bile duct could not be canulated and in one patient the procedure was deferred because of large periampullary varices. In the seven patients surgical intervention was planned. These seven patients formed the subject of this study. There were 4 females and 3 males. The age of the patients ranged from 16–48 years (median–29 years). Jaundice was the predominant complaint in all of the patients. Three patients had previous gastrointestinal bleed for which endoscopic therapy had been done. One patient had features suggestive of recurrent mild cholangitis. MRCP showed dilatation of intra and extra hepatic biliary radicles with narrowing at the mid or distal CBD in all 7 patients. Stones were seen in the CBD in 3 patients (Table 1).
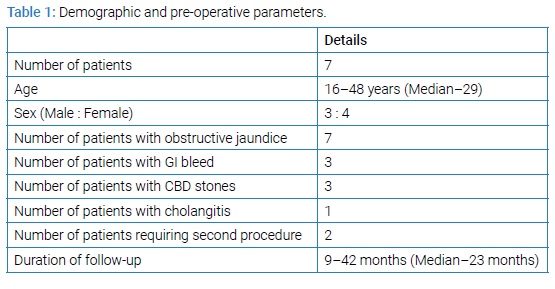
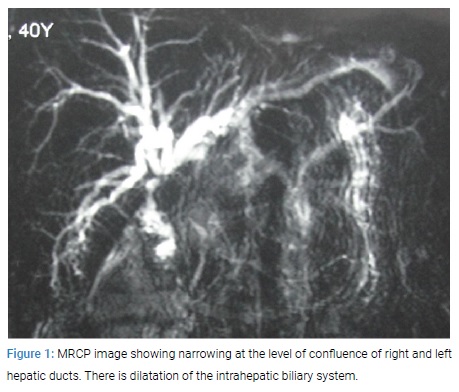
In 5 patients proximal spleno-renal shunt was done as the primary procedure. Three of the patients demonstrated clinical improvement after the shunt procedure. Liver function tests normalised over a period of 5–14 weeks. These patients did not require a second procedure. The other two patients required a bilioenteric bypass in the form of hepaticojejunostomy, three months after the first procedure. One of these patients had persistent elevation of liver function tests and the other had stones in the biliary tree which needed to be removed. In two patients a shunt procedure was not feasible as shuntable vein was not available. One of the patients underwent splenectomy with devascularisation and CBD exploration. The stones in the CBD were removed and the CBD was closed over a plastic stent. This patient was a bleeder and had fundal varices (Figure 1–2).
The surgery was difficult as anticipated. The other patient had recurrent cholangitis. This patient underwent cholecystojejunostomy to relieve the obstruction and cholangitis (Table 2).
These patients were followed up for a period of 9–42 months (median–23 months). Six of the patients are on regular follow-up. Three patients were clinically asymptomatic after surgery. Two patients continued to have mild jaundice or cholangitis on and off which was treated conservatively. Those patients with cholangitis responded to hydration and antibiotic. These patients were also put on prolonged oral ursodeoxycholic acid. One patient needed endoscopic stenting to relieve jaundice. This was done 11 months after PSRS. One patient had an episode of gastrointestinal bleed which was treated by endoscopic banding. One patient succumbed to severe cholangitis 7 months after surgery. This was the patient who underwent splenectomy with devascularisation and CBD exploration.
Discussion
Portal biliopathy is a rare and difficult condition to treat. Three theories have been described as the pathogenesis of portal biliopathy. The first one suggests that the pliable CBD is compressed by the large collateral veins running along the wall of the CBD in patients with portal hypertension. These were demonstrated as indentations on ERCP which represents external compression [8,9]. This theory explains the reversal of biliary obstruction following portal decompressive surgery as demonstrated in various studies [10,11]. Recent studies have demonstrated that microvascular blood flow through the CBD decreased to 62% of normal on clamping the portal vein in patients undergoing pancreaticoduodenectomy [12]. This emphasizes the importance of the portal vein in the vascular supply to the CBD. The supraduodenal common bile duct has the poorest vascular supply and is the most susceptible to ischaemic injury [13]. In the present study 5 patients underwent portosystemic shunt and out of these 3 patients improved, not requiring a subsequent drainage procedure. The effects of portal biliopathy seem to be reversible in the early phase if identified and treated with a shunt procedure. The second theory is that long standing portal venous thrombosis can cause sclerosis of the veins draining the common bile duct. This can affect and damage the capillaries and arterioles. This in turn can lead on to ischaemic strictures of the common bile duct [14]. These ischaemic strictures do not reverse after portosystemic shunt procedures. These strictures warrant a subsequent bilioenteric bypass. Infection or cholangitis is speculated as the third reason for biliary strictures [15–17]. Cholangitis can lead on to inflammation and fibrosis leading to biliary strictures. These are also likely to be persistent needing bilioenteric bypass. The last two theories may be the reason for non-reversal of the biliary obstruction in two of the five patients who underwent portosystemic shunt procedures in our study. These patients needed a subsequent hepatico-jejunostomy to drain the obstructed biliary system. It usually takes about 8–10 years for patients with EHPVO to develop symptomatic portal biliopathy. Gallstones may be seen in about one-third to half of the patients and CBD stones may be seen in about 20% [7]. Cholelithiasis and choledocholithiasis may contribute to some of the symptoms. The major difficulty in managing patients with symptomatic portal biliopathy is the rarity of the condition. Making a diagnosis of portal biliopathy is difficult and usually delayed. Hence there is no definite consensus in the management protocol. Various centres have managed patients in different manners according to the facilities and the expertise available in the centre. Advances in interventional endoscopy have facilitated these patients to be managed by non surgical methods. Upfront surgery in these patients is made difficult by the presence of large thin walled collaterals in the wall of the common bile duct. Dissection around the common bile duct and liver hilum may be associated with severe life-threatening haemorrhage [3,18]. Furthermore, some of these patients have intrahepatic strictures which are not amenable for surgical bilio-enteric bypass. So initial exploration of the common bile duct or bilioenteric bypass is not attempted and may be disastrous. Generally endoscopic management is accepted as the initial management, albeit it may not be simple. Endoscopic stenting is difficult in portal biliopathy because of collaterals around the ampulla. Haemobilia may be problematic following endoscopic management and is difficult to manage [19]. Endoscopic placement of plastic stent in the CBD gives long term relief of symptoms in a very small percentage of patients. But endoscopic stenting is needed initially as most patients present with some degree of cholangitis at diagnosis, or patients may not be fit for surgery. Surgical management is reserved for patients in whom endoscopic stenting has failed or is unsuccessful. In our centre 7 out of 23 patients with symptomatic portal biliopathy needed surgery. Splenectomy with proximal splenorenal shunt is the commonest shunt procedure practiced in adults in most centres [20]. In children a mesocaval shunt with jejunal vein interposition was the frequent approach [21]. In our centre as we manage adult patients, proximal splenorenal shunt was used. Some patients may have symptomatic improvement with portosystemic shunts alone. In our study 3 patients improved with shunts alone. Patients who continue to have symptoms following portosystemic shunts need bilioenteric bypass. Bilioenteric bypass may be in the form of hepaticojejunostomy or choledochoduodenostomy [10,22]. In our series both such patients underwent hepaticojejunostomy. We felt the previous shunt made the subsequent surgery easier as it is likely that the collaterals in the wall of the common bile duct shrunk after the shunt. Though it is desirable to do a portosystemic shunt procedure, about 5%–30% of patients with portal biliopathy do not have a shuntable vein [3]. Hence make shift procedures and modifications may be need as a desperate measure. We needed to perform splenectomy and devascularisation with CBD exploration in one patient considering the fact that the patient was a bleeder and other plans had failed. We were forced to perform a cholecystojejunostomy in one patient who had cholangitis and failed endoscopic stenting. The clinical scenario is complicated by cholangitis, persistent stricture, gastro-intestinal bleed and liver failure in the long run. So patients may still need endotherapy after surgery to manage bleed or recurrent or residual biliary strictures. In some studies patients were subjected to repeated percutaneous cholangioscopies to extract biliary stones, in whom endoscopic removal failed. Patients also need to be followed up for long durations. Treatment needs to be individualized and tailored according to severity, symptoms, complications, presence of shuntable vein and response to portosystemic shunt. The rarity of the condition and the different spectrum of presentation prevent the development of a reliable protocol for management.
Conclusion
Portal biliopathy is a complex problem to manage. Treatment becomes essential when patients become symptomatic. Endoscopic stenting is the preferred management. Surgery is reserved for failed endotherapy. Portosystemic shunt may be effective in relieving symptoms in some patients achieving good long term outcome. Some patients may need bilioenteric bypass as the second procedure to tackle persistent biliary stricture. Treatment needs to be modified according to the needs of each patient.
References
- Chandra R, Kapoor D, Tharakan A, Chaudhary A, Sarin SK. Portal biliopathy. J Gastroenterol Hepatol. 2001;16:1086–1092.
- Somnath Chattopadhyay, Samiran Nundy. Portal biliopathy. World J Gastroenterol. 2012;18(43):6177–6182.
- Vibert E, Azoulay D, Aloia T, Pascal G, Veilhan LA, Adam R, et al. Therapeutic Strategies in Symptomatic Portal Biliopathy. Ann Surg. 2007;246:97–104.
- Khuroo MS, Yattoo GN, Zargar SA, Javid G, Dar MY, Khan BA, et al. Biliary abnormalities associated with extrahepatic portal venous obstruction. Hepatology. 1993;17:807–813.
- Condat B, Vilgrain V, Asselah T, O’Toole D, Rufat P, Zappa M, et al. Portal cavernoma-associated cholangiopathy: a clinical and MR cholangiography coupled with MR portography imaging study. Hepatology. 2003;37:1302–1308.
- Sezgin O, Oguz D, Attintas E, Saritas U, Sahin B. Endoscopic management of biliary obstruction caused by cavernous transformation of the portal vein. Gastrointest Endosc. 2003;68:602–608.
- Dhiman RK, Saraswat VA, Valla DC, Chawla Y, Behera A, Varma V, et al. Portal cavernoma cholangiopathy: consensus statement of a working party of the Indian national association for study of the liver. J Clin Exp Hepatol. 2014;4:S2–S4.
- Dilawari JB, Chawla YK. Pseudosclerosing cholangitis in extrahepatic portal venous obstruction. Gut. 1992;33:272–276.
- Sarin SK, Bhatia V, Makwane U. Portal biliopathy in extrahepatic portal vein obstruction. Ind J Gastroenterol. 1992;11(1):A82.
- Agarwal AK, Sharma D, Singh S, Agarwal S, Girish SP. Portal biliopathy: a study of 39 surgically treated patients. HPB(Oxford). 2011;13:33–39.
- Khare R, Sikora SS, Srikanth G, Choudhuri G, Saraswat VA, Kumar A, et al. Extrahepatic portal venous obstruction and obstructive jaundice: approach to management. J Gastroenterol Hepatol. 2005;20:56–61.
- Slieker JC, Farid WR, van Eijck CH, Lange JF, van Bommel J, Metselaar HJ, et al. Significant contribution of the portal vein to blood flow through the common bile duct. Ann Surg. 2012;255:523–527.
- Deltenre P, Valla DC. Ischemic cholangiopathy. Semin Liver Dis. 2008;28:235–246.
- Somnath Chattopadhyay, Samiran Nundy. Portal biliopathy. World J Gastroenterol. 2012;18(43):6177–6182.
- Chaudhary A, Dhar P, Sarin SK, Sachdev A, Agarwal AK, Vij JC, et al. Bile duct obstruction due to portal biliopathy in extrahepatic portal hypertension: surgical management. Br J Surg. 1998;85:326–329.
- O’Donnell B, Moloney HA. Development and course of extrahepatic portal hypertension in children. Lancet. 1968;1:789–791.
- Gibson JB, Johnston GW, Fulton TT, Rodgers HW. Extrahepatic portal-venous obstruction. Br J Surg. 1965;52:129–139.
- Thervet L, Faulques B, Pissas A. Endoscopic management of obstructive jaundice due to portal cavernoma. Endoscopy. 1993;25:423–425.
- Dumortier J, Vaillant E, Boillot O. Diagnosis and treatment of biliary obstruction caused by portal cavernoma. Endoscopy. 2003;35:446–450.
- Choudhuri G, Tandon RK, Nundy S, Mishra NK. Common bile duct obstruction by portal cavernoma. Dig Dis Sci. 1988;33:1626–1628.
- Gauthier-Villars M, Franchi S, Gauthier F, Fabre M, Pariente D, Bernard O. Cholestasis in children with portal vein obstruction. J Pediatr. 2005;146:568–573.
- Chattopadhyay S, Govindasamy M, Singla P, Varma V, Mehta N, Kumaran V, et al. Portal biliopathy in patients with non-cirrhotic portal hypertension: does the type of surgery affect outcome? HPB (Oxford). 2012;14:441–447.
Keywords
Portal biliopathy; NCPF; Portal cavernoma; Portal hypertension; Biliary stricture
Cite this article
Pillai SA, Srinivasan K, Padmanabhan S. Symptomatic portal biliopathy – surgery for failed endoscopic management. Clin Surg J. 2020;1(3):1–5.
Copyright
© 2020 Sastha Ahanatha Pillai. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).