Abstract
Bouveret’s syndrome is a rare form of gallstone ileus caused by the passage and impaction of a large gallstone through a cholecystoduodenal fistula into the duodenum, resulting in gastric outlet obstruction. It is a rare form of gall stone ileus (1-3% of cases of gall stone ileus; gall stone ileus itself is extremely rare occurring in only 0.3-0.5% of patient with cholelithiasis) and causes significant morbidity and mortality1. It is common in elderly female patients with multiple comorbidities including a history of long standing cholelithiasis, presenting with features of small bowel or gastric outlet obstruction. A high index of suspicion is essential for prompt diagnosis and management. An upper gastrointestinal endoscopy, plain abdominal X-Ray and CT scan often helps in confirming the diagnosis and treatment modalities range from endoscopic retrieval, lithotripsy, laparoscopic procedures and when these fail, open surgery and retrieval of the obstructing stone. Here we present a 79 year old lady with multiple comorbidities along with a long standing history of cholelithiasis who developed Bouveret’s syndrome and discuss the pitfalls in diagnosis and management of this difficult and sometimes challenging condition.
Case Presentation
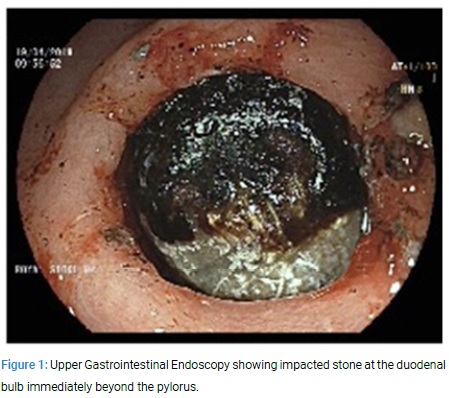
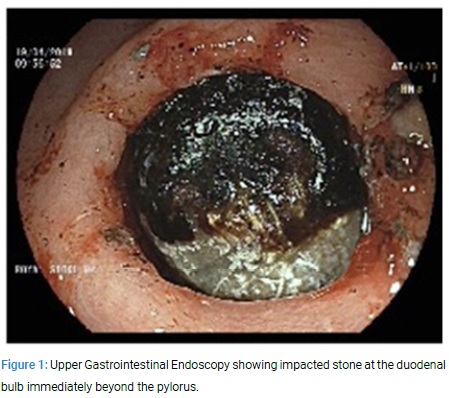
A 79 year old lady was admitted with suspected haematemesis of one day duration. She was complaining of upper abdominal pain and was dehydrated. Initial blood tests showed normal haemoglobin. After fluid resuscitation, she had an upper gastrointestinal endoscopy. This revealed low grade oesophagitis and a hard object in the duodenal bulb causing gastric outlet obstruction (Figure 1).
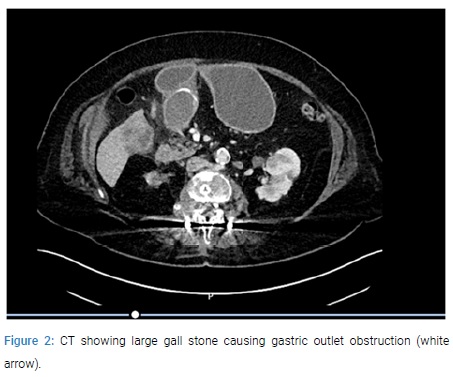
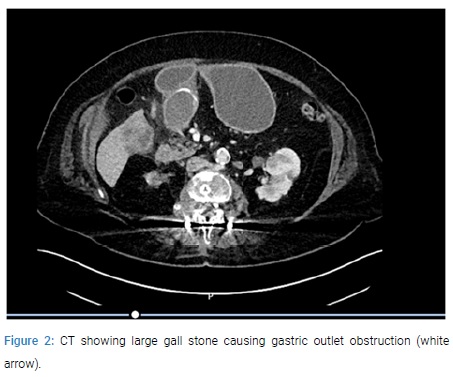
The scope could not be negotiated beyond and repeated attempts to snare it with a grasper was unsuccessful. An ultrasound examination revealed a trace of free fluid around the gall bladder with gallstones. The common bile duct was dilated to 8 mm with prominence of intra hepatic ducts in the right lobe of the liver. A CT scan revealed a 3.9 x 5.8 cm gall stone in the region of the gastric pylorus causing gastric outlet obstruction (Figure 2).
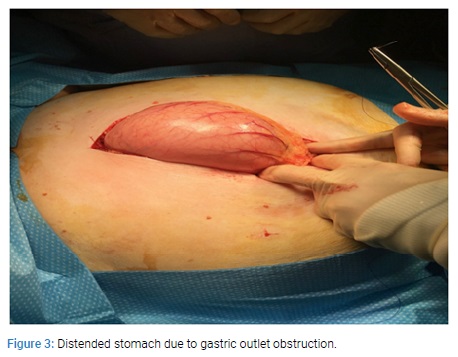
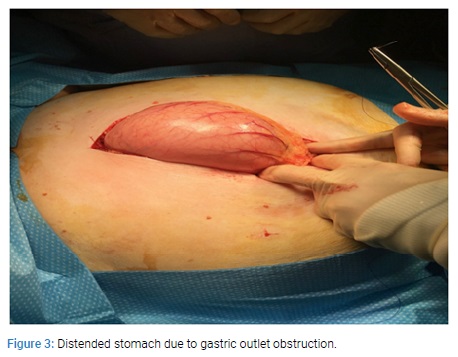
On review of her medical history, it was noted that she has been known to have gall stone disease since the last 16 years. When first diagnosed, the gallstone was 4 cm in size. In view of her comorbidities including ischemic heart disease, hypertension, Non Hodgkins lymphoma of the right kidney with infiltration to lumbar spine and psoas with pathological fractures requiring spinal fixation and chemotherapy, it was decided that conservative management is appropriate as the patient was also reluctant for surgery. Prior to this presentation, she was admitted 6 years ago with an episode of acute cholecystitis and a CT scan had shown a large obstructing calculus in the neck of the gall bladder. She was treated conservatively with antibiotics. The patient underwent laparotomy and at laparotomy, a gastrotomy was done and the stone was milked proximally from the impacted site at the duodenal bulb to the stomach and retrieved (Figure 3 and 4).

In view of her poor general condition, it was decided to leave the cholecystoduodenal fistula alone and she made a good recovery and was discharged after 10 days.
Discussion
Bilioenteric fistulae are a very rare complication of cholelithiasis occurring in less than 1% of all patients. In 60% of the cases the fistula is cholecystoduodenal. Less common variants are cholecystocolic (17%), cholecystogastric (5%) and choledochoduodenal (5%) [1-3]. Bouveret’s syndrome refers to the proximal impaction of a biliary calculus into the duodenum or the distal stomach resulting in gastric outlet obstruction in most cases. It was first described in 1770 by Beaussier. In 1896, the French physician Leon Bouveret published two cases of gastric outlet obstruction due to gallstone impaction in the duodenal bulb [4]. Bouveret’s syndrome is more prevalent in the elderly and in females, with a reported median age of 74 years and a female to male ratio of 1.9 [5,6]. It typically occurs secondary to recurrent inflammation of the gall bladder as it abuts a portion of the gastrointestinal tract, initiating the formation of a bilioenteric fistula due to the walls of the biliary system and the bowels becoming chronically inflamed and adherent. Increasing intraluminal pressure caused by obstruction leads to local ischemia and necrosis, allowing the gallstone to perforate the walls and pass into the bowel7. Stones smaller than 2.5 cm usually pass into the small bowel where they can pass uneventfully or cause gall stone ileus8.Gallstones obstructing the duodenum are usually more than 2.5?cm in size [7-9]. Risk factors for Bouveret’s syndrome include a long history of cholelithiasis, repeated episodes of biliary colic, acute cholecystitis or jaundice (60%), large stones (2-8 cm), the female gender and patients older than 60 years with significant comorbidities [10]. The clinical presentation of patients with Bouveret’s syndrome may be variable and non specific. Typical presentation involves an elderly female patient with multiple comorbidities including a history of cholelithiasis, presenting with symptoms suggestive of bowel obstruction or gastric outlet obstruction as was the case in our patient. The symptoms include abdominal pain (70%), nausea and vomiting (85%). Less common presentations include symptoms suggestive of a gastrointestinal bleed, including haematemesis (15%) and or melaena (6%) secondary to erosion of cystic, coeliac or gastro duodenal artery. Non specific signs include abdominal distension and tenderness, dehydration, fever and features of sepsis [11,12]. Differential diagnoses include perforated peptic ulcer, pancreatitis, gastric volvulus, bezoars, malignant fistula and other causes of gastric outlet obstruction such as peptic or malignant stricture [13,14]. Hence the key to making a prompt diagnosis is to have a high index of suspicion in patients with history of cholelithiasis and symptoms of gastric outlet obstruction as it is essential to institute early treatment to reduce the risk of morbidity and mortality in this sub group of elderly patients frequently with cardiovascular and general comorbidity [15,16]. Most patients have an abdominal X-ray as the initial investigation. Findings suggestive of Bouveret’s syndrome include Rigler’s triad: a dilated stomach, pneumobilia, and a radio-opaque shadow suggesting an ectopic gallstone (21%) [17]. Ultrasound may demonstrate cholelithiasis with features suggestive of cholecystitis such as gall bladder wall thickening or pericholecystic fluid [18]. Upper gastrointestinal series with oral contrast may give more insight to an obstructing mass by showing a filling defect, gallstone, dilation of the stomach or duodenum, pneumobilia, and/or outlet obstruction. In rare cases, there may be contrast extravasation into the gallbladder indicating a patent cholecystoduodenal or cholecystogastric fistula [19,20]. Majority of patients have CT scan in view of intestinal obstruction and this is helpful in diagnosing these patients as they are better in demonstrating Rigler’s triad than plain X-rays and contrast studies. They have been reported to have 93% sensitivity, 100% specificity and 99% diagnostic accuracy. CT helps in identifying the presence of a fistula, the extent of inflammation, presence of abscess and possibly the presence of the gall stone. However, 15-25% of gallstones may be missed as they are isoattenuating and hence not well visualised on CT [21,22]. MRCP can be helpful in confirming the diagnosis in such cases though the presence of air may make this difficult [23]. All patients usually undergo upper gastrointestinal endoscopy which demonstrates evidence of obstruction such as a dilated stomach with food content, bleeding stigmata such as blood clots in the stomach or duodenum, duodenal ulcer with excessive inflammation and oedema and rarely visualisation of the cholecystoduodenal fistula. However, visualisation of the obstructing gall stone is reported only in approximately two thirds of the cases. A first attempt to remove the stone during the initial endoscopy is successful only in a minority of the cases. In about 20% to 40% of all cases, the final diagnosis will only be established during surgery [4,24]. Since most patients presenting with Bouveret’s syndrome are elderly with multiple comorbidities, multiple endoscopic modalities of intervention have been reported with a view to avoid the significant morbidity and mortality associated with open surgical intervention (nearly 25-30%). These include endoscopic nets/baskets, mechanical, electrohydraulic, laser and extracorporeal shock wave lithotripsy as well as combined endoscopic and surgical therapies [25]. The first case of successful endoscopic removal of a gall stone (with a basket) located in the duodenum of a 84 year old lady with multiple comorbidities was reported by Bedogni in 1985 [26]. Following this, many case reports using nets and baskets have been published including one using a Roth net to remove a 4 cm stone lodged between the first and second part of the duodenum [27]. This is relatively simple and quick and is associated with low morbidity and mortality. However, it is ineffective in removing large stones as was the case with our patient and this may typically require another adjunct in the form of lithotripsy. Large stones that cannot be removed with an endoscopic net/basket can be crushed using mechanical lithotripsy in the stomach or proximal duodenum prior to extraction. This can be accomplished using a mechanical lithotripter and stone fragments removed endoscopically with the aid of a basket, snare or forceps [28]. It is important to remove all stone fragments to avoid the possibility of gall stone ileus [29]. Electrohydraulic lithotripsy via a dual channel gastroscope that allows continuous irrigation to enable fragmenting the stone with water immersion has been reported. The fragments were then pulled into the stomach with a snare, further fragmented with a mechanical lithotripter and removed using a Roth net. The obvious disadvantage is the risk of collateral damage to surrounding tissues including bleeding and perforation due to shock wave dispersion, which can be reduced with adequate water immersion [30]. Laser lithiotripsy including neodymium: YAG, rhodamine and holmium: YAG is advantageous over mechanical lithotripsy in that it enables precise targeting of energy on the stone thereby minimising tissue injury [31,32]. Extracorporeal shockwave lithotripsy has been reported to be successful, but problems with lack of visualisation/access and the need for further additional modes of therapy has made this treatment modality obsolete [33,34]. When endoscopic intervention is unsuccessful, then surgical options in the form of laparotomy and gastrotomy, pyloromyotomy or duodenotomy at or immediately proximal to the site of obstruction need to be consider [35]. It is usually possible to manoeuvre the impacted stone from the duodenum back into the stomach via a gastrotomy as was the case in our patient. In cases of distal duodenal impacted stone, it is possible to milk this into the proximal jejunum and remove it via an enterotomy distal to the ligament of Trietz [36]. Endoscopy with lithotripsy can be used as an adjunct to help mobilise or fragment the stone from a location which is difficult to access at open surgery into a more favourable location to perform the enterotomy [37]. Since open surgical intervention is associated with significant morbidity and mortality, laparoscopic approach should be considered if equipment and expertise is available. Enterolithotomy in the form of duodenotomy, pyloroduodenotomy and gastrotomy has been reported in literature to be safe and effective [38,39]. In both open and laparoscopic approaches, it is very important to examine the rest of the small bowel to ensure that there are no other stones in the alimentary tract that can cause potential gall stone ileus as the incidence of concurrent gall stones in other locations of the gastrointestinal tract is reported to be around 16%. The role of cholecystectomy with repair of the fistula at the time of surgical treatment of Bouveret’s syndrome is controversial [40]. Due to the poor general condition of the patient, it is argued that the benefits of this far outweigh the risks and hence is largely not done as it is reported that spontaneous fistula closure occurs in more than 50% of cases [41]. Simple stone-extraction is associated with less complications and mortality rates of 12% while the respective percentage for cholecystectomy and fistula repair is 20–30%. Since there is an increased risk of gall bladder carcinoma in patients with cholecystoenteric fistulas, repair of the fistula is recommended in younger patients.
Conclusion
Bouveret’s syndrome is a rare but potentially life threatening condition which affects <0.5% of patients with gall stones. A high index of suspicion due to non specific symptoms and investigations including CT and endoscopy is necessary to promptly diagnose and initiate management in this elderly sub group of patients with multiple comorbidities. Treatment modalities include endoscopy with adjuvants such as lithotripsy failing which surgery including a laparoscopic approach is effective. Simultaneous or subsequent cholecystectomy with repair of the fistula is usually not warranted in a majority of the cases.
Keywords
Bouveret’s syndrome; cholecystoduodenal fistula; cholelithiasis
Cite this article
Al-Saadi H, Okeke I, Mathew SS, Singh S, Shah A, Liao Y, et al. Bouveret’s syndrome – a case report and review of literature. Clin Surg J. 2020;1(2):1–5.
Copyright
© 2020 Vittal Rao. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).